Abstract
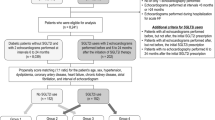
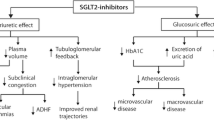
Diabetic patients frequently develop heart failure with preserved (HFpEF) or mid-range (HFmEF) cardiac ejection fractions. This condition may be secondary to diabetic cardiomyopathy or one of several relevant comorbidities, mainly hypertension. Several mechanisms link diabetes to HFpEF or HFmEF. Among these, non-enzymatic glycation of interstitial proteins, lipotoxicity, and endothelial dysfunction may promote structural damage and ultimate lead to heart failure. Findings from several large-scale trials indicated that treatment with sodium/glucose cotransporter 2 inhibitors (SGLT2-iss) resulted in significant improvements in cardiovascular outcomes in diabetic patients with high cardiovascular risk. However, there is currently some evidence that suggests a clinical advantage of using SGLT2-iss specifically in cases of HFpEF or HFmEF. Preclinical and clinical studies revealed that SGLT2-iss treatment results in a reduction in left ventricular mass and improved diastolic function. While some of the beneficial effects of SGLT2-iss have already been characterized (e.g., increased natriuresis and diuresis as well as reduced blood pressure, plasma volume, and arterial stiffness, and nephron-protective activities), there is increasing evidence suggesting that SGLT2-iss may have direct actions on the heart. These findings include SGLT2-iss-mediated reductions in the expression of hypertrophic foetal genes and diastolic myofilaments stiffness, increases in global phosphorylation of myofilament regulatory proteins (in HFpEF), inhibition of cardiac late sodium channel current and Na+/H+ exchanger activity, metabolic shifts, and effects on calcium cycling. Preliminary data from previously published studies suggest that SGLT2-iss could be useful for the treatment of HFpEF and HFmEF. Several large ongoing trials, including DELIVER AND EMPEROR -preserved have been designed to evalute the efficacy of SGLT2-iss in improving clinical outcomes in patients diagnosed with HFpEF. The goal of this manuscript is to review the use of SGLT2-iss inhibitors for HFpEF or HFmEF associated with diabetes.

Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Kenny HC, Abel ED (2019) Heart failure in type 2 diabetes mellitus. Circ Res 124:121–141. https://doi.org/10.1161/CIRCRESAHA.118.311371
Targher G, Dauriz M, Laroche C, Temporelli PL, Hassanein M, Seferovic et al (2017) ESC-HFA HF Long-Term Registry investigators. In-hospital and 1-year mortality associated with diabetes in patients with acute heart failure: results from the ESC-HFA Heart Failure Long-Term Registry. Eur J Heart Fail 19:54–65. https://doi.org/10.1002/ejhf.679
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur Heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Bozkurt B, Coats A, Tsutsui H (2021) Universal definition and classification of heart failure. J Card Fail 7:S1071–9164(21)00050–6. https://doi.org/10.1016/j.cardfail.2021.01.022
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A et al (2016) Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J 37:1526–1534. https://doi.org/10.1093/eurheartj/ehv728
Fitchett D, Inzucchi SE, Cannon CP, McGuire DK, Scirica BM, Johansen OE et al (2019) Empagliflozin reduced mortality and hospitalization for heart failure across the spectrum of cardiovascular risk in the EMPA-REG OUTCOME trial. Circulation 139:1384–1395. https://doi.org/10.1161/CIRCULATIONAHA.118.037778
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, CANVAS Program Collaborative Group et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377:644–657. https://doi.org/10.1056/NEJMoa1611925
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380:347–357. https://doi.org/10.1056/NEJMoa1812389
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U et al (2020) Cardiovascular outcomes with Ertugliflozin in type 2 diabetes. N Engl J Med 383:1425–1435. https://doi.org/10.1056/NEJMoa2004967
Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK et al (2021) Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med 384:129–139. https://doi.org/10.1056/NEJMoa2030186
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA et al (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381:1995–2008. https://doi.org/10.1056/NEJMoa1911303
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P et al (2020) Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 383:1413–1424. https://doi.org/10.1056/NEJMoa2022190
Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK et al (2021) Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med 384:117–128. https://doi.org/10.1056/NEJMoa2030183
Seferović PM, Fragasso G, Petrie M, Mullens W, Ferrari R, Thum T et al (2020) Sodium-glucose co-transporter 2 inhibitors in heart failure: beyond glycaemic control. A position paper of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 22:1495–1503. https://doi.org/10.1002/ejhf.1954
Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE et al (2007) Eur Heart J 28:2539–2550. https://doi.org/10.1093/eurheartj/ehm037
Meagher P, Adam M, Civitarese R, Bugyei-Twum A, Connelly KA (2018) Heart failure with preserved ejection fraction in diabetes: mechanisms and management. Can J Cardiol 34:632–643. https://doi.org/10.1016/j.cjca.2018.02.026
Lindman BR, Dávila-Román VG, Mann DL, McNulty S, Semigran MJ, Lewis GD et al (2014) Cardiovascular phenotype in HFpEF patients with or without diabetes: a RELAX trial ancillary study. J Am Coll Cardiol 64:541–549. https://doi.org/10.1016/j.jacc.2014.05.030
Kristensen SL, Mogensen UM, Jhund PS, Petrie MC, Preiss D, Win S et al (2017) Circulation 135:724–735. https://doi.org/10.1161/CIRCULATIONAHA.116.024593
Aguilar D, Deswal A, Ramasubbu K, Mann DL, Bozkurt B (2010) Comparison of patients with heart failure and preserved left ventricular ejection fraction among those with versus without diabetes mellitus. Am J Cardiol 105:373–377. https://doi.org/10.1016/j.amjcard.2009.09.04
MacDonald MR, Petrie MC, Varyani F, Ostergren J, Michelson EL, Young JB et al (2008) Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J 29:1377–1385. https://doi.org/10.1093/eurheartj/ehn153
Lam CS (2015) Diabetic cardiomyopathy: an expression of stage B heart failure with preserved ejection fraction. Diab Vasc Dis Res 12:234–238. https://doi.org/10.1177/1479164115579006
van Heerebeek L, Hamdani N, Handoko ML, Falcao-Pires I, Musters RJ, Kupreishvili K et al (2008) Diastolic stiffness of the failing diabetic heart: importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation 117:43–51. https://doi.org/10.1161/CIRCULATIONAHA.107.7285
Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, Grishman A (1972) New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol 30:595–602. https://doi.org/10.1016/0002-9149(72)90595-4
Kannel WB, Hjortland M, Castelli WP (1974) Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol 34:29–34. https://doi.org/10.1016/0002-9149(74)90089-7
Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS et al (2001) ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary circulation 104:2996–3007. https://doi.org/10.1161/hc4901.102568
Jia G, Hill MA, Sowers JR (2018) Diabetic cardiomyopathy: an update of mechanisms contributing to this clinical entity. Circ Res 122:624–638. https://doi.org/10.1161/CIRCRESAHA.117.311586
Miki T, Yuda S, Kouzu H, Miura T (2013) Diabetic cardiomyopathy: pathophysiology and clinical features. Heart Fail Rev 18:149–166. https://doi.org/10.1007/s10741-012-9313-3
Packer M (2021) Differential pathophysiological mechanisms in heart failure with a reduced or preserved ejection fraction in diabetes. JACC Heart Fail 9:535–549. https://doi.org/10.1016/j.jchf.2021.05.019
Anzawa R, Seki S, Nagoshi T, Taniguchi I, Feuvray D, Yoshimura M (2012) The role of Na+/H+ exchanger in Ca2+ overload and ischemic myocardial damage in hearts from type 2 diabetic db/db mice. Cardiovasc Diabetol 11(11):33. https://doi.org/10.1186/1475-2840-11-33.)
Nakamura TY, Iwata Y, Arai Y, Komamura K, Wakabayashi S (2008) Activation of Na+/H+ exchanger 1 is sufficient to generate Ca2+ signals that induce cardiac hypertrophy and heart failure. Circ Res 103:891–899. https://doi.org/10.1161/CIRCRESAHA.108.175141
Packer M (2020) Epicardial adipose tissue inflammation can cause the distinctive pattern of cardiovascular disorders seen in psoriasis. Am J Med 133:267–272. https://doi.org/10.1016/j.amjmed.2019.08.027
Fukami K, Yamagishi S, Okuda S (2014) Role of AGEs-RAGE system in cardiovascular disease. Curr Pharm Des 20:2395–2402. https://doi.org/10.2174/13816128113199990475
Hegab Z, Gibbons S, Neyses L, Mamas MA (2012) Role of advanced glycation end products in cardiovascular disease. World J Cardiol 4:90–102. https://doi.org/10.4330/wjc.v4.i4.90
Wong TC, Piehler KM, Kang IA, Kadakkal A, Kellman P, Schwartzman DS et al (2014) Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in diabetes and associated with mortality and incident heart failure admission. Eur Heart J 35:657–664. https://doi.org/10.1093/eurheartj/eht193
Bidasee KR, Nallani K, Yu Y, Cocklin RR, Zhang Y, Wang M et al (2003) Chronic diabetes increases advanced glycation end products on cardiac ryanodine receptors/calcium-release channels. Diabetes 52:1825–1836. https://doi.org/10.2337/diabetes.52.7.1825
Bidasee KR, Zhang Y, Shao CH, Wang M, Patel KP, Dincer UD, Besch HR Jr (2004) Diabetes increases formation of advanced glycation end products on Sarco(endo)plasmic reticulum Ca2+-ATPase. Diabetes 53:463–473. https://doi.org/10.2337/diabetes.53.2.463
Poornima IG, Parikh P, Shannon RP (2006) Diabetic cardiomyopathy: the search for a unifying hypothesis. Circ Res 98:596–605. https://doi.org/10.1161/01.RES.0000207406.94146.c2
Zhang DX, Fryer RM, Hsu AK, Zou AP, Gross GJ, Campbell WB, Li PL (2001) Production and metabolism of ceramide in normal and ischemic-reperfused myocardium of rats. Basic Res Cardiol 96:267–274. https://doi.org/10.1007/s003950170057
Ricciardi CA, Gnudi L (2021) Vascular growth factors as potential new treatment in cardiorenal syndrome in diabetes. Eur J Clin Invest 3:e13579. https://doi.org/10.1111/eci.1357
Natali A, Nesti L, Fabiani I, Calogero E, Di Bello V (2017) Impact of empagliflozin on subclinical left ventricular dysfunctions and on the mechanisms involved in myocardial disease progression in type 2 diabetes: rationale and design of the EMPA-HEART trial. Cardiovasc Diabetol 16:130. https://doi.org/10.1186/s12933-017-0615-6
Hammoudi N, Jeong D, Singh R, Farhat A, Komajda M, Mayoux E et al (2017) Empagliflozin improves left ventricular diastolic dysfunction in a genetic model of type 2 diabetes. Cardiovasc Drugs Ther 3:233–246. https://doi.org/10.1007/s10557-017-6734-1
Verma S, Mazer CD, Yan AT, Mason T, Garg V, Teoh H et al (2019) Effect of empagliflozin on left ventricular mass in patients with type 2 diabetes mellitus and coronary artery disease: the EMPA-HEART CardioLink-6 randomized clinical trial. Circulation 140:1693–1702. https://doi.org/10.1161/CIRCULATIONAHA.119.042375
Mason T, Coelho-Filho OR, Verma S, Chowdhury B, Zuo F, Quan A et al (2021) Empagliflozin reduces myocardial extracellular volume in patients with type 2 diabetes and coronary artery disease. JACC Cardiovasc Imaging 14:1164–1173. https://doi.org/10.1016/j.jcmg.2020.10.017
Li J, Woodward M, Perkovic V, Figtree GA, Heerspink HJL, Mahaffey KW et al (2020) Mediators of the effects of Canagliflozin on heart failure in patients with type 2 diabetes. JACC Heart Fail 8:57–66. https://doi.org/10.1016/j.jchf.2019.08.004
Williams DM, Nawaz A, Evans M (2020) Renal outcomes in type 2 diabetes: a review of cardiovascular and renal outcome trials. Diabetes Ther 11:369–386. https://doi.org/10.1007/s13300-019-00747-3
Uthman L, Baartscheer A, Schumacher CA, Fiolet JWT, Kuschma MC, Hollmann MW et al (2018) Direct cardiac actions of sodium glucose cotransporter 2 inhibitors target pathogenic mechanisms underlying heart failure in diabetic patients. Front Physiol 9:1575. https://doi.org/10.3389/fphys.2018.0157
Di Franco A, Cantini G, Tani A, Coppini R, Zecchi-Orlandini S, Raimondi L et al (2017) Int J Cardiol 243:86–90. https://doi.org/10.1016/j.ijcard.2017.05.032
Byrne NJ, Parajuli N, Levasseur JL, Boisvenue J, Beker DL, Masson G et al (2017) Empagliflozin prevents worsening of cardiac function in an experimental model of pressure overload-induced heart failure. JACC Basic Transl Sci 2:347–354. https://doi.org/10.1016/j.jacbts.2017.07.003
Pabel S, Wagner S, Bollenberg H, Bengel P, Kovács Á, Schach C et al (2018) Empagliflozin directly improves diastolic function in human heart failure. Eur J Heart Fail 20:1690–1700. https://doi.org/10.1002/ejhf.1328
Byrne NJ, Matsumura N, Maayah ZH, Ferdaoussi M, Takahara S, Darwesh AM et al (2020) Empagliflozin blunts worsening cardiac dysfunction associated with reduced NLRP3 (nucleotide-binding domain-like receptor protein 3) inflammasome activation in heart failure. Circ Heart Fail 13:e006277. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006277
Philippaert K, Kalyaanamoorthy S, Fatehi M, Long W, Soni S, Byrne NJ, Barr A et al (2021) Circulation 143:2188–2204. https://doi.org/10.1161/CIRCULATIONAHA.121.053350
Makielski JC (2016) Trends Cardiovasc Med 26:115–122. https://doi.org/10.1016/j.tcm.2015.05.006
Uthman L, Baartscheer A, Bleijlevens B, Schumacher CA, Fiolet JWT, Koeman A et al (2018) Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na+/H+ exchanger, lowering of cytosolic Na+ and vasodilation. Diabetologia 61:722–726. https://doi.org/10.1007/s00125-017-4509-7
Trum M, Riechel J, Lebek S, Pabel S, Sossalla ST, Hirt S (2020) ESC Heart Fail 7:4429–4437. https://doi.org/10.1002/ehf2.13024
Díaz-Rodríguez E, Agra RM, Fernández ÁL, Adrio B, García-Caballero T et al (2018) S.Effects of dapagliflozin on human epicardial adipose tissue: modulation of insulin resistance, inflammatory chemokine production, and differentiation ability. Cardiovasc Res 114:336–346. https://doi.org/10.1093/cvr/cvx186
Ferrannini E, Mark M, Mayoux E (2016) CV Protection in the EMPA-REG OUTCOME ttrial: a “thrifty substrate” hypothesis. Diabetes Care 39:1108–1114. https://doi.org/10.2337/dc16-0330
Becher PM, Schrage B, Ferrannini G, Benson L, Butler J, Carrero JJ et al (2021) Use of sodium-glucose co-transporter 2 inhibitors in patients with heart failure and type 2 diabetes mellitus: data from the Swedish Heart Failure Registry. Eur J Heart Fail 23:1012–1022. https://doi.org/10.1002/ejhf.2131
Abraham WT, Lindenfeld J, Ponikowski P, Agostoni P, Butler J, Desai AS et al (2021) Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes. Eur Heart J 42:700–710. https://doi.org/10.1093/eurheartj/ehaa943
Rådholm K, Figtree G, Perkovic V, Solomon SD, Mahaffey KW, de Zeeuw D et al (2018) Circulation 138:458–468. https://doi.org/10.1161/CIRCULATIONAHA.118.034222
Sarraju A, Li J, Cannon CP, Chang TI, Agarwal R, Bakris G et al (2021) Effects of canagliflozin on cardiovascular, renal, and safety outcomes in participants with type 2 diabetes and chronic kidney disease according to history of heart failure: Results from the CREDENCE trial. Am Heart 233:141–148. https://doi.org/10.1016/j.ahj.2020.12.008
Kato ET, Silverman MG, Mosenzon O, Zelniker TA, Cahn A, Furtado RHM et al (2019) Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation 139:2528–2536. https://doi.org/10.1161/CIRCULATIONAHA.119.040130
Cosentino F, Cannon CP, Cherney DZI, Masiukiewicz U, Pratley R, Dagogo-Jack S et al (2020) Efficacy of ertugliflozin on heart failure-related events in patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease: results of the VERTIS CV trial. Circulation 142:2205–2215. https://doi.org/10.1161/CIRCULATIONAHA.120.05025
CONSENSUS Trial Study Group (1987) Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 316:1429–1435. https://doi.org/10.1056/NEJM198706043162301
Singh AK, Singh R, Misra A (2021) Do SGLT-2 inhibitors exhibit similar cardiovascular benefit in patients with heart failure with reduced or preserved ejection fraction? J Diabetes 13:596–600. https://doi.org/10.1111/1753-0407.13182
Anker SD, Butler J, Filippatos GS, Jamal W, Salsali A, Schnee J et al (2019) Evaluation of the effects of sodium-glucose co-transporter 2 inhibition with empagliflozin on morbidity and mortality in patients with chronic heart failure and a preserved ejection fraction: rationale for and design of the EMPEROR-Preserved Trial. Eur J Heart Fail 21:1279–1287. https://doi.org/10.1002/ejhf.1596
Anker SD, Butler J, Filippatos G, Shahzeb KM, Ferreira JP et al (2020) Baseline characteristics of patients with heart failure with preserved ejection fraction in the EMPEROR-Preserved trial. Eur J Heart Fail 22:2383–2392. https://doi.org/10.1002/ejhf.2064
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. Online ahead of print. https://doi.org/10.1056/NEJMoa2107038
https://clinicaltrials.gov/ct2/results?cond=heart+failure+preserved&term=sglt2&cntry=&state=&city=&dist=. Accessed 16 July 2021
Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN et al (2021) Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial Eur J Heart Fail May 29. Online ahead of print. https://doi.org/10.1002/ejhf.2249
Author information
Authors and Affiliations
Contributions
AP, CR, AlP, and DS contributed to the conception and design of the review. AP and CR wrote sections of the manuscript. All authors contributed to manuscript revision and read and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Passantino, A., Rizzo, C., Scrutinio, D. et al. Diabetes and SGLT2-iss inhibitors in patients with heart failure with preserved or mid-range left ventricular ejection fractions. Heart Fail Rev 28, 683–695 (2023). https://doi.org/10.1007/s10741-021-10186-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10186-7