Abstract
Purpose
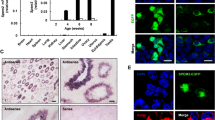
Sperm DNA fragmentation has been suggested as a marker for infertility diagnosis and prognosis. Hence, understanding its impact on male physiology and post-genomic pathways would be clinically important. We performed the proteomics and functional enrichment analyses of viable spermatozoa from ejaculates with low and high sperm DNA fragmentation to identify protein expression and pathways altered in association with sperm DNA fragmentation.
Methods
Sperm DNA fragmentation using the Comet assay and the Komet 6.0.1 software was assessed in raw samples from 89 subjects from a human reproduction service. The Low and High sperm DNA fragmentation groups were formed according to the Olive Tail Moment variable. Spermatozoa proteins from these groups were pooled and analyzed by a shotgun proteomic approach (2D nanoUPLC-ESI-MSE). Differentially expressed proteins were used for a functional enrichment study.
Results
Two hundred and fifty-seven proteins were identified or quantified in sperm from the Low and High sperm DNA fragmentation groups. Of these, seventy-one proteins were exclusively or overexpressed in the Low group, whereas twenty-three proteins were exclusively or overexpressed in the High group. One hundred and sixty-three proteins were conserved between these groups. We also functionally related the differentially expressed proteins in viable spermatozoa from the groups. Processes such as triacylglycerol metabolism, energy production, protein folding, response to unfolded proteins, and cellular detoxification were found to be altered in these cells.
Conclusions
Sperm DNA fragmentation is associated with differential protein expression in viable spermatozoa. These proteins may potentially be used as biomarkers for sperm DNA integrity.




Similar content being viewed by others
References
Brugh VM, Lipshultz LI. Male factor infertility: evaluation and management. Med Clin North Am. 2004;88:367–85.
Avendaño C, Franchi A, Taylor S, Morshedi M, Bocca S, Oehninger S. Fragmentation of DNA in morphologically normal human spermatozoa. Fertil Steril. 2009;91(4):1077–84.
Saleh RA, Agarwal A, Nada EA, EI-Tonsy MH, Sharma RK, Meyer A, et al. Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility. Fertil Steril. 2003;79(S3):1597–605.
Balhorn R, Cosman M, Thornton K, Krishnan VV, Corzett M, Bench G, et al. Protamine mediated condensation of DNA in mammalian sperm. In: Gagnon C, editor. The male gamete: From basic science to clinical applications. Vienna: Cache River Press; 1999. p. 55–70.
Barroso G, Morshedi M, Oehninger S. Analysis of DNA fragmentation, plasma membrane translocation of phosphatidylserine and oxidative stress in human spermatozoa. Hum Reprod. 2000;15:1338–44.
Sakkas D, Moffatt O, Manicardi GC, Mariethoz E, Tarozzi N, Bizzaro D. Nature of DNA damage in ejaculated human spermatozoa and the possible involvement of apoptosis. Biol Reprod. 2003;66:1061–7.
Sakkas D, Mariethoz E, St John JC. Abnormal sperm parameters in humans are indicative of an abortive apoptotic mechanism linked to the Fas-mediated pathway. Exp Cell Res. 1999;251(2):350–5.
O’Brien J, Zini A. Sperm DNA integrity and male infertility. Urology. 2005;65:16–22.
Benchaib M, Braun V, Lornage J, Hadj S, Salle B, Lejeune H, et al. Sperm DNA fragmentation decreases the pregnancy rate in an assisted reproductive technique. Hum Reprod. 2003;18(5):1023–8.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22:174–9.
Loft S, Kold-Jensen T, Hjollund NH, Giwercman A, Gyllemborg J, Ernst E, et al. Oxidative DNA damage in human sperm influences time to pregnancy. Hum Reprod. 2003;18:1265–72.
Shamsi MB, Kumar R, Dada R. Evaluation of nuclear DNA damage in human spermatozoa in men opting for assisted reproduction. Indian J Med Res. 2008;127:115–23.
Tomsu M, Sharma V, Miller D. Embryo quality and IVF treatment outcomes may correlate with different sperm comet assay parameters. Hum Reprod. 2002;17(7):1856–62.
Borini A, Tarozzi N, Bizzaro D, Bonu MA, Fava L, Flamigni C, et al. Sperm DNA fragmentation: paternal effect on early post-implantation embryo development in ART. Hum Reprod. 2006;21(11):2876–81.
Seli E, Gardner DK, Schoolcraft WB, Moffatt O, Sakkas D. Extent of nuclear DNA damage in ejaculated spermatozoa impacts on blastocyst development after in vitro fertilization. Fertil Steril. 2004;82:378–83.
Practice Committee of American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2012;98(2):294–301.
Evenson DP, Darzynkiewicz Z, Melamed MR. Relation of mammalian sperm chromatin heterogeneity to fertility. Science. 1980;210:1131–3.
Spano M, Bonde JP, Hjollund HI, Kolstad HA, Cordelli E, Leter G. Sperm chromatin damage impairs human fertility. Fertil Steril. 2000;73:43–50.
Zini A, Sigman M. Are tests of sperm DNA damage clinically useful? pros and cons. J Androl. 2009;30(3):219–29.
Huszar G, Patrizio P, Vigue L, Willets M, Wilker C, Adhoot D, et al. Cytoplasmic extrusion and the switch from creatine kinase B to M isoform are completed by the commencement of epididymal transport in human and stallion spermatozoa. J Androl. 1998;19(1):11–20.
Sakkas D. Novel technologies for selecting the best sperm for in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2013. doi:10.1016/j.fertnstert.2012.12.025.
Sharpe RM. Regulation of Spermatogenesis. In: Knobil E, Neil JD, editors. The physiology of reproduction. 2nd ed. New York: Raven Press, Ltd.; 1994. p. 1363–434.
Shen HM, Dai J, Chia SE, Lim A, Ong CN. Detection of apoptotic alterations in sperm in subfertile patients and their correlations with sperm quality. Hum Reprod. 2002;17(5):1266–73.
González-Marín C, Gosálvez J, Roy R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int J Mol Sci. 2012;13(11):14026–52.
McVicar CM, McClure N, Williamson K, Dalzell LH, Lewis SE. Incidence of Fas positivity and deoxyribonucleic acid double-stranded breaks in human ejaculated sperm. Fertil Steril. 2004;81 Suppl 1:767–74.
Dacheux JL, Voglmayr JK. Sequence of sperm cell surface differentiation and its relationship to exogenous fluid proteins in the ram epididymis. Biol Reprod. 1983;29:1033–46.
WHO (World Health Organization). Laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 5th ed. New York: Cambridge University Press; 2010.
Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, van Zyl JA, et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril. 1986;46:1118–23.
Fariello RM, Del Giudice PT, Spaine DM, Fraietta R, Bertolla RP, Cedenho AP. Effect of leukocytospermia and processing by discontinuous density gradient on sperm nuclear DNA fragmentation and mitochondrial activity. J Assist Reprod Genet. 2009;26:151–7.
Mozaffarieh M, Schoetzau A, Sauter M, Grieshaber M, Orgül S, Golubnitschaja O, et al. Comet assay analysis of single-stranded DNA breaks in circulating leukocytes of glaucoma patients. Mol Vis. 2008;14:1584–8.
Camargo M, Intasqui Lopes P, Del Giudice PT, Carvalho VM, Cardozo KH, Andreoni C, et al. Unbiased label-free quantitative proteomic profiling and enriched proteomic pathways in seminal plasma of adult men before and after varicocelectomy. Hum Reprod. 2013;28(1):33–46.
Intasqui P, Camargo M, Del Giudice PT, Spaine DM, Carvalho VM, Cardozo KHM, Zylbersztejn DS, Bertolla RP (2013) Sperm nuclear DNA fragmentation rate is associated with differential protein expression and enriched functions in human seminal plasma. BJU Int
Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, et al. Measurement of protein using bicinchoninic acid. Anal Biochem. 1985;150:76–85.
Cho CK, Smith CR, Diamandis EP. Amniotic fluid proteome analysis from down syndrome pregnancies for biomarker discovery. J Proteome Res. 2010;9(7):3574–82.
Pan S, Chen R, Crispin DA, May D, Stevens T, McIntosh MW, et al. Protein alterations associated with pancreatic cancer and chronic pancreatitis found in human plasma using global quantitative proteomics profiling. J Proteome Res. 2011;10(5):2359–576.
Smoot ME, Ono K, Ruscheinski J, Wang PL, Ideker T. Cytoscape 2.8: new features for data integration and network visualization. Bioinformatics. 2011;27(3):431–2.
Martin A, Ochagavia ME, Rabasa LC, Miranda J, Fernandez-de-Cossio J, Bringas R. A new tool for gene network building, visualization and analysis. BMC Bioinforma. 2010;11:91.
da Huang W, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37(1):1–13.
Quackenbush J. Extracting biology from high-dimensional biological data. J Exp Biol. 2007;210:1507–17.
Kovac JR, Pastuszak AW, Lamb DJ. The use of genomics, proteomics, and metabolomics in identifying biomarkers of male infertility. Fertil Steril. 2013. doi:10.1016/j.fertnstert.2013.01.111.
Agarwal A, Sharma RK, Nallella KP, Thomas AJ, Alvarez JG, Sikka SC. Reactive oxygen species as an independent marker of male factor infertility. Fertil Steril. 2006;86(4):878–85.
Baltz JM, Williams PO, Cone RA. Dense fibers protect mammalian sperm against damage. Biol Reprod. 1990;43:485–91.
Haidl G, Becker A, Henkel R. Poor development of outer dense fibers as a major cause of tail abnormalities in the spermatozoa of asthenoteratozoospermic men. Hum Reprod. 1991;6:1431–8.
Shao X, Murthy S, Demetrick DJ, van der Hoorn FA. Human outer dense fiber gene, ODF2, localizes to chromosome 9q34. Cytogenet Cell Genet. 1998;83(3–4):221–3.
Pixton KL, Deeks ED, Flesch FM, Moseley FL, Björndahl L, Ashton PR, et al. Sperm proteome mapping of a patient who experienced failed fertilization at IVF reveals altered expression of at least 20 proteins compared with fertile donors: case report. Hum Reprod. 2004;19:1438–47.
Aitken RJ, Baker MA. The role of proteomics in understanding sperm cell biology. Int JAndrol. 2008;31:295–302.
Fontaine JM, Rest JS, Welsh MJ, Benndorf R. The sperm outer dense fiber protein is the 10th member of the superfamily of mammalian small stress proteins. Cell Stress Chaperones. 2003;8(1):62–9.
Arrigo AP, Paul C, Ducasse C, Sauvageot O, Kretz-Remy C. Small stress proteins: modulation of intracellular redox state and protection against oxidative stress. Prog Mol Subcell Biol. 2002;28:171–84.
Arrigo AP, Paul C, Ducasse C, Manero F, Kretz-Remy C, Virot S, et al. Small stress proteins: novel negative modulators of apoptosis induced independently of reactive oxygen species. Prog Mol Subcell Biol. 2002;28:185–204.
Haslbeck M, Buchner J. Chaperone function of sHsps. Prog Mol Subcell Biol. 2002;28:37–59.
Gene Ontology (GO:0050821), http://amigo.geneontology.org/cgi-bin/amigo/term_details?term=GO:0050821&session_id=5683amigo1336408572
Nagamori I, Yabuta N, Fujii T, Tanaka H, Yomogida K, Nishimune Y, et al. Tisp40, a spermatid specific bZip transcription factor, functions by binding to the unfolded protein response element via the Rip pathway. Genes Cells. 2005;10(6):575–94.
Eddy EM. Role of heat shock protein HSP70-2 in spermatogenesis. Rev Reprod. 1999;4:23–30.
Redgrove KA, Nixon B, Baker MA, Hetherington L, Baker G, Liu DY, et al. The molecular chaperone HSPA2 plays a key role in regulating the expression of sperm surface receptors that mediate sperm-egg recognition. PLoS One. 2012;7:e50851.
Lima SB, Cenedeze MA, Bertolla RP, Filho PA, Oehninger S, Cedenho AP. Expression of the HSPA2 gene in ejaculated spermatozoa from adolescents with and without varicocele. Fertil Steril. 2006;86(6):1659–963.
Tesarik J, Greco E, Mendoza C. Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum Reprod. 2004;19(3):611–5.
Miki K, Willis WD, Brown PR, Goulding EH, Fulcher KD, Eddy EM. Targeted disruption of the Akap4 gene causes defects in sperm flagellum and motility. Dev Biol. 2002;248(2):331–42.
Batruch I, Lecker I, Kagedan D, Smith CR, Mullen BJ, Grober E, et al. Proteomic analysis of seminal plasma from normal volunteers and post-vasectomy patients identifies over 2000 proteins and candidate biomarkers of the urogenital system. J Proteome Res. 2011;10(3):941–53.
Cross NL, Mahasreshti P. Prostasome fraction of human seminal plasma prevents sperm from becoming acrosomally responsive to the agonist progesterone. Arch Androl. 1997;39(1):39–44.
Park KH, Kim BJ, Kang J, Nam TS, Lim JM, Kim HT, Park JK, Kim YG, Chae SW, Kim UH (2011) Ca2+ signaling tools acquired from prostasomes are required for progesterone-induced sperm motility. Sci Signal 17;4(173):ra31
Pons-Rejraji H, Artonne C, Sion B, Brugnon F, Canis M, Janny L, et al. Prostasomes: inhibitors of capacitation and modulators of cellular signalling in human sperm. Int J Androl. 2011;34:568–80.
Saez F, Motta C, Boucher D, Grizard G. Antioxidant capacity of prostasomes in human semen. Mol Hum Reprod. 1998;4:667–72.
Ronquist KG, Ek B, Stavreus-Evers A, Larsson A, Ronquist G (2013) Human prostasomes express glycolytic enzymes with capacity for ATP production. Am J Physiol Endocrinol Metab
Albarracín JL, Fernández-Novell JM, Ballester J, Rauch MC, Quintero-Moreno A, Peña A, et al. Gluconeogenesis-linked glycogen metabolism is important in the achievement of in vitro capacitation of dog spermatozoa in a medium without glucose. Biol Reprod. 2004;71(5):1437–45.
Mukai C, Okuno M. Glycolysis plays a major role for adenosine triphosphate supplementation in mouse sperm flagellar movement. Biol Reprod. 2004;71(2):540–7.
Marin S, Chiang K, Bassilian S, Lee WNP, Boros LG, Fernández-Novell JM, et al. Metabolic strategy of boar spermatozoa revealed by a metabolomic characterization. FEBS Lett. 2003;554:342–6.
Mahadevan MM, Miller MM, Moutos DM. Absence of glucose decreases human fertilization and sperm movement characteristics in vitro. Hum Reprod. 1997;12:119–23.
Williams AC, Ford WCL. The role of glucose in supporting motility and capacitation in human spermatozoa. J Androl. 2001;22(4):680–95.
Rogers BJ, Perreault SD. Importance of glycolysable substrates for in vitro capacitation of human spermatozoa. Biol Reprod. 1990;43:1064–9.
Argov N, Sklan D, Zeron Y, Roth Z. Association between seasonal changes in fatty-acid composition, expression of VLDL receptor and bovine sperm quality. Theriogenology. 2007;67:878–85.
Beer-Ljubic B, Aladrovic J, Marenjak TS, Laskaj R, Majic-Balic I, Milinkovic-Tur S. Cholesterol concentration in seminal plasma as a predictive tool for quality semen evaluation. Theriogenology. 2009;72:1132–40.
Amaral A, Castillo J, Estanyol JM, Ballescà JL, Ramalho-Santos J, Oliva R. Human sperm tail proteome suggests new endogenous metabolic pathways. Mol Cell Proteomics. 2013;12(2):330–42.
Miki K, Qu W, Goulding EH, Willis WD, Bunch DO, Strader LF, et al. Glyceraldehyde 3-phosphate dehydrogenase-S, a sperm-specific glycolytic enzyme, is required for sperm motility and male fertility. Proc Natl Acad Sci. 2004;101(47):16501–6.
Spiropoulos J, Turnbull DM, Chinnery PF. Can mitochondrial DNA mutations cause sperm dysfunction? Mol Hum Reprod. 2002;8:719–21.
Nakada K, Sato A, Yoshida K, Morita T, Tanaka H, Inoue S, Yonekawa H, Hayashi J (2006) Mitochondria-related male infertility. Proc Natl Acad Sci USA 10;103(41):15148–15153
Stendardi A, Focarelli R, Piomboni P, Palumberi D, Serafini F, Ferramosca A, et al. Evaluation of mitochondrial respiratory efficiency during in vitro capacitation of human spermatozoa. Int J Androl. 2011;34(3):247–55.
Ruiz-Pesini E, Diez C, Lapeña AC, Pérez-Martos A, Montoya J, Alvarez E, et al. Correlation of sperm motility with mitochondrial enzymatic activities. Clin Chem. 1998;44(8Pt1):1616–20.
Narisawa S, Hecht NB, Goldberg E, Boatright KM, Reed JC, Millán JL. Testis-specific cytochrome c-null mice produce functional sperm but undergo early testicular atrophy. Mol Cell Biol. 2002;15:5554–62.
Ferramosca A, Focarelli R, Piomboni P, Coppola L, Zara V. Oxygen uptake by mitochondria in demembranated human spermatozoa: a reliable tool for the evaluation of sperm respiratory efficiency. Int J Androl. 2008;31(3):337–45.
UniProt Entry Q8TDB8, http://www.uniprot.org/uniprot/Q8TDB8
Wang X, Sharma RK, Gupta A, George V, Thomas AJ, Falcone T, et al. Alterations in mitochondria membrane potential and oxidative stress in infertile men: a prospective observational study. Fertil Steril. 2003;80:844–50.
Bergamo P, Balestrieri M, Cammarota G, Guardiola J, Abrescia P. CD4-mediated anchoring of the seminal antigen gp17 onto the spermatozoon surface. Hum Immunol. 1997;58:30–41.
Thacker S, Yadav SP, Sharma RK, Kashou A, Willard B, Zhang D, Agarwal A (2011) Evaluation of sperm proteins in infertile men: a proteomic approach. Fertil Steril 30;95(8):2745–2748
Ma T, Keller JA, Yu X. RNF8-dependent histone ubiquitination during DNA damage response and spermatogenesis. Acta Biochim Biophys Sin. 2011;43(5):339–45.
Chakravarty S, Bansal P, Sutovsky P, Gupta SK. Role of proteasomal activity in the induction of acrosomal exocytosis in human spermatozoa. Reprod Biomed Online. 2008;16:391–400.
Kong M, Diaz ES, Morales P. Participation of the human sperm proteasome in the capacitation process and its regulation by protein kinase A and tyrosine kinase. Biol Reprod. 2009;80(5):1026–35.
Yi YJ, Zimmerman SW, Manandhar G, Odhiambo JF, Kennedy C, Jonáková V, et al. Ubiquitin-activating enzyme (UBA1) is required for sperm capacitation, acrosomal exocytosis and sperm-egg coat penetration during porcine fertilization. Int J Androl. 2012;35(2):196–210.
Sutovsky P, Moreno R, Ramalho-Santos J, Dominko T, Thompson WE, Schatten G. A putative, ubiquitin-dependent mechanism for the recognition and elimination of defective spermatozoa in the mammalian epididymis. J Cell Sci. 2001;114:1665–75.
Yoshida H, Matsui T, Hosokawa N, Kaufman JR, Nagata K, Mori K. A time-dependent phase shift in the mammalian unfolded protein response. Dev Cell. 2003;4:265–71.
Sylvester SR, Morales C, Oko R, Griswold MD. Localization of sulfated glycoprotein-2 (clusterin) on spermatozoa and in the reproductive tract of the male rat. Biol Reprod. 1991;45:195–207.
Buttyan R, Olsson CA, Pintar J, Chang C, Bandyk M, Ng PY, et al. Induction of the TRPM-2 gene in cells undergoing programmed death. Mol Cell Biol. 1989;9:3473–81.
Fritz IB, Burdzy K, Setchell B, Blaschuk O. Ram rete testis fluid contains a protein (clusterin) which influences cell-cell interaction in vitro. Biol Reprod. 1983;28:1173–88.
Murphy BF, Kirszbaum L, Walker ID, d’Apice AJ. SP-40, 40, a newly identified normal human serum protein found in the SC5b-9 complex of complement and in the immune deposits in glomerulonephritis. J Clin Invest. 1988;81:1858–64.
Jenne DE, Lowin B, Peitsch MC, Böttcher A, Schmitz G, Tschopp J. Clusterin (complement lysis inhibitor) forms a high density lipoprotein complex with apolipoprotein A-I in human plasma. J Biol Chem. 1991;266:11030–6.
Ibrahim NM, Gilbert GR, Loseth KL, Crabo BG. Correlation between clusterin-positive spermatozoa determined by flow cytometry in bull semen and fertility. J Androl. 2000;21:887–94.
O’Bryan MK, Murphy BF, Liu DY, Clarke GN, Baker HW. The use of anticlusterin monoclonal antibodies for the combined assessment of human sperm morphology and acrosome integrity. Hum Reprod. 1994;9:1490–6.
Novak S, Smith TA, Paradis F, Burwash L, Dyck MK, Foxcroft GR, et al. Biomarkers of in vivo fertility in sperm and seminal plasma of fertile stallions. Theriogenology. 2010;74:956–67.
Huleihel M, Lunenfeld E, Horowitz S, Levy A, Potashnik G, Glezerman M. Production of interleukin-1-like molecules by human sperm cells. Fertil Steril. 2000;73(6):1132–7.
Austgulen R, Arntzen KJ, Vatten LJ, Kahn J, Sunde A. Detection of cytokines (interleukin-1, interleukin-6, transforming growth factor-beta) and soluble tumor necrosis factor receptors in embryo culture fluids during in-vitro fertilization. Hum Reprod. 1995;10(1):171–6.
Cheng EH, Sheiko TV, Fisher JK, Craigen WJ, Korsmeyer SJ. VDAC2 inhibits BAK activation and mitochondrial apoptosis. Science. 2003;301(5632):513–7.
Liu B, Wang P, Wang Z, Jia Y, Niu X, Wang W, et al. Analysis and difference of voltage-dependent anion channel mRNA in ejaculated spermatozoa from normozoospermic fertile donors and infertile patients with idiopathic asthenozoospermia. J Assist Reprod Genet. 2010;27:719–24.
Hinsch K-D, De Pinto V, Aires VA, Schneider X, Messina A, Hinsch E. Voltage-dependent anion-selective channels VDAC2 and VDAC3 are abundant proteins in bovine outer dense fibers, a cytoskeletal component of the sperm flagellum. J Biol Chem. 2004;279(15):15281–8.
Alvarez JG, Storey BT. Role of glutathione peroxidase in protecting mammalian spermatozoa from loss of motility caused by spontaneous lipid peroxidation. Gamete Res. 1989;23:77–90.
Colagar AH, Marzony ET. Ascorbic Acid in human seminal plasma: determination and its relationship to sperm quality. J Clin Biochem Nutr. 2009;45:144–9.
Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003;79:829–43.
Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996;48:835–50.
Ichikawa T, Oeda T, Ohmori H, Schill W-B. Reactive oxygen species influence the acrosome reaction but not acrosin activity in human spermatozoa. International J Androl. 1999;22:37–42.
Tremellen K. Oxidative stress and male infertility – a clinical perspective. Hum Reprod Update. 2008;14:243–58.
Lin YN, Roy A, Yan W, Burns KH, Matzuk MM. Loss of zona pellucida binding proteins in the acrosomal matrix disrupts acrosome biogenesis and sperm morphogenesis. Mol Cell Biol. 2007;27(19):6794–805.
Nixon B, Aitken RJ, McLaughlin EA. New insights into the molecular mechanisms of sperm–egg interaction. Cell Mol Life Sci. 2007;64:1805–23.
Diamandis EP, Arnett WP, Foussias G, Pappas H, Ghandi S, Melegos DN, et al. Seminal plasma biochemical markers and their association with semen analysis findings. Urology. 1999;53(3):596–603.
Szecsi PB, Dalgaard D, Stakemann G, Wagner G, Foltmann B. T he concentration of pepsinogen C in human semen and the physiological activation of zymogen in the vagina. Biol Reprod. 1989;40(3):653–9.
Acknowledgements
The authors wish to thank Fleury/Finep for research funding and financial support. Ms. Intasqui was recipient of a scholarship from the Fundação de Amparo à Pesquisa no Estado de Sao Paulo (FAPESP process number 2011/00385-4).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Sperm DNA fragmentation is associated with differential protein expression and biological functions in viable sperm. These proteins may be potentially used as biomarkers for sperm DNA integrity.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 251 kb)
Rights and permissions
About this article
Cite this article
Intasqui, P., Camargo, M., Del Giudice, P.T. et al. Unraveling the sperm proteome and post-genomic pathways associated with sperm nuclear DNA fragmentation. J Assist Reprod Genet 30, 1187–1202 (2013). https://doi.org/10.1007/s10815-013-0054-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0054-6