Abstract
Newborn screening efforts focusing on the quantification of T cell receptor excision circles (TRECs), as a biomarker for abnormal thymic production of T cells, have allowed for the identification and definitive treatment of severe combined immunodeficiency (SCID) in asymptomatic neonates. With the adoption of TREC quantification in Guthrie cards across the USA and abroad, typical, and atypical SCID constitutes only ~ 10% of cases identified with abnormal TRECs associated with T cell lymphopenia. Several other non-SCID-related conditions may be identified by newborn screening in a term infant. Thus, it is important for physicians to recognize that other factors, such as prematurity, are often associated with low TRECs initially, but often improve with age. This paper focuses on a challenge that immunologists face: the diagnostic evaluation and management of cases in which abnormal TRECs are associated with variants of T cell lymphopenia in the absence of a genetically defined form of typical or atypical SCID. Various syndromes associated with T cell impairment, secondary forms of T cell lymphopenia, and idiopathic T cell lymphopenia are identified using this screening approach. Yet there is no consensus or guidelines to assist in the evaluation and management of these newborns, despite representing 90% of the patients identified, resulting in significant work for the clinical teams until a diagnosis is made. Using a case-based approach, we review pearls relevant to the evaluation of these newborns, as well as the management dilemmas for the families and team related to the resolution of genetic ambiguities.
Similar content being viewed by others
References
Chinn IK, Shearer WT. Severe combined immunodeficiency disorders. Immunol Allergy Clin N Am. 2015;35(4):671–94.
Puck JM. Newborn screening for severe combined immunodeficiency and T-cell lymphopenia. Immunol Rev. 2019;287(1):241–52.
van der Burg M, Mahlaoui N, Gaspar HB, Pai SY. Universal newborn screening for severe combined immunodeficiency (SCID). Front Pediatr. 2019;7:373.
Bifsha P, Leiding JW, Pai SY, Colamartino ABL, Hartog N, Church JA, et al. Diagnostic assay to assist clinical decisions for unclassified severe combined immune deficiency. Blood Adv. 2020;4(12):2606–10.
Bosticardo M, Pala F, Calzoni E, Delmonte OM, Dobbs K, Gardner CL, et al. Artificial thymic organoids represent a reliable tool to study T-cell differentiation in patients with severe T-cell lymphopenia. Blood Adv. 2020;4(12):2611–6.
Amatuni GS, Currier RJ, Church JA, Bishop T, Grimbacher E, Nguyen AA, et al. Newborn screening for severe combined immunodeficiency and T-cell lymphopenia in California, 2010–2017. Pediatrics. 2019;143(2):e20182300.
Yska HAF, Elsink K, Kuijpers TW, Frederix GWJ, van Gijn ME, van Montfrans JM. Diagnostic yield of next generation sequencing in genetically undiagnosed patients with primary immunodeficiencies: a systematic review. J Clin Immunol. 2019;39(6):577–91.
Mauracher AA, Pagliarulo F, Faes L, Vavassori S, Güngör T, Bachmann LM, et al. Causes of low neonatal T-cell receptor excision circles: a systematic review. J Allergy Clin Immunol Pract. 2017;5(5):1457–1460.e22.
Albin-Leeds S, Ochoa J, Mehta H, Vogel BH, Caggana M, Bonagura V, et al. Idiopathic T cell lymphopenia identified in New York state newborn screening. Clin Immunol. 2017;183:36–40.
Evans MO 2nd, McDermott DH, Murphy PM, Petersen MM. Abnormal newborn screen in a WHIM syndrome infant. J Clin Immunol. 2019;39(8):839–41. https://doi.org/10.1007/s10875-019-00686-5.
Heusinkveld LE, Yim E, Yang A, Azani AB, Liu Q, Gao JL, et al. Pathogenesis, diagnosis and therapeutic strategies in WHIM syndrome immunodeficiency. Expert Opin Orphan Drugs. 2017;5(10):813–25.
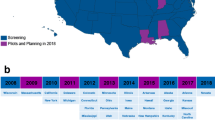
Dorsey M, Puck J. Newborn screening for severe combined immunodeficiency in the US: Current status and approach to management. Int J Neonatal Screen. 2017;3:15. https://doi.org/10.3390/ijns3020015.
Kobrynski LJ. Identification of severe combined immune deficiency T cell lymphopenia at newborn screening for severe combined immune deficiency. Ann Allergy Asthma Immunol. 2019;123:424–7. https://doi.org/10.1016/j.anai.2019.08.006.
Shearer WT, et al. Establishing diagnostic criteria for severe combined immunodeficiency disease (SCID), leaky SCID, and Omenn syndrome: the Primary Immune Deficiency Treatment Consortium experience. J Allergy Clin Immunol. 2014;133:1092–8. https://doi.org/10.1016/j.jaci.2013.09.044.
Dorsey MJ, Dvorak CC, Cowan MJ, Puck JM. Treatment of infants identified as having severe combined immunodeficiency by means of newborn screening. J Allergy Clin Immunol. 2017;139:733–42. https://doi.org/10.1016/j.jaci.2017.01.005.
Fernandez IZ, Baxter RM, Garcia-Perez JE, Vendrame E, Ranganath T, Kong DS, et al. A novel human IL2RB mutation results in T and NK cell-driven immune dysregulation. J Exp Med. 2019;216:1255–67. https://doi.org/10.1084/jem.20182015.
Picard C, Bobby Gaspar H, al-Herz W, Bousfiha A, Casanova JL, Chatila T, et al. International Union of Immunological Societies: 2017 primary immunodeficiency diseases committee report on inborn errors of immunity. J Clin Immunol. 2018;38:96–128. https://doi.org/10.1007/s10875-017-0464-9.
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A, Franco JL, Holland SM, Klein C, Morio T, Ochs HD, Oksenhendler E, Picard C, Puck J, Torgerson TR, Casanova JL, Sullivan KE. Human inborn errors of immunity: 2019 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol. 2020 Jan;40(1):24–64.
Dorsey MJ, Wright NAM, Chaimowitz NS, Dávila Saldaña BJ, Miller H, Keller MD, Thakar MS, Shah AJ, Abu-Arja R, Andolina J, Aquino V, Barnum JL, Bednarski JJ, Bhatia M, Bonilla FA, Butte MJ, Bunin NJ, Chandra S, Chaudhury S, Chen K, Chong H, Cuvelier GDE, Dalal J, DeFelice ML, DeSantes KB, Forbes LR, Gillio A, Goldman F, Joshi AY, Kapoor N, Knutsen AP, Kobrynski L, Lieberman JA, Leiding JW, Oshrine B, Patel KP, Prockop S, Quigg TC, Quinones R, Schultz KR, Seroogy C, Shyr D, Siegel S, Smith AR, Torgerson TR, Vander Lugt MT, Yu LC, Cowan MJ, Buckley RH, Dvorak CC, Griffith LM, Haddad E, Kohn DB, Logan B, Notarangelo LD, Pai SY, Puck J, Pulsipher MA, Heimall J. Infections in infants with SCID: Isolation, infection screening, and Prophylaxis in PIDTC Centers. J Clin Immunol. 2020.
Selim MA, Markert ML, Burchette JL, Herman CM, Turner JW. The cutaneous manifestations of atypical complete DiGeorge syndrome: a histopathologic and immunohistochemical study. J Cutan Pathol. 2008;35(4):380–5.
Villa A, Santagata S, Bozzi F, Giliani S, Frattini A, Imberti L, et al. Partial V(D)J recombination activity leads to Omenn syndrome. Cell. 1998;93:885–96.
Wada T, Yasui M, Toma T, Nakayama Y, Nishida M, Shimizu M, et al. Detection of T lymphocytes with a second-site mutation in skin lesions of atypical X-linked severe combined immunodeficiency mimicking Omenn syndrome. Blood. 2008;112(5):1872–5.
Roifman CM, Zhang J, Atkinson A, Grunebaum E, Mandel K. Adenosine deaminase deficiency can present with features of Omenn syndrome. J Allergy Clin Immunol. 2008;121(4):1056–8.
Turul T, Tezcan I, Artac H, de Bruin-Versteeg S, Barendregt BH, Reisli I, et al. Clinical heterogeneity can hamper the diagnosis of patients with ZAP70 deficiency. Eur J Pediatr. 2009;168(1):87–93.
Ege M, Ma Y, Manfras B, Kalwak K, Lu H, Lieber MR, et al. Omenn syndrome due to ARTEMIS mutations. Blood. 2005;105(11):4179–86.
Grunebaum E, Bates A, Roifman CM. Omenn syndrome is associated with mutations in DNA ligase IV. J Allergy Clin Immunol. 2008;122(6):1219–20.
Gennery AR, Slatter MA, Rice J, Hoefsloot LH, Barge D, McLean-Tooke A, et al. Mutations in CHD7 in patients with CHARGE syndrome cause T-B + natural killer cell + severe combined immune deficiency and may cause Omenn-like syndrome. Clin Exp Immunol. 2008;153(1):75–80.
Giliani S, Bonfim C, de Saint Basile G, Lanzi G, Brousse N, Koliski A, et al. Omenn syndrome in an infant with IL7RA gene mutation. J Pediatr. 2006;148(2):272–4.
Muller SM, Ege M, Pottharst A, Schulz AS, Schwarz K, Friedrich W. Transplacentally acquired maternal T lymphocytes in severe combined immunodeficiency: a study of 121 patients. Blood. 2001;98(6):1847–51.
Mehr S, Hsu P, Campbell D. Immunodeficiency in CHARGE syndrome. Am J Med Genet C: Semin Med Genet. 2017;175(4):516–23.
Yamazaki Y, Urrutia R, Franco LM, Giliani S, Zhang K, Alazami AM, et al. PAX1 is essential for development and function of the human thymus. Sci Immunol. 2020;5(44):eaax1036.
Gallo V, Cirillo E, Giardino G, Pignata C. FOXN1 deficiency: from the discovery to novel therapeutic approaches. J Clin Immunol. 2017;37(8):751–8.
Bosticardo M, Yamazaki Y, Cowan J, Giardino G, Corsino C, Scalia G, et al. Heterozygous FOXN1 variants cause low TRECs and severe T cell lymphopenia, revealing a crucial role of FOXN1 in supporting early thymopoiesis. Am J Hum Genet. 2019;105(3):549–61.
Du Q, Huynh LK, Coskun F, Molina E, King MA, Raj P, et al. FOXN1 compound heterozygous mutations cause selective thymic hypoplasia in humans. Clin Invest. 2019;129(11):4724–38.
Davies EG. Immunodeficiency in DiGeorge syndrome and options for treating cases with complete athymia. Front Immunol. 2013;4:322.
Caglayan Sozmen S, Isik S, Arikan Ayyildiz Z, Yildiz K, Cakır Y, Ozer E, et al. Cyclosporin treatment improves skin findings in Omenn syndrome. Pediatr Dermatol. 2015;32(2):e54–7.
Land MH, Garcia-Lloret MI, Borzy MS, Rao PN, Aziz N, McGhee SA, et al. Long-term results of bone marrow transplantation in complete DiGeorge syndrome. J Allergy Clin Immunol. 2007;120(4):908–15.
Kelty WJ, Beatty SA, Wu S, Hanson IC, Demmler-Harrison GJ, Martinez CA, et al. The role of breast-feeding in cytomegalovirus transmission and hematopoietic stem cell transplant outcomes in infants with severe combined immunodeficiency. J Allergy Clin Immunol Pract. 2019;7(8):2863–2865.e3.
Walter JE, Heimall J. CMV-Seropositive Mothers of SCID: To Breastfeed or Not? J Allergy Clin Immunol Pract. 2019;7(8):2866–7.
Rosenfeld L, Mas Marques A, Niendorf S, Hofmann J, Gratopp A, Kühl JS, et al. Life-threatening systemic rotavirus infection after vaccination in severe combined immunodeficiency (SCID). Pediatr Allergy Immunol. 2017;28(8):841–3.
Bakare N, Menschik D, Tiernan R, Hua W, Martin D. Severe combined immunodeficiency (SCID) and rotavirus vaccination: reports to the Vaccine Adverse Events Reporting System (VAERS). Vaccine. 2010;28(40):6609–12.
Waters V, Peterson KS, LaRussa P. Live viral vaccines in a DiGeorge syndrome patient. Arch Dis Child. 2007;92(6):519–20.
Hofstetter AM, Jakob K, Klein NP, Dekker CL, Edwards KM, Halsey NA, et al. Live vaccine use and safety in DiGeorge syndrome. Pediatrics. 2014;133(4):e946–54.
Al-Sukaiti NR, Lavi B, Al-Zaharani S, Atkinson D, Roifman Chaim M, Grunebaum E. Safety and efficacy of measles, mumps, and rubella vaccine in patients with DiGeorge syndrome. J Allergy Clin Immunol. 2010;126(4):868–9.
El-Sayed ZA, Radwan N. Newborn screening for primary immunodeficiencies: the gaps, challenges, and outlook for developing countries. Front Immunol. 2020;10:2987.
Amatuni GS, Sciortino S, Currier RJ, Naides SJ, Church JA, Puck JM. Reference intervals for lymphocyte subsets in preterm and term neonates without immune defects. J Allergy Clin Immunol. 2019;144(6):1674–83.
Joyce S, Gordon K, Brice G, Ostergaard P, Nagaraja R, Short J, et al. The lymphatic phenotype in Noonan and cardiofaciocutaneous syndrome. Eur J Hum Genet. 2016;24(5):690–6.
Kuo CY, Garcia-Lloret MI, Slev P, Bohnsack JF, Chen K. Profound T cell Lymphopenia associated with prenatal exposure to purine antagonists detected by TREC newborn screening. J Allergy Clin Immunol Pract. 2017;5(1):198–200.
Mancebo E, Clemente J, Sanchez J, Ruiz-Contreras J, De Pablos P, Cortezon S, et al. Longitudinal analysis of immune function in the first 3 years of life in thymectomized neonates during cardiac surgery. Clin Exp Immunol. 2008;154(3):375–83.
Mattes M, Connor J, Kelly SS, Schwartz MC. Lymphopenia in patients with single-ventricle heart disease after the Fontan operation. Congenit Heart Dis. 2016;11(3):270–5.
Hoskote AU, Ramaiah RN, Cale CM, Hartley JC, Brown KL. Role of immunoglobulin supplementation for secondary immunodeficiency associated with chylothorax after pediatric cardiothoracic surgery. Pediatr Crit Care Med. 2012;13(5):535–41.
Devaney R, Pasalodos S, Suri M, Bush A, Bhatt JM. Ataxia telangiectasia: presentation and diagnostic delay. Arch Dis Child. 2017;102(4):328–30.
Berland A, Rosain J, Kaltenbach S, Allain V, Mahlaoui N, Melki I, et al. PROMIDISalpha: a T-cell receptor alpha 407 signature associated with immunodeficiencies caused by V(D)J recombination defects. J Allergy Clin Immunol. 2019;143(1):325–34 e322.
Purswani P, Meehan CA, Kuehn HS, Chang Y, Dasso JF, Meyer AK, et al. Two unique cases of X-linked SCID: a diagnostic challenge in the era of newborn screening. Front Pediatr. 2019;7:55.
Mensa-Vilaró A, Bravo García-Morato M, de la Calle-Martin O, Franco-Jarava C, Martínez-Saavedra MT, González-Granado LI, et al. Unexpected relevant role of gene mosaicism in patients with primary immunodeficiency diseases. J Allergy Clin Immunol. 2019;143(1):359–68.
Author information
Authors and Affiliations
Contributions
All authors helped draft and approved the submitted manuscript. CAC and DB coordinated the creation of the original draft manuscript. DB, MJB, WYC, VRD, MJD, DJN, JMP, JS, and CAC participated in regular teleconferences surrounding the diagnostic evaluation and treatment of the immune disorders depicted in each case. All authors helped review the literature and cases. JEW and MCL helped illustrate the manuscript with the accompanying tables.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buchbinder, D., Walter, J.E., Butte, M.J. et al. When Screening for Severe Combined Immunodeficiency (SCID) with T Cell Receptor Excision Circles Is Not SCID: a Case-Based Review. J Clin Immunol 41, 294–302 (2021). https://doi.org/10.1007/s10875-020-00931-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-020-00931-2