Abstract
Purpose
Jacobsen syndrome (JS) is a rare form of genetic disorder that was recently classified as a syndromic immunodeficiency. Available detailed immunological data from JS patients are limited.
Methods
Clinical and immunological presentation of twelve pediatric patients with JS by means of revision of clinical records, flow cytometry, real-time PCR, and lymphocyte functional testing were collected.
Results
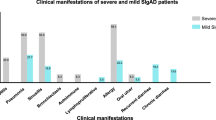
Recurrent infections were registered in 6/12 patients (50%), while bleeding episodes in 2/12 (16.7%). White blood cell and absolute lymphocyte counts were reduced in 8/12 (66.7%) and 7/12 (58.3%) patients, respectively. Absolute numbers of CD3+ and CD4+ T cells were reduced in 8/12 (66.7%) and 7/12 (58.3%), respectively. Of note, recent thymic emigrants (RTE) were reduced in all tested patients (9/9), with T-cell receptor excision circle analysis (TRECs) showing a similar trend in 8/9 patients; naïve CD4+ T cells were low only in 5/11 patients (45.4%). Interestingly, B-cell counts, IgM memory B cells, and IgM serum levels were reduced in 10/12 (83.3%) patients. Natural killer (NK) cell counts were mostly normal but the percentages of CD16+CD56low/− cells were expanded in 7/7 patients tested. The observed immunological alterations did not correlate with patients’ age. Finally, responses to proliferative stimuli were normal at presentation for all patients, although they may deteriorate over time.
Conclusions
Our data suggest that patients affected with JS may display important numeric and maturational alterations in the T-, B-, and NK-cell compartments. These findings suggest that JS patients should be regularly monitored from an immunological point of view.


Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Jacobsen P, Hauge M, Henningsen K, Hobolth N, Mikkelsen M, Philip J. An (11;21) translocation in four generations with chromosome 11 abnormalities in the offspring. A clinical, cytogenetical, and gene marker study. Hum Hered. 1973;23:568–85. https://doi.org/10.1159/000152624.
Favier R, Akshoomoff N, Mattson S, Grossfeld P. Jacobsen syndrome: advances in our knowledge of phenotype and genotype. Am J Med Genet C Semin Med Genet. 2015;169(3):239–50. https://doi.org/10.1002/ajmg.c.31448.
Grossfeld PD, Mattina T, Lai Z, Favier R, Jones KL, Cotter F, et al. The 11q terminal deletion disorder: a prospective study of 110 cases. Am J Med Genet A. 2004;129A(1):51–61. https://doi.org/10.1002/ajmg.a.30090.
Penny LA, Dell’Aquila M, Jones MC, Bergoffen J, Cunniff C, Fryns JP, et al. Clinical and molecular characterization of patients with distal 11q deletions. Am J Hum Genet. 1995;56(3):676–83.
Tootleman E, Malamut B, Akshoomoff N, Mattson SN, Hoffman HM, Jones MC, et al. Partial Jacobsen syndrome phenotype in a patient with a de novo frameshift mutation in the ETS1 transcription factor. Cold Spring Harb Mol Case Stud. 2019;5(3):1–9. https://doi.org/10.1101/mcs.a004010.
Stevenson WS, Rabbolini DJ, Beutler L, Chen Q, Gabrielli S, Mackay JP, et al. Paris-Trousseau thrombocytopenia is phenocopied by the autosomal recessive inheritance of a DNA-binding domain mutation in FLI1. Blood. 2015;126(17):2027–30. https://doi.org/10.1182/blood-2015-06-650887.
Pivnick EK, Velagaleti GV, Wilroy RS, Smith ME, Rose SR, Tipton RE, et al. Jacobsen syndrome: report of a patient with severe eye anomalies, growth hormone deficiency, and hypothyroidism associated with deletion 11 (q23q25) and review of 52 cases. J Med Genet. 1996;33(9):772–8. https://doi.org/10.1136/jmg.33.9.772.
Breton-Gorius J, Favier R, Guichard J, Cherif D, Berger R, Debili N, et al. A new congenital dysmegakaryopoietic thrombocytopenia (Paris-Trousseau) associated with giant platelet α-granules and chromosome 11 deletion at 11q23. Blood. 1995;85(7):1805–14. https://doi.org/10.1182/blood.v85.7.1805.bloodjournal8571805.
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A, et al. Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee. Epub 2020. Erratum in: J Clin Immunol. 2020 Feb 22. J Clin Immunol. 2020;40(1):24–64. https://doi.org/10.1007/s10875-019-00737-x.
Dalm VASH, Driessen GJA, Barendregt BH, van Hagen PM, van der Burg M. The 11q terminal deletion disorder Jacobsen syndrome is a syndromic primary immunodeficiency. J Clin Immunol. 2015;35(8):761–8. https://doi.org/10.1007/s10875-015-0211-z.
Sottini A, Ghidini C, Zanotti C, Chiarini M, Caimi L, Lanfranchi A, et al. Simultaneous quantification of recent thymic T-cell and bone marrow B-cell emigrants in patients with primary immunodeficiency undergone to stemcell transplantation. Clin Immunol. 2010;136:217–27. https://doi.org/10.1016/j.clim.2010.04.005.
Remaschi G, Ricci S, Cortimiglia M, De Vitis E, Iannuzzi L, Boni L, et al. TREC and KREC in very preterm infants: reference values and effects of maternal and neonatal factors. J Matern Fetal Neonatal Med. 2019;29:1–6. https://doi.org/10.1080/14767058.2019.1702951.
Seppänen M, Koillinen H, Mustjoki S, Tomi M, Sullivan KE. Terminal deletion of 11q with significant late-onset combined immune deficiency. J Clin Immunol. 2014;34(1):114–8. https://doi.org/10.1007/s10875-013-9966-2.
Grossfeld P. Brain hemorrhages in Jacobsen syndrome: a retrospective review of six cases and clinical recommendations. Am J of Med Genet A. 2017;173(3):667–70. https://doi.org/10.1002/ajmg.a.38032.
Muller-Durovic B, Grahlert J, Devine OP, Akbar AN, Hess C. CD56-negative NK cells with impaired effector function expand in CMV and EBV co-infected healthy donors with age. Aging. 2019;11:724–40. https://doi.org/10.18632/aging.101774.
Milush JM, Lopez-Verges S, York VA, Deeks SG, Martin JN, Hecht FM, et al. CD56negCD16(+) NK cells are activated mature NK cells with impaired effector function during HIV-1 infection. Retrovirology. 2013;10:158. https://doi.org/10.1186/1742-4690-10-158.
Weller S, Bonnet M, Delagreverie H, Israel L, Chrabieh M, Maródi L, et al. IgM+IgD+CD27+ B cells are markedly reduced in IRAK-4-, MyD88-, and TIRAP- but not UNC-93B-deficient patients. Blood. 2012;120(25):4992–5001. https://doi.org/10.1182/blood-2012-07-440776.
Nguyen HV, Mouly E, Chemin K, Luinaud R, Despres R, Fermand JP, et al. The Ets-1 transcription factor is required for Stat1-mediated T-bet expression and IgG2a class switching in mouse B cells. Blood. 2012;119(18):4174–81. https://doi.org/10.1182/blood-2011-09-378182.
Tsao HW, Tai TS, Tseng W, Chang HH, Grenningloh R, Miaw SC, et al. Ets-1 facilitates nuclear entry of NFAT proteins and their recruitment to the IL-2 promoter. Proc Natl Acad Sci U S A. 2013;110(39):15776–81. https://doi.org/10.1073/pnas.1304343110.
Smeets MF, Wiest DL, Izon DJ. Fli-1 regulates the DN2 to DN3 thymocyte transition and promotes gammadelta T-cell commitment by enhancing TCR signal strength. Eur J Immunol. 2014;44(9):2617–24. https://doi.org/10.1002/eji.201444442.
Bradshaw S, Zheng WJ, Tsoi LC, Gilkeson G, Zhang XK. A role for Fli-1 in B cell proliferation: implications for SLE pathogenesis. Clin Immunol. 2008;129(1):19–30. https://doi.org/10.1016/j.clim.2008.05.010.
Masuya M, Moussa O, Abe T, Deguchi T, Higuchi T, Ebihara Y, et al. Dysregulation of granulocyte, erythrocyte, and NK cell lineages in Fli-1 gene-targeted mice. Blood. 2005;105(1):95–102. https://doi.org/10.1182/blood-2003-12-4345.
Acknowledgements
We would like to thank the patients, the patients’ families, and the nurses for their collaboration and efforts. Several of the authors are members of the European Reference Network for Rare Immunodeficiency, Autoinflammatory and Autoimmune Diseases (project identification no. 739543).
Funding
The research leading to these results has received funding from the European Community’s Seventh Framework Programme FP7/ 2007–2013 under grant agreement no 201549 (EURO-PADnet HEALTH- F2–2008–201549) and grant from the Italian Ministry of Research GR- 2010–2315762. The research leading to these results also received funding from the “Fondazione C. Golgi,” Brescia, Italy, and the Jeffrey Modell Foundation. We thank “Fondazione Città della Speranza ONLUS (https://cittadellasperanza.org/)” for their support to our scientific work.
Author information
Authors and Affiliations
Contributions
M.B., F.S., L.G., S.R., A.M., S.R., D.Z., A.P., D.M., V.L. designed the work and coordinated the project; M.B., F.S., L.G., S.R., A.M., S.R., D.M., B.P., C.C., L.L., M.C., A.S., L.I., C.G., L.R. R.B., A.P., D.M., V.L. contributed with clinical, immunological, and molecular data; M.B., L.G., S.R., A.M., S.R., A.P., D.M., V.L. analyzed the data and wrote the manuscript; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved from the local hospital Ethical Committee and was conducted in accordance with the 1964 Helsinki Declaration.
Consent to Participate
Informed consent was collected from all patients or their legal guardians.
Consent for Publication
Informed consent was collected from all patients or their legal guardians.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10875_2021_1169_MOESM1_ESM.pdf
Supplementary file1 (PDF 115 KB) Supplementary Table 1. Detailed hematologic and immunologic evaluation of twelve patients with Jacobsen Syndrome
10875_2021_1169_MOESM2_ESM.pdf
Supplementary file2 (PDF 84 KB) Supplementary Figure 1. Flow cytometry representation of natural killer cells distribution in Jacobsen Syndrome patients. Representative cytofluorimetric panels of CD3-CD16/CD56+ NK cells, in which it is highlighted the relative proportion of CD16+CD56dim (dark pink) and CD16+CD56low/- (pink) cells, are shown for Pt9 (right) compared to an age-matched heathy control (HC) (left)
10875_2021_1169_MOESM3_ESM.pdf
Supplementary file3 (PDF 158 KB) Supplementary Figure 2. Long term immunological follow-up of a single patient with Jacobsen Syndrome. Patient’s parameters over a 6-year follow up period: A) WBCs (absolute counts), B) lymphocytes (absolute counts), C) serum IgA, D) serum IgM, E) CD4 naïve (percentages) F) CD4 RTE (percentages), G) CD8 naïve (percentages) H) switched memory (percentages), I) IgM memory cells (percentages) compared to aged matched healthy controls’ range (grey full area). L) Mitogen proliferative response to anti-CD3 MoAb, anti-CD3 MoAb + IL2, PHA, over time. = reduced response compared to control
Rights and permissions
About this article
Cite this article
Baronio, M., Saettini, F., Gazzurelli, L. et al. Immunological Evaluation of Patients Affected with Jacobsen Syndrome Reveals Profound Not Age-Related Lymphocyte Alterations. J Clin Immunol 42, 365–374 (2022). https://doi.org/10.1007/s10875-021-01169-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-021-01169-2