Abstract
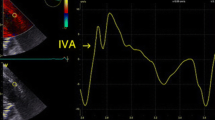
Right Ventricular (RV) output mostly derives from longitudinal shortening in normal hearts. However, following even uncomplicated cardiac surgery with preserved RV function a significant and sustained decrease in longitudinal contraction has been observed. How the RV compensates and sustains output in this setting remains unsettled. The aim of this study was to evaluate the RV contraction pattern by speckle tracking echocardiography to elucidate possible compensatory mechanisms mitigating the reduced RV longitudinal contraction after cardiac surgery. Thirty patients with normal preoperative ejection fraction and no valvulopathy underwent coronary artery bypass grafting (CABG) with the use of cardiopulmonary bypass (CPB). RV dedicated speckle tracking software measuring longitudinal and transverse displacement, as well as strain, was employed on transesophageal echocardiographic (TEE) images as part of the Right Ventricular Echocardiography in cardiac SurgEry (ReVERSE) study. Data was recorded at baseline (after anesthesia induction), immediately after CPB and upon chest closure. Tricuspid Annulus Plane Systolic Excursion (TAPSE) was reduced from 2.0 [1.6–2.5 cm] to 0.8 [0.6–11 mm] from baseline to after chest closure. RV longitudinal displacement was reduced from 6.1 [3.4–8.8 mm] to 2.9 [0.4–5.4 mm] at the same time-points. RV speckle tracking revealed concomitantly that transverse displacement of the free wall increased significantly from 1.2 [0–2.7 mm] at baseline to 5.4 [3.6–7.2 mm] after chest closure. RV speckle tracking strain did not change significantly. Increased transverse displacement likely compensates for reduction in RV longitudinal contraction following cardiac surgery and maintains cardiac output. The sustained output from the right ventricle was not related to an increased contractility.




Similar content being viewed by others
References
Rushmer RF, Thal N. The mechanics of ventricular contraction; a cinefluorographic study. Circulation. 1951;4:219–28.
Maus TM. TAPSE: a red herring after cardiac surgery. J Cardiothorac Vasc Anesth. 2018;32:779–81.
Korshin A, Grønlykke L, Nilsson JC, Møller-Sørensen H, Ihlemann N, Kjøller SM, et al. Tricuspid annular plane systolic excursion is significantly reduced during uncomplicated coronary artery bypass surgery: a prospective observational study. J Thorac Cardiovasc Surg. 2018;158:480–9.
Grønlykke L, Ihlemann N, Ngo AT, Thyregod HGH, Kjaergaard J, Korshin A, et al. Measures of right ventricular function after transcatheter versus surgical aortic valve replacement. Interact Cardiovasc Thorac Surg. 2017;24:181–7.
Becker M, Robbers L, Brouwer W, Beck A, Abel MD, Bondarenko O, et al. A Cardiovascular magnetic resonance study on the short and long-term effects of coronary artery bypass graft surgery on the right ventricular systolic function. Madridge J Cardiol. 2017;1:14–20.
Tamborini G, Muratori M, Brusoni D, Celeste F, Maffessanti F, Caiani EG, et al. Is right ventricular systolic function reduced after cardiac surgery? A two- and three-dimensional echocardiographic study. Eur J Echocardiogr. 2009;10:630–4.
Maffessanti F, Gripari P, Tamborini G, Muratori M, Fusini L, Alamanni F, et al. Evaluation of right ventricular systolic function after mitral valve repair: a two-dimensional Doppler, speckle-tracking, and three-dimensional echocardiographic study. J Am Soc Echocardiogr. 2012;25:701–8.
Coisne A, Modine T, Outteryck F, Mouton S, Pilato R, Ridon H, et al. Clinical significance of right ventricular longitudinal function parameters after aortic valve replacement. JACC Cardiovasc Imaging. 2017;11:651–2.
Jadhav T, Kareem H, Nayak K, Pai U, Devasia T. Padmakumar R (2018) A study of right ventricular function in pre- and post-valvular surgeries. Interv Med Appl Sci. 2018;10(3):137–44.
Khani M, Hosseintash M, Foroughi M, Naderian M, Khaheshi I. Assessment of the effect of off-pump coronary artery bypass (OPCAB) surgery on right ventricle function using strain and strain rate imaging. Cardiovasc Diagn Ther. 2016;6:138–43.
Rösner A, Avenarius D, Malm S, Iqbal A, Schirmer H, Bijnens B, et al. Changes in right ventricular shape and deformation following coronary artery bypass surgery-insights from echocardiography with strain rate and magnetic resonance imaging. Echocardiography. 2015;32:1809–20.
Garcia Gigorro R, Renes Carreño E, Mayordomo S, Marín H, Perez Vela JL, Corres Peiretti MA, et al. Evaluation of right ventricular function after cardiac surgery: the importance of tricuspid annular plane systolic excursion and right ventricular ejection fraction. J Thorac Cardiovasc Surg. 2016;152:613–20.
Schuuring MJ, Bolmers PPM, Mulder BJM, de Bruin-Bon RACM, Koolbergen DR, Hazekamp MG, et al. Right ventricular function declines after cardiac surgery in adult patients with congenital heart disease. Int J Cardiovasc Imaging. 2012;28:755–62.
Bitcon CJ, Tousignant C. The effect of pericardial incision on right ventricular systolic function: a prospective observational study. Can J Anaesth. 2017;64:1194–201.
Grønlykke L, Korshin A, Holmgaard F, Kjøller SM, Gustafsson F, Nilsson JC, et al. Severe loss of right ventricular longitudinal contraction occurs after cardiopulmonary bypass in patients with preserved right ventricular output. Int J Cardiovasc Imaging. 2019;95:1507–10.
Korshin A, Grønlykke L, Nilsson J-C, Møller-sørensen H, Ihlemann N, Kjøller M, et al. The feasibility of tricuspid annular plane systolic excursion performed by transesophageal echocardiography throughout heart surgery and its interchangeability with transthoracic echocardiography. Int J Cardiovasc Imaging. 2018;30:283.
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–48.
Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62:D22–33.
Joshi SB, Salah AK, Mendoza DD, Goldstein SA, Fuisz AR, Lindsay J. Mechanism of paradoxical ventricular septal motion after coronary artery bypass grafting. Am J Cardiol. 2009;103:212–5.
Mehra MR, Park MH, Landzberg MJ, Lala A, Waxman AB. International right heart failure foundation scientific working group. right heart failure: toward a common language. J Heart Lung Transplant. 2014;33:123–6.
Amsallem M, Mercier O, Kobayashi Y, Moneghetti K, Haddad F. Forgotten no more: a focused update on the right ventricle in cardiovascular disease. JACC Heart Fail. 2018;6:891–903.
Schneider M, Binder T. Echocardiographic evaluation of the right heart. Wien Klin Wochenschr. 2018;130:413–20.
Dandel M, Hetzer R. Evaluation of the right ventricle by echocardiography: particularities and major challenges. Expert Rev Cardiovasc Ther. 2018;16:259–75.
Grønlykke L, Ravn HB, Gustafsson F, Hassager C, Kjaergaard J, Nilsson JC. Right ventricular dysfunction after cardiac surgery—diagnostic options. Scand Cardiovasc J. 2016;51:114–21.
Duncan AE, Sarwar S, Kateby Kashy B, Sonny A, Sale S, Alfirevic A, et al. Early left and right ventricular response to aortic valve replacement. Anesth Analg. 2017;124:406–18.
Desai RR, Vargas Abello LM, Klein AL, Marwick TH, Krasuski RA, Ye Y, et al. Tricuspid regurgitation and right ventricular function after mitral valve surgery with or without concomitant tricuspid valve procedure. J Thorac Cardiovasc Surg. 2013;146:1126–32.e10.
Arya A, Pande S, Agarwal SK, Srivastav N, Srivastava NK, Kumar S, et al. Effect of coronary artery bypass grafting on function of right ventricle in patients with severe left ventricular dysfunction. J Indian Coll Cardiol. 2016;6:1–5.
Foo JS, Lazu M, Pang SY, Lee PT, Tan JL. Comparative analysis of right heart chamber remodeling after surgical and device secundum atrial septal defect closure in adults. J Interv Cardiol. 2018;31:672–8.
Mazurek JA, Vaidya A, Mathai SC, Roberts JD, Forfia PR. Follow-up tricuspid annular plane systolic excursion predicts survival in pulmonary arterial hypertension. Pulm Circ. 2017;7:361–71.
Modin D, Mogelvang R, Andersen DM, Biering-Sorensen T. Right ventricular function evaluated by tricuspid annular plane systolic excursion predicts cardiovascular death in the general population. J Am Heart Assoc. 2019;8:e012197.
Buckberg G, Hoffman JIE. Right ventricular architecture responsible for mechanical performance: unifying role of ventricular septum. J Thorac Cardiovasc Surg. 2014;148:3166–71.e1–4.
Moya Mur J-L, García Martín A, García Lledó A, Lázaro Rivera C, Rincón Díaz LM, Miguelena Hycka J, et al. Geometrical and functional cardiac changes after cardiac surgery: a phisiopatological explanation based on speckle tracking. Int J Cardiovasc Imaging. 2018;108:422.
Geske JB, Anavekar NS, the RNJO, 2016. Differentiation of constriction and restriction: complex cardiovascular hemodynamics. onlinejacc.org
Salvo GD, Pergola V, Fadel B, Bulbul ZA, Caso P. Strain echocardiography and myocardial mechanics: from basics to clinical applications. J Cardiovasc Echogr. 2015;25:1–8.
Yockelson SR, Heitner SB, Click S, Geleto G, Treggiari MM, Hutchens MP. Right ventricular systolic performance determined by 2D speckle-tracking echocardiography and acute kidney injury after cardiac surgery. J Cardiothorac Vasc Anesth. 2018;33:725–31.
Li Y, Wang Y, Ye X, Kong L, Zhu W, Lu X. Clinical study of right ventricular longitudinal strain for assessing right ventricular dysfunction and hemodynamics in pulmonary hypertension. Medicine (Baltimore). 2016;95:e5668.
Singh A, Huang X, Dai L, Wyler D, Alfirevic A, Blackstone EH, et al. Right ventricular function is reduced during cardiac surgery independent of procedural characteristics, reoperative status, or pericardiotomy. J Thorac Cardiovasc Surg. 2019. https://doi.org/10.1016/j.jtcvs.2019.04.035.
Reynolds HR, Tunick PA, Grossi EA, Dilmanian H, Colvin SB, Kronzon I. Paradoxical septal motion after cardiac surgery: a review of 3,292 cases. Clin Cardiol. 2007;30:621–3.
Kirklin JW. Theye RA. Cardiac performance after open intracardiac surgery. Circulation. 1963;28:1061–70.
Čanádyová J, Zmeko D, Mokráček A. Re-exploration for bleeding or tamponade after cardiac operation. Interact Cardiovasc Thorac Surg. 2012;14:704–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1—Video 1: Transesophageal echocardiographic loop in the mid-esophageal 4-chamber view with using speckle tracking software from TomTec 2D cardiac performance analysis applied (TomTec Imaging Systems GMBH, Unterschleissheim, Germany). (AVI 19573 kb)
Rights and permissions
About this article
Cite this article
Korshin, A., Grønlykke, L., Holmgaard, F. et al. Right ventricular transverse displacement increases following cardiac surgery: possibly compensating loss in tricuspid annular plane systolic excursion (TAPSE). J Clin Monit Comput 34, 1139–1148 (2020). https://doi.org/10.1007/s10877-020-00466-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00466-2