Abstract
Purpose
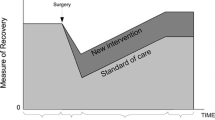
Functional dependency is a known determinant of surgical risk. To enhance our understanding of the relationship between dependency and adverse surgical outcomes, we studied how postoperative mortality following a surgical complication was impacted by preoperative functional dependency.
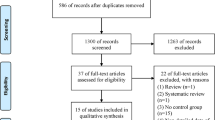
Methods
We explored a historical cohort of 6,483,387 surgical patients within the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). All patients ≥ 18 years old within the ACS-NSQIP from 2007 to 2017 were included.
Results
There were 6,222,611 (96.5%) functionally independent, 176,308 (2.7%) partially dependent, and 47,428 (0.7%) totally dependent patients. Within 30 days postoperatively, 57,652 (0.9%) independent, 15,075 (8.6%) partially dependent, and 10,168 (21.4%) totally dependent patients died. After adjusting for confounders, increasing functional dependency was associated with increased odds of mortality (Partially Dependent OR: 1.72, 99% CI: 1.66 to 1.77; Totally Dependent OR: 2.26, 99% CI: 2.15 to 2.37). Dependency also significantly impacted mortality following a complication; however, independent patients usually experienced much stronger increases in the odds of mortality. There were six complications not associated with increased odds of mortality. Model diagnostics show our model was able to distinguish between patients who did and did not suffer 30-day postoperative mortality nearly 96.7% of the time.
Conclusions
Within our cohort, dependent surgical patients had higher rates of comorbidities, complications, and odds of 30-day mortality. Preoperative functional status significantly impacted the level of postoperative mortality following a complication, but independent patients were most affected.
Similar content being viewed by others
References
Shah, R., et al., Association of Frailty with Failure to Rescue After Low-Risk and High-Risk Inpatient Surgery. JAMA Surg, 2018. 153(5): p. e180214.
Scarborough, J.E., et al., The impact of functional dependency on outcomes after complex general and vascular surgery. Ann Surg, 2015. 261(3): p. 432-7.
Pel-Littel, R.E., et al., Frailty: defining and measuring of a concept. J Nutr Health Aging, 2009. 13(4): p. 390-4.
Akyar, S., et al., The Impact of Frailty on Postoperative Cardiopulmonary Complications in the Emergency General Surgery Population. Surg J (N Y), 2018. 4(2): p. e66-e77.
Puts, M.T., P. Lips, and D.J. Deeg, Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol, 2005. 58(11): p. 1188-98.
Rockwood, K., et al., A global clinical measure of fitness and frailty in elderly people. Cmaj, 2005. 173(5): p. 489-95.
Theou, O., et al., Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc, 2013. 61(9): p. 1537-51.
Lally F, Crome P. Understanding frailty. Postgrad Med J. 2007;83(975):16-20. https://doi.org/10.1136/pgmj.2006.048587A
Linda P. Fried, Catherine M. Tangen, Jeremy Walston, Anne B. Newman, Calvin Hirsch, John Gottdiener, Teresa Seeman, Russell Tracy, Willem J. Kop, Gregory Burke, Mary Ann McBurnie, Frailty in Older Adults: Evidence for a Phenotype, The Journals of Gerontology: Series A, Volume 56, Issue 3, 1 March 2001, Pages M146–M157. https://doi.org/10.1093/gerona/56.3.M146A
Makary MA, Segev DL, Pronovost PJ Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP. Frailty as a predictor of surgical outcomes in older patients J Am Coll Surg. 2010 Jun;210(6):901–8. https://doi.org/10.1016/j.jamcollsurg.2010.01.028. Epub 2010 Apr 28 PMID: 20510798.
Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm--issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62(7):731-737. https://doi.org/10.1093/gerona/62.7.731A
Linda P. Fried, Luigi Ferrucci, Jonathan Darer, Jeff D. Williamson, Gerard Anderson, Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care, The Journals of Gerontology: Series A, Volume 59, Issue 3, March 2004, Pages M255–M263. https://doi.org/10.1093/gerona/59.3.M255A
Thomas N. Robinson, Ben Eiseman, Jeffrey I. Wallace, Skotti D. Church, Kim K. McFann, Shirley M. Pfister, Terra J. Sharp, Marc Moss, Redefining Geriatric Preoperative Assessment Using Frailty, Disability and Co-Morbidity, Annals of Surgery: September 2009 - Volume 250 - Issue 3 - p 449–455. https://doi.org/10.1097/SLA.0b013e3181b45598
Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL. Canadian Study of Health and Aging Clinical Frailty Scale: Does It Predict Adverse Outcomes among Geriatric Trauma Patients?. J Am Coll Surg. 2017 Nov;225(5):658–665.e3. https://doi.org/10.1016/j.jamcollsurg.2017.08.008. Epub 2017 Sep 6. PMID: 28888692.
Chow, W.B., et al., Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg, 2012. 215(4): p. 453-66.
Hall DE, Arya S, Schmid KK, Blaser C, Carlson MA, Bailey TL, Purviance G, Bockman T, Lynch TG, Johanning J. Development and Initial Validation of the Risk Analysis Index for Measuring Frailty in Surgical Populations. JAMA Surg. 2017 Feb 1;152(2)175–182. https://doi.org/10.1001/jamasurg.2016.4202. PMID: 27893030; PMCID: PMC7140150.
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J Am Coll Surg. 2018 Feb;226(2)173–181.e8. https://doi.org/10.1016/j.jamcollsurg.2017.11.005. Epub 2017 Nov 16. PMID: 29155268.
E Dent P Kowal EO Hoogendijk 2016 Jun Frailty measurement in research and clinical practice: A review Eur J Intern Med. 31 3 10 https://doi.org/10.1016/j.ejim.2016.03.007. Epub 2016 Mar 31 PMID: 27039014
McDonald VS, Thompson KA, Lewis PR, Sise CB, Sise MJ, Shackford SR. Frailty in trauma: A systematic review of the surgical literature for clinical assessment tools. J Trauma Acute Care Surg. 2016 May;80(5)824–834. https://doi.org/10.1097/TA.0000000000000981. PMID: 26881488.
Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Tang A, O'Keeffe T, Green DJ, Vercruysse G, Fain MJ, Friese RS, Rhee P. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg. 2014 Jul;219(1):10–17.e1. https://doi.org/10.1016/j.jamcollsurg.2014.03.020. Epub 2014 Mar 19. Erratum in: J Am Coll Surg. 2016 Mar;222(3):336. PMID: 24952434.
Program, A.C.o.S.N.S.Q.I. User Guide for the 2017 ACS NSQIP Participant Use Data File. 12/16/2020]; Available from: https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2017.ashx.
Fried, L.P., et al., Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci, 2004;59(3): p. 255–263.
Khan, M.A., et al., Perioperative risk factors for 30-day mortality after bariatric surgery: is functional status important? Surg Endosc, 2013. 27(5): p. 1772-7.
Ponzetto, M., et al., Risk factors for early and late mortality in hospitalized older patients: the continuing importance of functional status. J Gerontol A Biol Sci Med Sci, 2003. 58(11): p. 1049-54.
Cohen, M.E., et al., Effect of subjective preoperative variables on risk-adjusted assessment of hospital morbidity and mortality. Ann Surg, 2009. 249(4): p. 682-9.
Kilic, A., et al., Functional status is highly predictive of outcomes after redo lung transplantation: an analysis of 390 cases in the modern era. Ann Thorac Surg, 2013. 96(5): p. 1804–11; discussion 1811.
de la Fuente, S.G., K.M. Bennett, and J.E. Scarborough, Functional status determines postoperative outcomes in elderly patients undergoing hepatic resections. J Surg Oncol, 2013;107(8):865–70.
Lentine, K.L., et al., Impact of Functional Status on Outcomes of Simultaneous Pancreas-kidney Transplantation: Risks and Opportunities for Patient Benefit. Transplant Direct, 2020. 6(9): p. e599.
Stienen, M.N. et al., The influence of preoperative dependency on mortality, functional recovery and complications after microsurgical resection of intracranial tumors. J Neurooncol, 2018;139(2):441–448.
Network, E. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. 12/16/20]; Available from: https://www.equator-network.org/reporting-guidelines/strobe/.
White, I.R., P. Royston, and A.M. Wood, Multiple imputation using chained equations: Issues and guidance for practice. Stat Med, 2011;30(4): p. 377–99.
Buuren, S. and C. Groothuis-Oudshoorn, MICE: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software, 2011. 45.
Jakobsen, J.C., et al., When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med Res Methodol, 2017. 17(1): p. 162.
Little, R.J., et al., The prevention and treatment of missing data in clinical trials. The New England journal of medicine, 2012;367(14): p. 1355–1360.
Groenwold, R.H., et al., Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. Cmaj, 2012. 184(11): p. 1265-9.
Jones, M.P., Indicator and Stratification Methods for Missing Explanatory Variables in Multiple Linear Regression. Journal of the American Statistical Association, 1996. 91(433): p. 222-230.
Wasserstein, R.L. and N.A. Lazar, The ASA Statement on p-Values: Context, Process, and Purpose. The American Statistician, 2016. 70(2): p. 129-133.
Tibshirani, R., Regression Shrinkage and Selection Via the Lasso. Journal of the Royal Statistical Society: Series B (Methodological), 1996. 58(1): p. 267-288.
Bien, J., J. Taylor, and R. Tibshirani, A LASSO FOR HIERARCHICAL INTERACTIONS. Ann Stat, 2013. 41(3): p. 1111-1141.
Zhao, Y. and Q. Long, Variable Selection in the Presence of Missing Data: Imputation-based Methods. Wiley Interdiscip Rev Comput Stat, 2017. 9(5).
Steyerberg, E.W., et al., Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology, 2010. 21(1): p. 128-38.
Cook, N.R., Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem, 2008. 54(1): p. 17-23.
Freundlich, R.E., et al., Complications Associated With Mortality in the National Surgical Quality Improvement Program Database. Anesth Analg, 2018. 127(1): p. 55-62.
Naseer, M., H. Forssell, and C. Fagerström, Malnutrition, functional ability and mortality among older people aged ⩾ 60 years: a 7-year longitudinal study. Eur J Clin Nutr, 2016. 70(3): p. 399-404.
Curtis, G.L., et al., Dependent Functional Status is a Risk Factor for Perioperative and Postoperative Complications After Total Hip Arthroplasty. J Arthroplasty, 2019. 34(7s): p. S348-s351.
Minhas, S.V., A.S. Mazmudar, and A.A. Patel, Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Joint J, 2017. 99-b(6): p. 824–828.
Kaplan, R.M., D.A. Chambers, and R.E. Glasgow, Big data and large sample size: a cautionary note on the potential for bias. Clin Transl Sci, 2014. 7(4): p. 342-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Robert Freundlich has stock in Pfizer, 3 M, Johnson and Johnson, and Gilead Pharmaceuticals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Patient Demographics
Summary Statistics | ||||||
|---|---|---|---|---|---|---|
Whole dataset | Totally Independent | Partially Dependent | Totally Dependent | |||
Total Number of Patients | 6,483,387 | 6,222,611 | 176,308 | 47,428 | ||
Death (%) | 84,170 (1.3) | 57,652 (0.9) | 15,075 (8.6) | 10,168 (21.4) | ||
Demographics | Year (%) | 2007 | 210,405 (3.2) | 195,729 (3.1) | 10,236 (5.8) | 4440 (9.4) |
2008 | 269,847 (4.2) | 251,709 (4.0) | 12,963 (7.4) | 5175 (10.9) | ||
2009 | 336,185 (5.2) | 313,595 (5.0) | 16,503 (9.4) | 6087 (12.8) | ||
2010 | 363,431 (5.6) | 343,089 (5.5) | 14,923 (8.5) | 5210 (11.0) | ||
2011 | 442,149 (6.8) | 420,960 (6.8) | 14,120 (8.0) | 3878 (8.2) | ||
2012 | 543,885 (8.4) | 525,316 (8.4) | 13,542 (7.7) | 2903 (6.1) | ||
2013 | 651,940 (10.1) | 628,574 (10.1) | 14,715 (8.3) | 3145 (6.6) | ||
2014 | 750,937 (11.6) | 726,360 (11.7) | 16,006 (9.1) | 3184 (6.7) | ||
2015 | 885,502 (13.7) | 855,685 (13.8) | 20,042 (11.4) | 4178 (8.8) | ||
2016 | 1,000,393 (15.4) | 966,924 (15.5) | 21,245 (12.0) | 4549 (9.6) | ||
2017 | 1,028,713 (15.9) | 994,670 (16.0) | 22,013 (12.5) | 4679 (9.9) | ||
Race (%) | White | 4,747,446 (73.4) | 4,561,675 (73.5) | 126,902 (72.2) | 32,109 (68.0) | |
Black | 643,386 (9.9) | 608,546 (9.8) | 23,364 (13.3) | 8426 (17.9) | ||
Asian | 172,860 (2.7) | 166,434 (2.7) | 3801 (2.2) | 1015 (2.2) | ||
Other | 903,309 (14.0) | 870,373 (14.0) | 21,695 (12.3) | 5644 (12.0) | ||
Sex = Female (%) | 3,691,976 (57.0) | 3,549,090 (57.1) | 98,076 (55.7) | 24,242 (51.2) | ||
Age (years)—median (IQR) | 58 [45, 69] | 57 [44, 68] | 72 [60, 82] | 69 [56, 80] | ||
Height (cm)—median (IQR) | 168 [160, 175] | 168 [160, 175] | 165 [157, 175] | 168 [157, 175] | ||
Weight (kg)—median (IQR) | 81.6 [68.0, 97.5] | 81.6 [68.0, 97.5] | 74.4 [61.2, 90.7] | 72.6 [59.0, 88.9] | ||
Preoperative Comorbidities and Procedural Variables | Surgical Specialty (%) | General Surgery | 3,325,982 (51.3) | 3,211,754 (51.6) | 71,363 (40.5) | 26,090 (55.0) |
Vascular | 484,793 (7.5) | 437,155 (7.0) | 36,437 (20.7) | 8857 (18.7) | ||
Orthopedics | 1,189,299 (18.3) | 1,129,604 (18.2) | 44,290 (25.1) | 6708 (14.1) | ||
Urology | 321,597 (5.0) | 312,158 (5.0) | 5857 (3.3) | 1365 (2.9) | ||
Neurosurgery | 286,015 (4.4) | 273,362 (4.4) | 9168 (5.2) | 1799 (3.8) | ||
Other | 875,700 (13.5) | 858,577 (13.8) | 9193 (5.2) | 2609 (5.5) | ||
Wound Classification (%) | 1 – Clean | 3,575,426 (55.1) | 3,439,672 (55.3) | 96,463 (54.7) | 17,940 (37.8) | |
2 – Clean/ Contaminated | 2,140,662 (33.0) | 2,081,106 (33.4) | 38,687 (21.9) | 10,981 (23.2) | ||
3 – Contaminated | 423,012 (6.5) | 399,617 (6.4) | 14,776 (8.4) | 5693 (12.0) | ||
4 – Dirty/Infected | 344,282 (5.3) | 302,214 (4.9) | 26,382 (15.0) | 12,814 (27.0) | ||
ASA Class (%) | 1 | 583,875 (9.0) | 579,093 (9.3) | 1235 (0.7) | 87 (0.2) | |
2 | 2,912,622 (45.1) | 2,876,798 (46.4) | 18,893 (10.7) | 1886 (4.0) | ||
3 | 2,556,923 (39.6) | 2,417,971 (39.0) | 104,291 (59.3) | 20,239 (42.8) | ||
4/5 | 410,794 (6.4) | 330,433 (5.3) | 51,355 (29.2) | 25,078 (53.0) | ||
Diabetes (%) | 0 – No | 5,486,362 (84.6) | 5,302,856 (85.2) | 120,327 (68.2) | 32,787 (69.1) | |
1 – Insulin | 377,319 (5.8) | 330,895 (5.3) | 33,704 (19.1) | 9797 (20.7) | ||
2 – Non-Insulin | 619,698 (9.6) | 588,860 (9.5) | 22,277 (12.6) | 4844 (10.2) | ||
Dyspnea (%) | 0 – No | 6,044,616 (93.2) | 5,826,783 (93.6) | 145,917 (82.8) | 37,516 (79.1) | |
1 – At Rest | 42,863 (0.7) | 29,051 (0.5) | 7206 (4.1) | 6149 (13.0) | ||
2 – Moderate Exertion | 395,878 (6.1) | 366,762 (5.9) | 23,182 (13.1) | 3761 (7.9) | ||
Sepsis (%) | 0 – None | 6,084,721 (94.0) | 5,884,964 (94.8) | 140,007 (79.6) | 26,515 (56.0) | |
1 – Systemic Inflammatory Response Syndrome (SIRS) | 219,814 (3.4) | 192,436 (3.1) | 18,442 (10.5) | 6972 (14.7) | ||
2 – Sepsis | 135,212 (2.1) | 114,743 (1.8) | 13,177 (7.5) | 6082 (12.8) | ||
3 – Septic Shock | 31,359 (0.5) | 18,641 (0.3) | 4320 (2.5) | 7790 (16.4) | ||
Functional Status (%) | 0 – Totally Independent | 6,222,611 (96.5) | 6,222,611 (100.0) | 0 (0.0) | 0 (0.0) | |
1 – Partially Dependent | 176,308 (2.7) | 0 (0.0) | 176,308 (100.0) | 0 (0.0) | ||
2 – Totally Dependent | 47,428 (0.7) | 0 (0.0) | 0 (0.0) | 47,428 (100.0) | ||
Outpatient (%) | 2,550,335 (39.3) | 2,511,457 (40.4) | 17,433 (9.9) | 2786 (5.9) | ||
Transfer Status = Admitted from other (%) | 274,086 (4.2) | 202,184 (3.3) | 47,389 (26.9) | 21,499 (45.4) | ||
Emergency (%) | 636,169 (9.8) | 575,060 (9.2) | 37,692 (21.4) | 18,058 (38.1) | ||
Smoker (%) | 1,189,267 (18.3) | 1,142,322 (18.4) | 32,105 (18.2) | 7512 (15.8) | ||
Ventilator Dependent (%) | 29,861 (0.5) | 15,185 (0.2) | 2453 (1.4) | 11,582 (24.4) | ||
History of Severe Chronic Obstructive Pulmonary Disease (%) | 296,716 (4.6) | 263,668 (4.2) | 24,312 (13.8) | 6339 (13.4) | ||
Ascites (%) | 30,524 (0.5) | 24,623 (0.4) | 3268 (1.9) | 2401 (5.1) | ||
History of Congestive Heart Failure (%) | 56,817 (0.9) | 41,922 (0.7) | 10,120 (5.7) | 4161 (8.8) | ||
Hypertension Requiring Medication (%) | 2,943,652 (45.4) | 2,771,762 (44.5) | 123,744 (70.2) | 30,723 (64.8) | ||
Acute Renal Failure (%) | 25,937 (0.4) | 19,058 (0.3) | 3786 (2.1) | 2738 (5.8) | ||
Dialysis (%) | 94,879 (1.5) | 75,327 (1.2) | 13,473 (7.6) | 5052 (10.7) | ||
Disseminated Cancer (%) | 142,302 (2.2) | 132,313 (2.1) | 7499 (4.3) | 1738 (3.7) | ||
Open Wound/Wound Infection (%) | 216,208 (3.3) | 157,509 (2.5) | 39,712 (22.5) | 16,980 (35.8) | ||
Steroid Use for Chronic Condition (%) | 226,678 (3.5) | 207,868 (3.3) | 13,610 (7.7) | 3680 (7.8) | ||
Weight Loss (%) | 92,197 (1.4) | 80,291 (1.3) | 8687 (4.9) | 2723 (5.7) | ||
Bleeding Disorder (%) | 294,254 (4.5) | 250,997 (4.0) | 30,855 (17.5) | 9800 (20.7) | ||
Transfusion (%) | 58,983 (0.9) | 45,321 (0.7) | 8075 (4.6) | 4904 (10.3) | ||
Intraoperative/ Postoperative Complications | Return to Operating Room = Yes (%) | 214,429 (3.3) | 189,899 (3.1) | 16,015 (9.1) | 7192 (15.2) | |
Superficial Incisional Surgical Site Infection (%) | 114,112 (1.8) | 106,398 (1.7) | 5692 (3.2) | 1397 (2.9) | ||
Deep Incisional Surgical Site Infection (%) | 36,876 (0.6) | 33,148 (0.5) | 2670 (1.5) | 834 (1.8) | ||
Organ Space Surgical Site Infection (%) | 81,794 (1.3) | 76,040 (1.2) | 3792 (2.2) | 1507 (3.2) | ||
Wound Disruption (%) | 27,445 (0.4) | 24,442 (0.4) | 2058 (1.2) | 785 (1.7) | ||
Pneumonia (%) | 82,053 (1.3) | 66,004 (1.1) | 9817 (5.6) | 5376 (11.3) | ||
Unplanned Intubation (%) | 58,243 (0.9) | 47,258 (0.8) | 6996 (4.0) | 3437 (7.2) | ||
Pulmonary Embolism (%) | 21,471 (0.3) | 19,776 (0.3) | 1172 (0.7) | 418 (0.9) | ||
Progressive Renal Insufficiency (%) | 17,862 (0.3) | 15,411 (0.2) | 1618 (0.9) | 690 (1.5) | ||
Acute Renal Failure (%) | 20,581 (0.3) | 16,516 (0.3) | 2226 (1.3) | 1621 (3.4) | ||
Urinary Tract Infection (%) | 90,406 (1.4) | 78,808 (1.3) | 7861 (4.5) | 3135 (6.6) | ||
Stroke/Cerebrovascular Accident (%) | 13,548 (0.2) | 11,419 (0.2) | 1454 (0.8) | 576 (1.2) | ||
Cardiac Arrest (%) | 21,281 (0.3) | 16,569 (0.3) | 2743 (1.6) | 1703 (3.6) | ||
Myocardial Infarction (%) | 23,347 (0.4) | 19,872 (0.3) | 2545 (1.4) | 705 (1.5) | ||
Transfusions (%) | 329,261 (5.1) | 288,116 (4.6) | 29,329 (16.6) | 9115 (19.2) | ||
Deep Vein Thrombosis Requiring Therapy (%) | 38,829 (0.6) | 34,039 (0.5) | 3085 (1.7) | 1433 (3.0) | ||
Sepsis (%) | 107,620 (1.7) | 93,228 (1.5) | 9392 (5.3) | 4127 (8.7) | ||
Septic Shock (%) | 54,799 (0.8) | 42,644 (0.7) | 7368 (4.2) | 3980 (8.4) | ||
Lab Values | Blood Urea Nitrogen (mg/dL)—median (IQR) | 15.0 [11.0, 19.0] | 15.00 [11.0, 19.0] | 18.5 [13.0, 27.0] | 21.0 [13.0, 33.6] | |
Serum Albumin (g/dL)—median (IQR) | 4.0 [3.6, 4.3] | 4.0 [3.6, 4.3] | 3.3 [2.7, 3.8] | 2.8 [2.2, 3.4] | ||
Total Bilirubin (mg/dL)—median (IQR) | 0.5 [0.4, 0.8] | 0.5 [0.4, 0.8] | 0.5 [0.36, 0.8] | 0.6 [0.4, 0.9] | ||
Serum Glutamic Oxaloacetic Transaminase (units/L)—median (IQR) | 22 [17,29] | 22 [17,29] | 22 [17,31] | 25 [18,41] | ||
Alkaline Phosphatase (units/L)—median (IQR) | 77 [62, 97] | 76 [61, 96] | 87 [68, 118] | 90 [68, 127] | ||
White Blood Cell Count (K/uL)—median (IQR) | 7.40 [5.90, 9.40] | 7.30 [5.90, 9.30] | 8.50 [6.51, 11.40] | 10.0 [7.30, 14.14] | ||
Hematocrit (volume %)—median (IQR) | 40.0 [36.5, 42.9] | 40.0 [36.8, 43.0] | 35.0 [30.5, 39.2] | 32.3 [28.2, 37.1] | ||
Platelet Count (K/uL)—median (IQR) | 241 [198, 291] | 241 [198, 290] | 236 [182, 306] | 234 [167, 319] | ||
International Normalized Ratio of Prothrombin Time values—median (IQR) | 1.0 [1.0, 1.1] | 1.0 [1.0, 1.1] | 1.1 [1.0, 1.2] | 1.2 [1.1, 1.4] | ||
Appendix 2: Missingness Rates
Count | Proportion | |
|---|---|---|
Age | 24,622 | 0.38% |
Sex | 4014 | 0.06% |
Race | 16,386 | 0.25% |
Height | 130,609 | 2.01% |
Weight | 69,082 | 1.07% |
Work Relative Value Unit | 5742 | 0.09% |
In/outpatient | 4 | < 0.00% |
Transfer Status | 5711 | 0.09% |
Anesthesia | 1545 | 0.02% |
Surgical Service | 1 | < 0.00% |
Emergency | 32 | < 0.00% |
Wound Classification | 5 | < 0.00% |
ASA Classification | 19,173 | 0.30% |
Diabetes | 8 | < 0.00% |
Smoke | 25 | < 0.00% |
Dyspnea | 30 | < 0.00% |
Functional Status | 37,040 | 0.57% |
Ventilator | 11 | < 0.00% |
History of Chronic Obstructive Pulmonary Disease | 13 | < 0.00% |
Ascites | 20 | < 0.00% |
History of Congestive Heart Failure | 13 | < 0.00% |
Hypertension | 16 | < 0.00% |
Preoperative Acute Renal Failure | 19 | < 0.00% |
Dialysis | 24 | < 0.00% |
Disseminated Cancer | 17 | < 0.00% |
Open Wound/Wound Infection | 17 | < 0.00% |
Steroid | 17 | < 0.00% |
Weight Loss | 18 | < 0.00% |
Bleeding Disorder | 15 | < 0.00% |
Preop Transfusion | 20 | < 0.00% |
Systemic Sepsis | 12,281 | 0.19% |
Operation Time | 945 | 0.01% |
Hospital Length of Stay | 5683 | 0.09% |
Days from Admission to Surgery | 239 | < 0.00% |
Return to Operating Room | 55 | < 0.00% |
Serum Sodium | 1,232,739 | 19.01% |
Blood Urea Nitrogen | 1,416,070 | 21.84% |
Serum Creatinine | 1,186,261 | 18.30% |
Serum Albumin | 3,150,009 | 48.59% |
Total Bilirubin | 3,151,874 | 48.61% |
Serum Glutamic Oxaloacetic Transaminase | 3,145,901 | 48.52% |
Alkaline Phosphatase | 3,131,423 | 48.30% |
White Blood Cell Count | 1,033,486 | 15.94% |
Hematocrit | 942,893 | 14.54% |
Platelet Count | 1,037,770 | 16.01% |
Partial Thromboplastin Time | 4,278,329 | 65.99% |
International Normalized Ratio (INR) of Prothrombin Time values | 3,732,736 | 57.57% |
Prothrombin Time | 5,809,086 | 89.60% |
Appendix 3: Totally Dependent Patients with Unplanned Intubation Cohort Summary
Lived | Died | ||
|---|---|---|---|
Count (%) | 2112 (5.4) | 1326 (7.2) | |
Sex = Female (%) | 945 (44.8) | 618 (46.6) | |
Age (years)—median (IQR) | 65 [54, 75] | 72 [61, 81] | |
Weight (kg)—median (IQR) | 76 [63, 94] | 71 [59, 87] | |
Wound Classification (%) | 1 – Clean | 560 (26.5) | 372 (28.1) |
2 – Clean/ Contaminated | 510 (24.1) | 299 (22.5) | |
3 – Contaminated | 328 (15.5) | 210 (15.8) | |
4 – Dirty/Infected | 714 (33.8) | 445 (33.6) | |
ASA Class (%) | 1 | 1 (0.0) | 1 (0.1) |
2 | 38 (1.8) | 13 (1.0) | |
3 | 677 (32.1) | 379 (28.6) | |
4/5 | 1391 (66.0) | 933 (70.4) | |
Diabetes (%) | 0 – No | 1492 (70.6) | 896 (67.6) |
1 – Insulin | 398 (18.8) | 286 (21.6) | |
2 – Non-Insulin | 222 (10.5) | 144 (10.9) | |
Dyspnea (%) | 0 – No | 1420 (67.2) | 872 (65.8) |
1 – At Rest | 462 (21.9) | 297 (22.4) | |
2 – Moderate Exertion | 230 (10.9) | 157 (11.8) | |
Sepsis (%) | 0 – None | 750 (35.5) | 478 (36.1) |
1 – Systemic Inflammatory Response Syndrome (SIRS) | 403 (19.1) | 270 (20.4) | |
2 – Sepsis | 312 (14.8) | 269 (20.3) | |
3 – Septic Shock | 646 (30.6) | 307 (23.2) | |
Outpatient (%) | 14 (0.7) | 14 (1.1) | |
Transfer Status = Admitted from other (%) | 927 (43.9) | 624 (47.1) | |
Emergency (%) | 1144 (54.2) | 662 (49.9) | |
Smoker (%) | 474 (22.4) | 250 (18.9) | |
Ventilator Dependent (%) | 863 (40.9) | 352 (26.5) | |
History of Severe Chronic Obstructive Pulmonary Disease (%) | 373 (17.7) | 251 (18.9) | |
Ascites (%) | 174 (8.2) | 138 (10.4) | |
History of Congestive Heart Failure (%) | 282 (13.4) | 205 (15.5) | |
Hypertension Requiring Medication (%) | 1384 (65.5) | 936 (70.6) | |
Acute Renal Failure (%) | 182 (8.6) | 109 (8.2) | |
Dialysis (%) | 225 (10.7) | 241 (18.2) | |
Disseminated Cancer (%) | 62 (2.9) | 85 (6.4) | |
Open Wound/Wound Infection (%) | 678 (32.1) | 526 (39.7) | |
Steroid Use for Chronic Condition (%) | 200 (9.5) | 176 (13.3) | |
Weight Loss (%) | 141 (6.7) | 136 (10.3) | |
Bleeding Disorder (%) | 497 (23.5) | 352 (26.5) | |
Transfusion (%) | 268 (12.7) | 180 (13.6) | |
Return to Operating Room = Yes (%) | 743 (35.2) | 315 (23.8) | |
Superficial Incisional Surgical Site Infection (%) | 112 (5.3) | 33 (2.5) | |
Deep Incisional Surgical Site Infection (%) | 70 (3.3) | 33 (2.5) | |
Organ Space Surgical Site Infection (%) | 168 (8.0) | 76 (5.7) | |
Wound Disruption (%) | 95 (4.5) | 53 (4.0) | |
Pneumonia (%) | 959 (45.4) | 494 (37.3) | |
Unplanned Intubation (%) | 2112 (100.0) | 1326 (100.0) | |
Pulmonary Embolism (%) | 59 (2.8) | 30 (2.3) | |
Progressive Renal Insufficiency (%) | 85 (4.0) | 53 (4.0) | |
Acute Renal Failure (%) | 168 (8.0) | 137 (10.3) | |
Urinary Tract Infection (%) | 264 (12.5) | 115 (8.7) | |
Stroke/Cerebrovascular Accident (%) | 62 (2.9) | 49 (3.7) | |
Cardiac Arrest (%) | 174 (8.2) | 472 (35.6) | |
Myocardial Infarction (%) | 71 (3.4) | 87 (6.6) | |
Transfusions (%) | 472 (22.3) | 349 (26.3) | |
Deep Vein Thrombosis Requiring Therapy (%) | 186 (8.8) | 69 (5.2) | |
Sepsis (%) | 393 (18.6) | 156 (11.8) | |
Septic Shock (%) | 614 (29.1) | 527 (39.7) | |
Rights and permissions
About this article
Cite this article
Clifton, J.C., Engoren, M., Shotwell, M.S. et al. The Impact of Functional Dependence and Related Surgical Complications on Postoperative Mortality. J Med Syst 46, 6 (2022). https://doi.org/10.1007/s10916-021-01779-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-021-01779-8