Abstract
S-nitrosylation (SNO) is a covalent post-translational oxidative modification. The reaction is the nitroso group (–NO) to a reactive cysteine thiol within a protein to form the SNO. In recent years, a variety of proteins in human body have been found to undergo thiol nitrosylation under specific conditions. Protein SNO, which is closely related to cardiovascular disease, Parkinson’s syndrome, Alzheimer’s disease and tumors, plays an important role in regulatory mechanism of protein function in both physiological and pathological pathways, such as in cellular homeostasis and metabolism. This review discusses possible molecular mechanisms protein SNO modification, such as the role of NO in vivo and the formation mechanism of SNO, with particular emphasis on mechanisms utilized by SNO to cause certain diseases of human. Importantly, the effect of SNO on diseases is multifaceted and multi-channel, and its critical value in vivo is not well defined. Intracellular redox environment is also a key factor affecting its level. Therefore, we should pay more attention to the equilibrium relationship between SNO and denitrosylation pathway in the future researches. These findings provide theoretical support for the improvement or treatment of diseases from the point of view of SNO.





Similar content being viewed by others
References
Calabrese V, Cornelius C, Rizzarelli E, Owen JB, Dinkova-Kostova AT, Butterfield DA (2009) Nitric oxide in cell survival: a janus molecule. Antioxid Redox Signal 11:2717–2739
Liu L, Yan Y, Zeng J, Hanes MA, Ahearn G, McMahon TJ, Dickfeld T, Marshall HE, Que LG, Stamler JS (2004) Essential roles of S-nitrosothiols in vascular homeostasis and endotoxic shock. Cell 116:617–628
Baldelli S, Ciriolo MR (2016) Altered S-nitrosylation of p53 is responsible for impaired antioxidant response in skeletal muscle during aging. Aging 8:3450–3467
Valek L, Heidler J, Scheving R, Wittig I, Tegeder I (2019) Nitric oxide contributes to protein homeostasis by S-nitrosylations of the chaperone HSPA8 and the ubiquitin ligase UBE2D. Redox Biol 20:217–235
Wu BW (2016) Peroxiredoxin-2 nitrosylation facilitates cardiomyogenesis of mouse embryonic stem cells via XBP-1s/PI3K pathway. Free Radic Biol Med 97:179–219
DelaTorre A, Schroeder RA, Kuo PC (1997) Alteration of NF-kappa B p50 DNA binding kinetics by S-nitrosylation. Biochem Biophys Res Commun 238:703–706
Li J (2016) Nitrosylated proteasome degradation pathway can inhibit the activity of cell cycle dependent protein kinase 5. Adv Physiol Sci 47:239
Yang HN, Yan XQ, Lv LX, Han D, Hu SQ, Xu T (2019) Study on the mechanism of kainic acid-induced denitrosylation of Procaspase 3 in rat hippocampus CA1 region. Med J Commun 5:433–437
Mannick JB, Hausladen A, Liu LM, Hess DT, Zeng M, Miao QX, Kane LS, Gow AJ, Stamler JS (1999) Fas-induced caspase denitrosylation. Science 284:651–654
Mannick JB, Schonhoff CM, Papeta N, Ghafourifar P, Szibor M, Fang K, Gaston B (2001) S-Nitrosylation of mitochondrial caspases. J Cell Biol 154:1111–1116
Matsushita K, Morrell CN, Cambien B, Yang SX, Yamakuchi M, Bao C, Hara MR, Quick RA, Cao W, O’Rourke B, Lowenstein JM, Pevsner J, Wagner DD, Lowenstein CJ (2003) Nitric oxide regulates exocytosis by S-nitrosylation of N-ethylmaleimide-sensitive factor. Cell 115:139–150
Han T, Tang Y, Li J, Xue B, Gong L, Yu X, Liu C (2017) Nitric oxide donor protects against acetic acid-induced gastric ulcer in rats via S-nitrosylation of TRPV1on vagus nerve. Sci Rep 7:1898
Kawashima S, Yokoyama M (2004) Dysfunctuon of endothelial nitric oxide synthase and atherosclerosis. Arterioscler Thromb Vasc Biol 24:998–1005
Li J, Feng J, Wang X (2017) Regulation of vascular function by nitric oxide-related S-nitrosylation. Acta Physiol Sin 69:557–570
Calabrese V, Mancuso C, Calvani M, Rizzarelli E, Butterfield DA, Giuffrida Stella AM (2007) Nitric oxide in the central nervous system: neuroprotection versus neurotoxicity. Nat Neurosci 8:766–775
Murad F (1986) Cyclic guanosine-monophosphate as a mediator of vasodilation. J Clin Investig 78:1–5
Gonzalez DR, Treuer A, Sun QA, Stamler JS, Hare JM (2009) S-nitrosylation of cardiac ion channels. J Cardiovasc Pharmacol 54:188–195
Benhar M, Forrester MT, Stamler JS (2009) Protein denitrosylation: enzymatic mechanisms and cellular functions. Nat Rev Mol Cell Biol 10:721–732
Calabrese V, Cornelius C, Dinkova-Kostova AT, Calabrese EJ, Mattson MP (2010) Cellular stress responses, the hormesis paradigm, and vitagenes: novel targets for therapeutic intervention in neurodegenerative disorders. Antioxid Redox Signal 13:1763–1811
Stamler JS (1994) Redox signaling: nitrosylation and related target interactions of nitric oxide. Cell 78:931–936
Hess DT, Matsumoto A, Kim SO, Marshall HE, Stamler JS (2005) Protein S-nitrosylation: purview and parameters. Nat Rev Mol Cell Biol 6:150–166
Liang J, Cheng SL, Hou J, Xu Z, Zhao YL (2012) Car-Parinello molecular dynamics simulations of thionitroxide and S-nitrosothiol in the gas phase, methanol, and water—a theoretical study of S-nitrosylation. Sci China Chem 55:2081–2088
Hogg N (1999) The kinetics of S-transnitrosation—a reversible second-order reaction. Anal Biochem 272:257–262
Shi T, Chen M, Chen XP, Wang JT, Wan AJ, Zhao YL (2015) Molecular mechanism of protein S-nitrosylation and its disease correlation. Prog Chem 5:594–600
Duan S, Chen C (2007) S-nitrosylation/denitrosylation and apoptosis of immune cells. Cell Mol Immunol 4:353–358
Lima B, Forrester MT, Hess DT, Stamler JS (2010) S-nitrosylation in cardiovascular signaling. Cric Res 106:633–646
Forrester MT, Foster MW, Stamler JS (2007) Assessment and application of the biotin switch technique for examining protein S-nitrosylation under conditions of pharmacologically induced oxidative stress. J Biol Chem 282:13977–13983
Cao Y, Gomes SA, Rangel EB, Paulino EC, Fonseca TL, Li JL, Teixeira MB, Gouveia CHA, Bianco AC, Kapiloff MS, Balkan W, Hare JM (2015) S-nitrosoglutathione reductase–dependent PPARγ denitrosylation participates in MSC-derived adipogenesis and osteogenesis. J Clin Investig 125:1679–1691
Sengupta R, Ryter SW, Zuckerbraun BS, Tzeng E, Billiar TR, Stoyanovsky DA (2007) Thioredoxin catalyzes the denitrosation of low-molecular mass and protein S-nitrosothiols. Biochemistry 46:8472–8483
Stoyanovsky DA, Tyurina YY, Tyurin VA, Anand D, Mandavia DN, Gius D, Ivanova J, Pitt B, Billiar TR, Kagan VE (2005) Thioredoxin and lipoic acid catalyze the denitrosation of low molecular weight and protein S-nitrosothiols. J Am Chem Soc 127:15815–15823
Kelleher ZT, Sha Y, Foster MW, Foster WM, Forrester MT, Marshall HE (2014) Thioredoxin-mediated denitrosylation regulates cytokine-induced nuclear factor κB (NF-κB) activation. J Biol Chem 289:3066–3072
Chen YL, Liu RH, Zhang GW, Yu Q, Jia M, Zheng C, Wang YL, Xu CB, Zhang YP, Liu EQ (2015) Hypercysteinemia promotes atherosclerosis by reducing protein S-nitrosylation. Biomed Pharmacother 70:253–259
Li J, Zhang Y, Zhang YY, Lu SL, Miao YT, Yang J, Huang SM, Ma XL, Han LL, Deng JC, Fan FF, Liu B, Huo Y, Xu QB, Chen C, Wang X, Feng J (2018) GSNOR modulates hyperhomocysteinemia-induced T cell activation and atherosclerosis by switching Akt S-nitrosylation to phosphorylation. Redox Biol 17:386–399
Jankov RP, Daniel KL, Iny S, Kantores C, Ivanovska J, Fadel NB, Jain A (2018) Sodium nitrite augments lung S-nitrosylation and reverses chronic hypoxic pulmonary hypertension in juvenile rats. Am J Physiol Lung Cell Mol Physiol 315:L742–L751
Jiang H, Song N, Wang J, Ren LY, Xie JX (2007) Peripheral iron dextran induced degeneration of dopaminergic neurons in rat substantia nigra. Neurochem Int 51:32–36
Roth JA, Singleton S, Feng J, Garrick M, Paradkar PN (2010) Parkin regulates metal transport via proteasomal degradation of the 1B isoforms of divalent metal transporter 1. J Neurochem 113:454–464
Bi MX, Du XX, Jiao Q, Liu ZG, Jiang H (2020) α-Synuclein regulates iron homeostasis via preventing parkin-mediated DMT1 ubiquitylation in Parkinson’s disease models. ACS Chem Neurosci 11:1682–1691
Liu C, Zhang CW, Lo SQ, Ang ST, Chew KCM, Yu DJ, Chai BH, Tan B, Tsang F, Tai YK, Tan BWQ, Liang MC, Tan HT, Tang JY, Lai MKP, Chua JJE, Chung MCM, Khanna S, Lim K, Soong TW (2018) S-nitrosylation of divalent metal transporter 1 enhances iron uptake to mediate loss of dopaminergic neurons and motoric deficit. J Neurosci 38:8364–8377
Yao DD, Gu ZZ, Nakamura T, Shi ZQ, Ma YL, Gaston B, Palmer LA, Rockenstein E, Zhang ZH, Masliah E, Uehara T, Lipton SA (2004) Nitrosative stress linked to sporadic Parkinson’s disease: S-nitrosylation of parkin regulates its E3 ubiquitin ligase activity. Proc Natl Acad Sci USA 101:10810–10814
Yin L, Xie YY, Yin SY, Lv XL, Zhang J, Gu ZZ, Sun HD, Liu SQ (2015) The S-nitrosylation status of PCNA localized in cytosol impacts the apoptotic pathway in a Parkinson’s disease paradigm. PLoS One 10:e0117546
Calabrese V, Santoro A, Monti D, Crupi R, Di Paola R, Latteri S, Cuzzocrea S, Zappia M, Giordano J, Calabrese EJ, Franceschi C (2018) Aging and Parkinson’s disease: inflammaging, neuroinflammation and biological remodeling as key factors in pathogenesis. Free Radic Biol Med 115:80–91
Kumar R, Jangir DK, Verma G, Shekhar S, Hanpude P, Kumar S, Kumari R, Singh N, Bhavesh NS, Jana NR, Maiti TK (2017) S-nitrosylation of UCHL1 induces its structural instability and promotes α-synuclein aggregation. Sci Rep 7:44558
Hedrich K, Djarmati A, Schafer N, Hering R, Wellenbrock C, Weiss PH, Hilker R, Vieregge P, Ozelius LJ, Heutink P, Bonifati V, Schwinger E, Lang AE, Noth J, Bressman S, Pramstaller PP, Riess O, Klein C (2004) DJ-1 (PARK7) mutations are less frequent than Parkin (PARK2) mutations in early-onset Parkinson disease. Neurology 62:389–394
Kumar R, Kumari R, Kumar S, Jangir DK, Maiti TK (2018) Extracellular α-synuclein disrupts membrane nanostructure and promotes S-nitrosylation induced neuronal cell death. Biomacromolecules 19:1118–1129
Oh C, Sultan A, Platzer J, Dolatabadi N, Soldner F, Mcclatchy DB, Diedrich JK, Yates JR, Ambasudhan R, Nakamura T, Jaenisch R, Lipton SA (2017) S-nitrosylation of PINK1 attenuates PINK1/Parkin dependent mitophagy in hiPSC-based Parkinson’s disease models. Cell Rep 21:2171–2182
Wilkaniec A, Lenkiewicz AM, Czapski GA, Jeśko H, Hilgier W, Brodzik R, Gąssowskadobrowolska M, Culmsee C, Adamczyk A (2019) Extracellular alpha-synuclein oligomers induce Parkin S-nitrosylation: relevance to sporadic Parkinson’s disease etiopathology. Mol Neurobiol 56:125–140
Zhang ZZ, Liu L, Jiang XX, Zhai SD, Xing D (2016) The essential role of Drp1 and its regulation by S-nitrosylation of Parkin in dopaminergic neurodegeneration: implications for Parkinson’s disease. Antioxid Redox Signal 25:609–622
Ryu I, Lee K, Do S (2016) Aβ-affected pathogenic induction of S-nitrosylation of OGT and identifification of Cys-NO linkage triplet. Biochim Biophys Acta 1864:609–621
Masliah E (1995) Mechanisms of synaptic dysfunction in Alzheimer’s disease. Histol Histopathol 10:509–519
Scheff SW, Price DA, Schmitt FA, Mufson EJ (2006) Hippocampal synaptic loss in early Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging 27:1372–1384
Langston JW, Ballard P, Tetrud JW, Irwin I (1983) Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science 219:979–980
Nakamura T, Lipton SA (2017) ‘SNO’-storms compromise protein activity and mitochondrial metabolism in neurodegenerative disorders. Trends Endocrinol Metab 28:879–892
Bak DW, Pizzagalli MD, Weerapana E (2017) Identifying functional cysteine residues in the mitochondria. ACS Chem Biol 12:947–957
Chouchani ET, Hurd TR, Nadtochiy SM, Brookes PS, Fearnley IM, Lilley KS, Smith RA, Murphy MP (2010) Identification of S-nitrosated mitochondrial proteins by S-nitrosothiol difference in gel electrophoresis (SNO-DIGE): implications for the regulation of mitochondrial function by reversible S-nitrosation. Biochem J 430:49–59
Doulias PT, Tenopoulou M, Greene JL, Raju K, Ischiropoulos H (2013) Nitric oxide regulates mitochondrial fatty acid metabolism through reversible protein S-nitrosylation. Sci Signal 6:rs1
Lee YI, Giovinazzo D, Kang HC, Lee Y, Jeong JS, Doulias PT, Xie Z, Hu J, Ghasemi M, Ischiropoulos H, Qian J, Zhu H, Blackshaw S, Dawson VL, Dawson TM (2014) Protein microarray characterization of the S-nitrosoproteome. Mol Cell Proteom 13:63–72
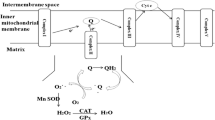
Piantadosi CA (2012) Regulation of mitochondrial processes by protein S-nitrosylation. Biochem Biophys Acta 1820:712–721
Seneviratne U, Nott A, Bhat VB, Ravindra KC, Wishnok JS, Tsai LH, Tannenbaum SR (2016) S-nitrosation of proteins relevant to Alzheimer’s disease during early stages of neurodegeneration. Proc Natl Acad Sci USA 113:4152–4157
Sun J, Morgan M, Shen RF, Steenbergen C, Murphy E (2007) Preconditioning results in S-nitrosylation of proteins involved in regulation of mitochondrial energetics and calcium transport. Circ Res 101:1155–1163
Bubber P, Haroutunian V, Fisch G, Blass JP, Gibson GE (2005) Mitochondrial abnormalities in Alzheimer brain: mechanistic implications. Ann Neurol 57:695–703
Xu PF, Ye SY, Li KY, Huang MQ, Wang QL, Zeng SS, Chen X, Gao WW, Chen JP, Zhang QB, Zhong Z, Lin Y, Rong ZL, Xu Y, Hao BT, Peng AH, Ouyang MZ, Liu QZ (2019) NOS1 inhibits the interferon response of cancer cells by S-nitrosylation of HDAC2. J Exp Clin Cancer Res 38:1–16
Laurence Z, Lorenzo G, Oliver K, Smyth MJ, Guido K (2015) Type I interferons in anticancer immunity. Nat Rev Immunol 15:405–414
Minn AJ (2015) Interferons and the immunogenic effects of cancer therapy. Trends Immunol 36:725–737
Yilmaz M, Christofori G (2009) EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastasis Rev 28:15–33
Bukholm IRK, Nesland JM, Karesen R, Jacobsen U, Borresendale AL (1998) E-cadherin and α-, β-, and γ-catenin protein expression in relation to metastasis in human breast carcinoma. J Pathol 185:262–266
Bajpai S, Feng YF, Krishnamurthy R, Longmore GD, Wirtz D (2009) Loss of alpha-catenin decreases the strength of single E-cadherin bonds between human cancer cells. J Biol Chem 284:18252–18259
Yoshida R, Kimura N, Harada Y, Ohuchi N (2001) The loss of E-cadherin, α- and β-catenin expression is associated with metastasis and poor prognosis in invasive breast cancer. Int J Oncol 18:513–520
Basudhardebashree S, Almeida DO, Kesarwalaaparna HL, Chengrobert YS, Glynnsharon A, Ambsstefan WA, Ridnourlisa A (2017) Nitric oxide synthase-2-derived nitric oxide drives multiple pathways of breast cancer progression. Antioxid Redox Signal 26:1044–1058
Switzer CH, Glynn SA, Cheng RYS, Ridnour LA, Green JE, Ambs S, Wink DA (2012) S-nitrosylation of EGFR and Src activates an oncogenic signaling network in human basal-like breast cancer. Mol Cancer Res 10:1203–1215
Zhou SL, Han QL, Wang R, Li X, Wang QY, Wang HZ, Wang J, Ma YF (2016) PRDX2 protects hepatocellular carcinoma SMMC-7721 cells from oxidative stress. Oncol Lett 12:2217–2221
Mullen L, Hanschmann EM, Lillig CH, Herzenberg LA, Ghezzi P (2015) Cysteine oxidation targets peroxiredoxins 1 and 2 for exosomal releasethrough a novel mechanism of redox-dependent secretion. Mol Med 21:98–108
Saito S, Furuno A, Sakurai J, Park H, Shinya K, Tomida A (2012) Compound C prevents the unfolded protein response during glucose deprivation through a mechanism independent of AMPK and BMP signaling. PLoS One 7:e45845
Lee CW, Wong LL, Tse EYT, Liu HF, Leong VY, Lee JM, Hardie DG, Ng IO, Ching Y (2012) AMPK promotes p53 acetylation via phosphorylation and inactivation of SIRT1 in liver cancer cells. Can Res 72:4394–4404
Zhang YH, Sun CN, Xiao GK, Shan H, Tang LY, Yi YJ, Yu WG, Gu YC (2019) S-nitrosylation of the Peroxiredoxin-2 promotes S-nitrosoglutathione-mediated lung cancer cells apoptosis via AMPK-SIRT1 pathway. Cell Death Dis 10:329
Pan LH, Lin Z, Tang X, Tian JX, Zheng Q, Jing J, Xie LP, Chen HS, Lu QL, Wang H, Li QG, Han Y, Ji Y (2020) S-nitrosylation of plastin-3 exacerbates thoracic aortic dissection formation via endothelial barrier dysfunction. Arterioscler Thromb Vasc Biol 40:175–188
Hoffman EP, Brown RH, Kunkel LM (1987) Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell 51:919–928
Connuck DM, Sleeper LA, Colan SD, Cox GF, Towbin JA, Lowe AM, Wilkinson JD, Orav EJ, Cuniberti L, Salbert BA, Lipshultz SE (2008) Characteristics and outcomes of cardiomyopathy in children with Duchenne or Becker muscular dystrophy: a comparative study from the Pediatric Cardiomyopathy Registry. Am Heart J 155:998–1005
Lillo MA, Himelman E, Shirokova N, Xie LF, Fraidenraich D, Contreras JE (2019) S-nitrosylation of connexin43 hemichannels elicits cardiac stress-induced arrhythmias in Duchenne muscular dystrophy mice. JCI Insight 4:e130091
Dai Y, Wang H, Ogawa A, Yamanaka H, Obata K, Tokunaga A, Noguchi K (2005) Ca2+/calmodulin-dependent protein kinase II in the spinal cord contributes to neuropathic pain in a rat model of mononeuropathy. Eur J Neurosci 21:2467–2474
Coultrap SJ, Buard I, Kulbe JR, Dell'Acqua ML, Bayer KU (2010) CaMKII Autonomy is substrate-dependent and further stimulated by Ca(2+)/calmodulin. J Biol Chem 285:17930–17937
Song T, Hatano N, Kambe T, Miyamoto Y, Ihara H, Yamamoto H, Sugimoto K, Kume K, Yamaguchi F, Tokuda M, Watanabe Y (2008) Nitric oxide-mediated modulation of calcium/calmodulin-dependent protein kinase II. Biochem J 412:223–231
Coultrap SJ, Bayer KU (2014) Nitric oxide induces Ca2+-independent activity of the Ca2+/calmodulin-dependent protein kinase II (CaMKII). J Biol Chem 289:19458–19465
Coultrap SJ, Zaegel V, Bayer KU (2014) CaMKII isoforms differ in their specific requirements for nitric oxide regulation. FEBS Lett 588:4672–4676
Calabrese V, Santoro A, Salinaro AT, Modafferi S, Scuto M, Albouchi F, Monti D, Giordano J, Zappia M, Franceschi C, Calabrese EJ (2018) Hormetic approaches to the treatment of Parkinson’s disease: perspectives and possibilities. J Neurosci Res 96:1641–1662
Pilipenko V, Narbute K, Amara I, Trovato A, Scuto M, Pupure J, Jansone B, Poikans J, Bisenieks E, Klusa V, Calabrese V (2019) GABA-containing compound gammapyrone protects against brain impairments in Alzheimer’s disease model male rats and prevents mitochondrial dysfunction in cell culture. J Neurosci Res 97:708–726
Peters V, Calabrese V, Forsberg E, Volk N, Fleming T, Baelde H, Weigand T, Thiel C, Trovato A, Scuto M, Modafferi S, Schmitt CP (2018) Protective actions of anserine under diabetic conditions. Int J Mol Sci 19:2751
Singh AP, Singh R, Verma SS, Rai V, Kaschula CH, Maiti P, Gupta SC (2019) Health benefits of resveratrol: evidence from clinical studies. Med Res Rev 39:1851–1891
Di Rosa G, Brunetti G, Scuto M, Salinaro AT, Calabrese EJ, Crea R, Schmitz-Linneweber C, Calabrese V, Saul N (2020) Healthspan enhancement by olive polyphenols in C. elegans wild type and Parkinson’s models. Int J Mol Sci 21:3893
Brunetti G, Di Rosa G, Scuto M, Leri M, Stefani M, Schmitz-Linneweber C, Calabrese V, Saul N (2020) Healthspan maintenance and prevention of Parkinson’s-like phenotypes with hydroxytyrosol and oleuropein aglycone in C. elegans. Int J Mol Sci 21:2588
Leri M, Scuto M, Ontario ML, Calabrese V, Calabrese EJ, Bucciantini M, Stefani M (2020) Healthy effects of plant polyphenols: molecular mechanisms. Int J Mol Sci 21:1250
Neurauter G, Schrocksnadel K, Scholl-Burgi S, Sperner-Unterweger B, Schubert C, Ledochowski M, Fuchs D (2008) Chronic immune stimulation correlates with reduced phenylalanine turnover. Curr Drug Metab 9:622–627
Miquel S, Champ C, Day J, Aarts E, Bahr BA, Bakker M, Bánáti D, Calabrese V, Cederholm T, Cryan J, Dye L, Farrimon JA, Korosi A, Layé S, Maudsley S, Milenkovic D, Mohajeri MH, Sijben J, Solomon A, Spencer JPE, Thuret S, Berghe WV, Vauzour D, Vellas B, Wesnes K, Willatts P, Wittenberg R, Geurts L (2017) Poor cognitive ageing: vulnerabilities, mechanisms and the impact of nutritional interventions. Ageing Res Rev 42:40–55
Stebbing ARD (1982) Hormesis—the stimulation of growth by low-levels of inhibitors. Sci Total Environ 22:213–234
Navarro A, Boveris A (2008) Mitochondrial nitric oxide synthase, mitochondrial brain dysfunction in aging, and mitochondria-targeted antioxidants. Adv Drug Deliv Rev 60:1534–1544
Calabrese EJ, Calabrese V, Tsatsakis A, Giordano JJ (2020) Hormesis and Ginkgo biloba (GB): numerous biological effects of GB are mediated via hormesis. Ageing Res Rev 10:101019
Acknowledgements
The authors gratefully acknowledge the financial support of National Natural Science Foundation of China (31701531), Hebei Natural Science Foundation (C2018201146), and One Province One School Project of China.
Author information
Authors and Affiliations
Contributions
Writing—original draft preparation, YZ and YD; writing—review and editing, YL, HX and XY; supervision, YL. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Deng, Y., Yang, X. et al. The Relationship Between Protein S-Nitrosylation and Human Diseases: A Review. Neurochem Res 45, 2815–2827 (2020). https://doi.org/10.1007/s11064-020-03136-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-03136-6