Abstract
Purpose
The encapsulation of pancreatic β-cells in biocompatible matrix has generated great interest in diabetes treatment. Our work has shown improved microcapsules when incorporating the bile acid ursodeoxycholic acid (UDCA), in terms of morphology and cell viability although cell survival remained low. Thus, the study aimed at incorporating the polyelectrolytes polyallylamine (PAA) and poly-l-ornithine (PLO), with the polymer sodium alginate (SA) and the hydrogel ultrasonic gel (USG) with UDCA and examined cell viability and functionality post microencapsulation.
Methods
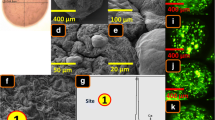
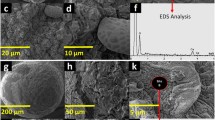
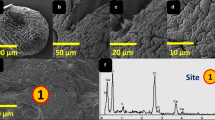
Microcapsules without (control) and with UDCA (test) were produced using 1% PLO, 2.5% PAA, 1.8% SA and 4.5% USG. Pancreatic β-cells were microencapsulated and the microcapsules’ morphology, surface components, cellular and bile acid distribution, osmotic and mechanical stability as well as biocompatibilities, insulin production, bioenergetics and the inflammatory response were tested.
Results
Incorporation of UDCA at 4% into a PLO-PAA-SA formulation system increased cell survival (p < 0.01), insulin production (p < 0.01), reduced the inflammatory profile (TNF-α, IFN-ϒ, IL-6 and IL-1β; p < 0.01) and improved the microcapsule physical and mechanical strength (p < 0.01).
Conclusions
β-cell microencapsulation using 1% PLO, 2.5% PAA, 1.8% SA, 4.5% USG and the bile acid UDCA (4%) has good potential in cell transplantation and diabetes treatment.




Similar content being viewed by others
Change history
27 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11095-021-03142-5
Abbreviations
- ACMT:
-
Artificial cell microencapsulation technology
- ATPP:
-
Adenosine triphosphate production
- BR:
-
Basal respiration
- CBA:
-
Cytokine bead array
- CE:
-
Coupling efficiency
- DM:
-
Diabetes mellitus
- DMEM:
-
Dulbecco’s modified eagle’s medium
- ECAR:
-
Extracellular acidification rate
- EDXR:
-
Energy dispersive x-ray spectroscopy
- ELISA:
-
Enzyme-linked immunosorbent assay
- G:
-
Glycolysis
- IFN-γ:
-
Interferon-γ
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- MR:
-
Maximal respiration
- MTT:
-
(3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide)
- NGD-ECAR:
-
Non-glucose-derived extracellular acidification rate
- OCR:
-
Oxygen consumption rate
- OM:
-
Optical microscopy
- PAA:
-
Polyallylamine
- PL:
-
Proton leak
- PLO:
-
Poly-l-ornithine
- PPR:
-
Proton production rate
- SA:
-
Sodium alginate
- SEM:
-
Scanning electron microscopy
- SRC:
-
Spare respiratory capacity
- T1D:
-
Type 1 diabetes mellitus
- T2D:
-
Type 2 diabetes mellitus
- TNF-α:
-
Tumour necrosis factor-α
- TRITC:
-
Tetramethylrhodamine isothiocyanate
- UDCA:
-
Ursodeoxycholic acid
- USG:
-
Ultrasonic gel
References
Donath MY, Ehses JA, Maedler K, Schumann DM, Ellingsgaard H, Eppler E, et al. Mechanisms of β-cell death in type 2 diabetes. Diabetes. 2005;54 suppl 2:S108–13.
Vehik K, Dabelea D. The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev. 2011;27(1):3–13.
Negrulj R, Mooranian A, Al-Salami H. Potentials and limitations of bile acids in type 2 diabetes mellitus: applications of microencapsulation as a novel oral delivery system. J Endocrinol Diabetes Mellitus. 2013;1(2):49–59.
Beck J, Angus R, Madsen B, Britt D, Vernon B, Nguyen KT. Islet encapsulation: strategies to enhance islet cell functions. Tissue Eng. 2007;13(3):589–99.
Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365(9467):1333–46.
Sutherland DE. Current status of beta-cell replacement therapy (pancreas and islet transplantation) for treatment of diabetes mellitus. Transplant Proc. 2003;35(5):1625–7.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. Stability and release kinetics of an advanced gliclazide-cholic acid formulation: the use of artificial-cell microencapsulation in slow release targeted oral delivery of antidiabetics. J Pharm Innov. 2014;9:150–7.
Hafiz MM, Faradji RN, Froud T, Pileggi A, Baidal DA, Cure P, et al. Immunosuppression and procedure-related complications in 26 patients with type 1 diabetes mellitus receiving allogeneic islet cell transplantation. Transplantation. 2005;80(12):1718–28.
Steele JA, Halle JP, Poncelet D, Neufeld RJ. Therapeutic cell encapsulation techniques and applications in diabetes. Adv Drug Deliv Rev. 2014;67–68:74–83.
Lacík I. Polymer chemistry in diabetes treatment by encapsulated islets of Langerhans: review to 2006. Aust J Chem. 2006;59(8):508–24.
de Vos P, Lazarjani HA, Poncelet D, Faas MM. Polymers in cell encapsulation from an enveloped cell perspective. Adv Drug Deliv Rev. 2014;67–68:15–34.
Vaithilingam V, Tuch BE. Islet transplantation and encapsulation: an update on recent developments. Rev Diabet Stud. 2011;8(1):51–67.
Orive G, Maria Hernández R, Rodríguez Gascón A, Calafiore R, Swi Chang TM, Vos P, et al. History, challenges and perspectives of cell microencapsulation. Trends Biotechnol. 2004;22(2):87–92.
Schmidt JJ, Rowley J, Kong HJ. Hydrogels used for cell-based drug delivery. J Biomed Mater Res A. 2008;87(4):1113–22.
Bhatia SR, Khattak SF, Roberts SC. Polyelectrolytes for cell encapsulation. Curr Opin Colloid Interface Sci. 2005;10(1):45–51.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Arfuso F, Jones F, et al. Advanced bile acid-based multi-compartmental microencapsulated pancreatic beta-cells integrating a polyelectrolyte-bile acid formulation, for diabetes treatment. Artif Cells Nanomed Biotechnol. 2014;1–8.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Characterization of a novel bile acid-based delivery platform for microencapsulated pancreatic β-cells. Artif Cells Nanomed Biotechnol. 2016;44(1):194–200.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. The effect of a tertiary bile acid, taurocholic acid, on the morphology and physical characteristics of microencapsulated probucol: potential applications in diabetes: a characterization study. Drug Deliv and Transl Res. 2015;1–12.
Prakash S, Soe-Lin H. Strategy for cell therapy: polymers for live cell encapsulation and delivery. Trends Biomater Artif Organs. 2004;18(1):24–35.
Mooranian A, Negrulj R, Al-Salami H. The incorporation of water-soluble gel matrix into bile acid-based microcapsules for the delivery of viable β-cells of the pancreas, in diabetes treatment: biocompatibility and functionality studies. Drug Deliv and Transl Res. 2016;6(1):17–23.
Hamaguchi K, Gaskins HR, Leiter EH. NIT-1, a pancreatic beta-cell line established from a transgenic NOD/Lt mouse. Diabetes. 1991;40(7):842–9.
Mooranian A, Negrulj R, Mikov M, Golocorbin-Kon S, Arfuso F, Al-Salami H. Novel chenodeoxycholic acid-sodium alginate matrix in the microencapsulation of the potential antidiabetic drug, probucol. An in vitro study. J Microencapsul. 2015;32(6):589–97.
Mooranian A, Negrulj R, Chen-Tan N, Al-Sallami HS, Fang Z, Mukkur T, et al. Novel artificial cell microencapsulation of a complex gliclazide-deoxycholic bile acid formulation: a characterization study. Drug Des Dev Ther. 2014;8:1003.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. An advanced microencapsulated system: a platform for optimized oral delivery of antidiabetic drug-bile acid formulations. Pharm Dev Technol. 2015;20(6):702–9.
Sherman I, Fisher M. Hepatic transport of fluorescent molecules: in vivo studies using intravital TV microscopy. Hepatology. 1986;6(3):444–9.
Negrulj R, Mooranian A, Chen-Tan N, Al-Sallami HS, Mikov M, Golocorbin-Kon S, et al. Swelling, mechanical strength, and release properties of probucol microcapsules with and without a bile acid, and their potential oral delivery in diabetes. Artif Cells Nanomed Biotechnol. 2015;1–8.
Mooranian A, Negrulj R, Al-Sallami HS, Fang Z, Mikov M, Golocorbin-Kon S, et al. Release and swelling studies of an innovative antidiabetic-bile acid microencapsulated formulation, as a novel targeted therapy for diabetes treatment. J Microencapsul. 2015;32(2):151–6.
Uludag H, Sefton MV. Colorimetric assay for cellular activity in microcapsules. Biomaterials. 1990;11(9):708–12.
De Castro M, Orive G, Hernandez RM, Gascon AR, Pedraz JL. Comparative study of microcapsules elaborated with three polycations (PLL, PDL, PLO) for cell immobilization. J Microencapsul. 2005;22(3):303–15.
Bertolotti A, Borgogna M, Facoetti A, Marsich E, Nano R. The effects of alginate encapsulation on NIT-1 insulinoma cells: viability, growth and insulin secretion. In vivo. 2009;23(6):929–35.
Vaithilingam V, Kollarikova G, Qi M, Lacik I, Oberholzer J, Guillemin GJ, et al. Effect of prolonged gelling time on the intrinsic properties of barium alginate microcapsules and its biocompatibility. J Microencapsul. 2011;28(6):499–507.
Lee YY, Hong SH, Lee YJ, Chung SS, Jung HS, Park SG, et al. Tauroursodeoxycholate (TUDCA), chemical chaperone, enhances function of islets by reducing ER stress. Biochem Biophys Res Commun. 2010;397(4):735–9.
de Vos P, de Haan BJ, Kamps JA, Faas MM, Kitano T. Zeta-potentials of alginate-PLL capsules: a predictive measure for biocompatibility? J Biomed Mater Res A. 2007;80(4):813–9.
Labhasetwar VD, Dorle AK. A study on the zeta potential of microcapsules during ageing. J Microencapsul. 1991;8(1):83–5.
Xie HG, Li XX, Lv GJ, Xie WY, Zhu J, Luxbacher T, et al. Effect of surface wettability and charge on protein adsorption onto implantable alginate‐chitosan‐alginate microcapsule surfaces. J Biomed Mater Res A. 2010;92(4):1357–65.
Naldini A, Carraro F, Silvestri S, Bocci V. Hypoxia affects cytokine production and proliferative responses by human peripheral mononuclear cells. J Cell Physiol. 1997;173(3):335–42.
Zheng X, Zheng X, Wang X, Ma Z, Gupta Sunkari V, Botusan I, et al. Acute hypoxia induces apoptosis of pancreatic [beta]-cell by activation of the unfolded protein response and upregulation of CHOP. Cell Death Dis. 2012;3:e322.
Donath MY, Böni-Schnetzler M, Ellingsgaard H, Ehses JA. Islet inflammation impairs the pancreatic β-cell in type 2 diabetes. Physiology (Bethesda, Md). 2009;24:325–31.
Perez MJ, Briz O. Bile-acid-induced cell injury and protection. World J Gastroenterol. 2009;15(14):1677–89.
Kullmann F, Arndt H, Gross V, Ruschoff J, Scholmerich J. Beneficial effect of ursodeoxycholic acid on mucosal damage in trinitrobenzene sulphonic acid-induced colitis. Eur J Gastroenterol Hepatol. 1997;9(12):1205–11.
Martinez-Moya P, Romero-Calvo I, Requena P, Hernandez-Chirlaque C, Aranda CJ, Gonzalez R, et al. Dose-dependent antiinflammatory effect of ursodeoxycholic acid in experimental colitis. Int Immunopharmacol. 2013;15(2):372–80.
Amaral JD, Viana RJ, Ramalho RM, Steer CJ, Rodrigues CM. Bile acids: regulation of apoptosis by ursodeoxycholic acid. J Lipid Res. 2009;50(9):1721–34.
Takka S, Cali AG. Bile salt-reinforced alginate-chitosan beads. Pharm Dev Technol. 2012;17(1):23–9.
Lim F, Sun AM. Microencapsulated islets as bioartificial endocrine pancreas. Science. 1980;210(4472):908–10.
Dufrane D, Goebbels RM, Gianello P. Alginate macroencapsulation of pig islets allows correction of streptozotocin-induced diabetes in primates up to 6 months without immunosuppression. Transplantation. 2010;90(10):1054–62.
Mooranian A, Negrulj R, Al-Salami H. The effects of ionic gelation- vibrational jet flow technique in fabrication of microcapsules incorporating beta-cell: applications in type-1 diabetes. Curr Diabetes Rev. 2016. doi:10.2174/1573399812666151229101756.
Mooranian A, Negrulj R, Al-Salami H. Viability and topographical analysis of microencapsulated β-cells exposed to a biotransformed tertiary bile acid: an ex vivo study. Int J Nano Biomater. 2016;(in press). http://www.inderscience.com/info/ingeneral/forthcoming.php?jcode=ijnbm.
Mooranian A, Negrulj R, Morahan G, Jamieson E, Al-Salami H. Designing anti-diabetic β-cells microcapsules using polystyrenic sulfonate, polyallylamine and a tertiary bile acid: morphology, bioenergetics and cytokine analysis. Biotechnol Prog. 2016. doi:10.1002/btpr.2223.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors acknowledge Australian Postgraduate Award (APA) + Curtin Research Scholarship (CRS) for their support. The authors acknowledge the Curtin Health Innovation Research Institute for provision of laboratory space and technology platforms utilised in this study and also acknowledge the use of laboratory equipment, scientific and technical assistance of the Curtin University, Microscopy and Microanalysis Facility, which has been partially funded by the University, State and Commonwealth Governments. The authors also acknowledge the ARC Centre of Excellence in Plant Energy Biology (University of Western Australia) for training, support and access to equipment. The NIT-1 pancreatic mouse β-cells were a generous donation from Professor Grant Morahan at the University of Western Australia. The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised to correct Fig. 1.
Rights and permissions
About this article
Cite this article
Mooranian, A., Negrulj, R. & Al-Salami, H. The Influence of Stabilized Deconjugated Ursodeoxycholic Acid on Polymer-Hydrogel System of Transplantable NIT-1 Cells. Pharm Res 33, 1182–1190 (2016). https://doi.org/10.1007/s11095-016-1863-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-1863-y