Abstract
Purpose
Recently we demonstrated that microencapsulation of a murine pancreatic β-cell line using an alginate-ursodeoxycholic acid (UDCA) matrix produced microcapsules with good stability and cell viability. In this study, we investigated if translation of this formulation to microencapsulation of primary β-cells harvested from mature double-transgenic healthy mice would also generate stable microcapsules with good cell viability.
Methods
Islets of Langerhans were isolated from Ngn3-GFP/RIP-DsRED mice by intraductal collagenase P digestion and density gradient centrifugation, dissociated into single cells and the β-cell population purified by Fluorescence Activated Cell Sorting. β-cells were microencapsulated using either alginate-poly-l-ornithine (F1; control) or alginate-poly-l-ornithine-UDCA (F2; test) formulations. Microcapsules were microscopically examined and microencapsulated cells were analyzed for viability, insulin and cytokine release, 2 days post-microencapsulation.
Results
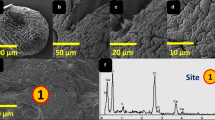
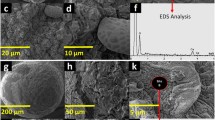
Microcapsules showed good uniformity and morphological characteristics and even cell distribution within microcapsules with or without UDCA. Two days post microencapsulation cell viability, mitochondrial ATP and insulin production were shown to be optimized in the presence of UDCA whilst production of the proinflammatory cytokine IL-1β was reduced. Contradictory to our previous studies, UDCA did not reduce production of any other pro-inflammatory biomarkers.
Conclusions
These results suggest that UDCA incorporation improves microcapsules’ physical and morphological characteristics and improves the viability and function of encapsulated mature primary pancreatic β-cells.




Similar content being viewed by others
Abbreviations
- ATP:
-
Adenosine triphosphate
- CMRL:
-
Connaught Medical Research Laboratories
- DAPI:
-
Diamidino-2-phenylindole
- FCS:
-
Fetal calf serum
- IFN-γ:
-
Interferon-γ
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- IL-12:
-
Interleukin-12
- IL-17:
-
Interleukin-17
- MTS:
-
3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H–tetrazolium
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- Ngn3-GFP:
-
Neurogenin3-Green fluorescent protein
- PBS:
-
Phosphate buffered saline
- PLO:
-
Poly-l-ornithine
- RIP-DsRED:
-
Rat insulin promoter-Discosoma sp. red fluorescent protein
- SA:
-
Sodium alginate
- TNF-α:
-
Tumor necrosis factor-α
- UDCA:
-
Ursodeoxycholic acid
- XTT:
-
2,3-Bis-(2-Methoxy-4-Nitro-5-Sulfophenyl)-2H–Tetrazolium-5-Carboxanilide
References
Fineberg SE, Anderson JH. Complications of insulin therapy. John Wiley & Sons, Ltd: International textbook of diabetes mellitus; 2003.
Bas VN, Cetinkaya S, Agladioglu SY, Kendirici HN, Bilgili H, Yildirim N, et al. Insulin oedema in newly diagnosed type 1 diabetes mellitus. J Clin Res Pediat Endocrinol. 2010;2(1):46–8.
Hirsch IB. Type 1 diabetes mellitus and the use of flexible insulin regimens. Am Fam Physician. 1999;60(8):2343–52. 55-6
Efrat S. Beta-cell replacement for insulin-dependent diabetes mellitus. Adv Drug Deliv Rev. 2008;60(2):114–23.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Arfuso F, Jones F, et al. Advanced bile acid-based multi-compartmental microencapsulated pancreatic beta-cells integrating a polyelectrolyte-bile acid formulation, for diabetes treatment. Artif Cells Nanomed Biotechnol. 2014;1–8.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. An advanced microencapsulated system: a platform for optimized oral delivery of antidiabetic drug-bile acid formulations. Pharm Dev Technol. 2015;20(6):702–9.
Mooranian A, Negrulj R, Al-Salami H. Alginate-deoxycholic acid interaction and its impact on pancreatic Β-cells and insulin secretion and potential treatment of type 1 diabetes. J Pharm Innov. 2016;1-6
Mooranian A, Negrulj R, Jamieson E, Morahan G, Al-Salami H. Biological assessments of encapsulated pancreatic β-cells: their potential transplantation in diabetes. Cell Mol Bioeng. 2016;9:530–7.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Characterization of a novel bile acid-based delivery platform for microencapsulated pancreatic β-cells. Artif Cells Nanomed Biotechnol. 2014;1-7
Mooranian A, Negrulj R, Morahan G, Jamieson E, Al-Salami H. Designing anti-diabetic beta-cells microcapsules using polystyrenic sulfonate, polyallylamine and a tertiary bile acid: morphology, bioenergetics and cytokine analysis. Biotechnol Prog. 2016;32:501–9.
Mooranian A, Negrulj R, Al-Salami H. The effects of ionic gelation- vibrational jet flow technique in fabrication of microcapsules incorporating beta-cell: applications in type-1 diabetes. Curr Diabetes Rev 2015.
Mooranian A, Negrulj R, Al-Salami H. Flow vibration-doubled concentric system coupled with low ratio amine to produce bile acid-macrocapsules of beta-cells. Ther Deliv. 2016;7(3):171–8.
Mooranian A, Negrulj R, Al-Salami H. The impact of 1% allylamine on cell delivery microcapsules and insulin therapy in diabetes. J Microencapsul. 2016; (in press)
Mooranian A, Negrulj R, Al-Salami H. The incorporation of water-soluble gel matrix into bile acid-based microcapsules for the delivery of viable beta-cells of the pancreas, in diabetes treatment: biocompatibility and functionality studies. Drug Del Trans Res. 2016;6(1):17–23.
Mooranian A, Negrulj R, Al-Salami H. The influence of stabilized Deconjugated ursodeoxycholic acid on polymer-hydrogel system of transplantable NIT-1 cells. Pharm Res. 2016;33:1182–90.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Jones F, Arfuso F, et al. Novel multicompartmental bile acid-based microcapsules for pancreatic beta-cell transplantation. Xenotransplantation. 2015;22:S93–S4.
Mooranian A, Negrulj R, Chen-Tan N, Fakhouri M, Jones F, Arfuso F, et al. Novel multicompartmental bile acid-based microcapsules for pancreatic beta-cell transplantation. Transplantation. 2015;99(11):S151–S2.
Mooranian A, Negrulj R, Al-Salami H. Primary bile acid chenodeoxycholic acid-based microcapsules to examine β-cell survival and the inflammatory response. BioNanoSci. 2016;1-7
Mooranian A, Negrulj R, Al-Salami H. Viability and topographical analysis of microencapsulated β-cells exposed to a biotransformed tertiary bile acid: an ex vivo study. Intern J Nano Biomater 2016.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Jones F, Arfuso F, et al. Novel multicompartmental bile acid-based microcapsules for pancreatic beta-cell transplantation. Transplantation. 2015;99(11):S151–S2.
Mooranian A, Negrulj R, Al-Salami H. The incorporation of water-soluble gel matrix into bile acid-based microcapsules for the delivery of viable β-cells of the pancreas, in diabetes treatment: biocompatibility and functionality studies. Drug Deliv Transl Res. 2015;1-7
McKenzie MD, Jamieson E, Jansen ES, Scott CL, Huang DC, Bouillet P, et al. Glucose induces pancreatic islet cell apoptosis that requires the BH3-only proteins Bim and puma and multi-BH domain protein Bax. Diabetes. 2010;59(3):644–52.
Thomas HE, Darwiche R, Corbett JA, Kay TW. Evidence that β cell death in the nonobese diabetic mouse is Fas independent. J Immunol. 1999;163(3):1562–9.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Multicompartmental, multilayered probucol microcapsules for diabetes mellitus: formulation characterization and effects on production of insulin and inflammation in a pancreatic beta-cell line. Artif Cells Nanomed Biotechnol. 2015;1-12
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. The effect of a tertiary bile acid, taurocholic acid, on the morphology and physical characteristics of microencapsulated probucol: potential applications in diabetes: a characterization study. Drug Deliv Transl Res. 2015;1-12
Mooranian A, Negrulj R, Mikov M, Golocorbin-Kon S, Arfuso F, Al-Salami H. Novel chenodeoxycholic acid-sodium alginate matrix in the microencapsulation of the potential antidiabetic drug, probucol. An in vitro study. J Microencapsul. 2015;1-9
Negrulj R, Mooranian A, Chen-Tan N, Al-Sallami HS, Mikov M, Golocorbin-Kon S, et al. Swelling, mechanical strength, and release properties of probucol microcapsules with and without a bile acid, and their potential oral delivery in diabetes. Artif Cells Nanomed Biotechnol. 2015;1-8
Engin F, Yermalovich A, Nguyen T, Hummasti S, Fu W, Eizirik DL, et al. Restoration of the unfolded protein response in pancreatic beta cells protects mice against type 1 diabetes. Sci Transl Med. 2013;5(211):211ra–56.
Amaral JD, Viana RJ, Ramalho RM, Steer CJ, Rodrigues CM. Bile acids: regulation of apoptosis by ursodeoxycholic acid. J Lipid Res. 2009;50(9):1721–34.
Joo SS, Kang HC, Won TJ, Lee DI. Ursodeoxycholic acid inhibits pro-inflammatory repertoires, IL-1 beta and nitric oxide in rat microglia. Arch Pharm Res. 2003;26(12):1067–73.
Stojančević M, Pavlović N, Goločorbin-Kon S, Mikov M. Application of bile acids in drug formulation and delivery. Frontiers Life Sci. 2013;7(3–4):112–22.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mooranian, A., Tackechi, R., Jamieson, E. et al. Innovative Microcapsules for Pancreatic β-Cells Harvested from Mature Double-Transgenic Mice: Cell Imaging, Viability, Induced Glucose-Stimulated Insulin Measurements and Proinflammatory Cytokines Analysis. Pharm Res 34, 1217–1223 (2017). https://doi.org/10.1007/s11095-017-2138-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2138-y