Abstract
Background
The weight loss after bariatric surgery shows considerable individual variation. Twin studies of response to dietary interventions and studies of bariatric surgery patients suggest that genetic differences may play a role. This study aimed to examine the effect of three genetic risk scores on the inter-individual variation in excess body mass index loss (EBMIL) after Roux-en-Y gastric bypass. Furthermore, we searched among known adiposity-related single nucleotide polymorphisms (SNPs) for genetic determinants of the inter-individual variation in EBMIL.
Methods
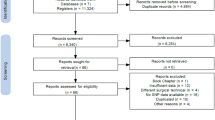
Patients with morbid obesity underwent Roux-en-Y gastric bypass and were genotyped (n = 577). Two genetic risk scores for weight loss after bariatric surgery and a genetic risk score for body mass index were calculated. Associations between the genetic risk scores and EBMIL were evaluated. Lasso regression was performed on 126 SNPs known to be associated with adiposity.
Results
The average EBMIL was 76.9% (range 21.7–149.2%). EBMIL was 81.1% (SD 20.6) and 73.9% (SD 21.7) in the high and low tertile groups of a genetic risk score for weight loss. Patients with a low genetic risk score for body mass index (in the lowest 5% percentile) had an EBMIL of 68.8% (SD 20.6, p = 0.018). Thirteen adiposity-related SNPs were identified to associate with EBMIL through lasso regression.
Discussion
A genetic risk score was associated with EBMIL after bariatric surgery, but may not yet be applicable to clinical practice. Patients genetically predisposed to low body mass index had lower weight loss after bariatric surgery.
Similar content being viewed by others
References
Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Hainer V, Stunkard AJ, Kunesova M, et al. Intrapair resemblance in very low calorie diet-induced weight loss in female obese identical twins. Int J Obes Relat Metab Disord. 2000;24(8):1051–7.
Hatoum IJ, Greenawalt DM, Cotsapas C, et al. Heritability of the weight loss response to gastric bypass surgery. J Clin Endocrinol Metab. 2011;96(10):E1630–3.
Bandstein M, Voisin S, Nilsson EK, et al. A genetic risk score is associated with weight loss following Roux-en Y gastric bypass surgery. Obes Surg. 2016;26(9):2183–9.
Rinella ES, Still C, Shao Y, et al. Genome-wide association of single-nucleotide polymorphisms with weight loss outcomes after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2013;98(6):E1131–6.
Bandstein M, Mwinyi J, Ernst B, et al. A genetic variant in proximity to the gene LYPLAL1 is associated with lower hunger feelings and increased weight loss following Roux-en-Y gastric bypass surgery. Scand J Gastroenterol. 2016;51(9):1050–5.
Hatoum IJ, Greenawalt DM, Cotsapas C, et al. Weight loss after gastric bypass is associated with a variant at 15q26.1. Am J Hum Genet. 2013;92(5):827–34.
de Toro-Martin J, Guenard F, Tchernof A, et al. Polygenic risk score for predicting weight loss after bariatric surgery. JCI Insight. 2018;3(17). https://doi.org/10.1172/jci.insight.122011.
Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206.
Shungin D, Winkler TW, Croteau-Chonka DC, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518(7538):187–96.
Kakela P, Jaaskelainen T, Torpstrom J, et al. Genetic risk score does not predict the outcome of obesity surgery. Obes Surg. 2014;24(1):128–33.
Speliotes EK, Willer CJ, Berndt SI, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42(11):937–48.
Heid IM, Jackson AU, Randall JC, et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet. 2010;42(11):949–60.
Loos RJ. The genetics of adiposity. Curr Opin Genet Dev. 2018;50:86–95.
Borisenko O, Colpan Z, Dillemans B, et al. Clinical indications, utilization, and funding of bariatric surgery in Europe. Obes Surg. 2015;25(8):1408.
Fenger M, Hansen DL, Worm D, et al. Gastric bypass surgery reveals independency of obesity and diabetes mellitus type 2. BMC Endocr Disord. 2016;16(1):59.
Willer CJ, Li Y, Abecasis GR. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26(17):2190–1.
McCarthy MI. Genomics, type 2 diabetes, and obesity. N Engl J Med. 2010;363(24):2339–50.
Grau K, Cauchi S, Holst C, et al. TCF7L2 rs7903146-macronutrient interaction in obese individuals’ responses to a 10-wk randomized hypoenergetic diet. Am J Clin Nutr. 2010;91(2):472–9.
Svendstrup M. Body fat distribution, metabolic health and weight changes - genetic and epidemiological studies in a prospective design: University of Copenhagen; 2017.
Livingstone KM, Celis-Morales C, Papandonatos GD, et al. FTO genotype and weight loss: systematic review and meta-analysis of 9563 individual participant data from eight randomised controlled trials. BMJ. 2016;354:i4707.
Osland E, Yunus RM, Khan S, et al. Weight loss outcomes in laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a meta-analysis and systematic review of randomized controlled trials. Surg Laparosc Endosc Percutan Tech. 2017;27(1):8–18.
Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 55 kb)
Rights and permissions
About this article
Cite this article
Aasbrenn, M., Schnurr, T.M., Have, C.T. et al. Genetic Determinants of Weight Loss After Bariatric Surgery. OBES SURG 29, 2554–2561 (2019). https://doi.org/10.1007/s11695-019-03878-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03878-5