Abstract
Background
Failure occurs in up to 60% of the patients that were treated with primary restrictive bariatric operations such as Laparoscopic Adjustable Gastric Banding (LAGB), or restrictive/metabolic operations like Laparoscopic Sleeve Gastrectomy (LSG). Insufficient weight loss and weight regain are the most commonly reported reasons of failure. The aim of this retrospective multicenter study was to compare One Anastomosis Gastric Bypass (OAGB) to Roux-en-Y Gastric Bypass (RYGB) as a revisional procedure in terms of weight loss, procedure time, complication rate and morbidity.
Methods
491 patients operated on between 2012 and 2017 for failed restrictive surgery were included in this study (OAGB (n=185) or RYGB (n=306)). Failure was defined as total weight loss (TWL) less than 25%, excess weight loss (EWL) less than 50% and/or a remaining body mass index (BMI) larger than 40 kg/m2 at two years of follow up. Primary outcome measures were %TWL and % excess BMI loss (EBMIL) at 12, 24 and 36 months of follow-up. Secondary outcomes were procedure time, reduction of comorbidity, early and late complication rate, and mortality.
Results
%TWL was significantly larger in the OAGB group at 12 months (mean 24.1±9.8 vs. 21.9±9.7, p = 0.023) and 24 months (mean 23.9±11.7 vs. 20.5±11.2, p = 0.023) of follow-up. %EBMIL was significantly larger in the OAGB group at 12 months (mean 69.0±44.6 vs. 60.0±30.1, p = 0.014) and 24 months (mean 68.6±51.6 vs. 56.4±35.4, p = 0.025) of follow-up. Intra-abdominal complications (leakage, bleeding, intra-abdominal abscess and perforation) occurred less frequently after revisional OAGB (1.1% vs. 4.9%, p = 0.025). Surgical intervention for biliary reflux (5.4% vs. 0.3%, p < 0.001) was more prevalent in the OAGB group. Surgical intervention for internal herniation (0.0% vs. 4.9%, p = 0.002) was more prevalent in the RYGB group.
Conclusions
This study suggests that OAGB is superior to RYGB as a remedy for insufficient weight loss and weight regain after failed restrictive surgery with more weight loss and a lower early complication rate. To substantiate these findings, further research from prospective randomized controlled trials is needed.
Similar content being viewed by others
Introduction
Obesity is a global health problem of increasing proportions and is a major risk factor for premature death and morbidity such as type 2 diabetes mellitus (T2DM), obstructive sleep apnea syndrome (OSAS), hypertension, dyslipidemia and osteoarthritis [1].
Bariatric surgery is the most effective treatment in morbidly obese patients, in terms of weight loss and reduction of these comorbidities [2, 3].
Primary restrictive procedures such as Vertical Banded Gastroplasty (VBG), Laparoscopic Adjustable Gastric Banding (LAGB) or Laparoscopic Sleeve Gastrectomy (LSG), although the latter is considered to be a metabolic procedure, seem to be a safe and effective strategy for weight reduction in short and mid-term follow-up. However, patients who underwent these procedures are at risk of having insufficient weight loss and weight regain [4,5,6,7,8]. These complications can be an indication for revisional surgery [8, 9]. Cumulative failure rates in patients who received LSG and LAGB have been reported up to 30 and 60%, respectively [10,11,12,13,14,15,16,17]. However, revisional procedures appear to be only moderately effective in terms of additional weight loss. On average, revisional surgery has a higher complication rate and longer length of stay compared to primary bariatric interventions [18, 19].
Roux-en-Y gastric bypass (RYGB) is currently the golden standard as a revisional procedure. However, various success rates of RYGB as a remedy of failure of restrictive surgery are reported [20,21,22,23,24,25,26,27,28,29,30,31,32,33]. In current literature weight loss results of revisional RYGB is usually inferior compared to primary RYGB, with an reported additional percentage excess body mass index loss (EBMIL) at 6, 12 and 48 months of 22.5%, 29.1% and 37.5%, respectively [20, 31]. Early complications such as leakage, bleeding and infection occur in 11.8-16.6% of the cases and surgical intervention due to these complications is performed in 4.5-8% [20,21,22,23]. A long-term complication of (revisional) RYGB, which often requires surgical intervention, is internal herniation and occurs in 3.3-4.9%. [20, 25, 29].
The benefits of RYGB as a revisional procedure might outweigh the risk for the majority of the patients, but the overall complication rate remains relatively high. Due to technical difficulties of revisional surgery a learning curve is present, but most recent literature still reports an early allcause complication rate of 4.5-11.4% [31,32,33]. In previous studies on revisional RYGB, series are often small, and groups are heterogeneous, with both weight-related problems and complications of primary surgery-related being an indication for revision.
Therefore, caution is needed to draw firm conclusions about the benefits of revisional RYGB and a more targeted approach in finding a remedy for patients after failed restrictive surgery is paramount.
One Anastomosis Gastric Bypass (OAGB), as first reported by Rutledge [34], has been described as a viable alternative, due to its relative technical simplicity, reversibility and shorter operation time.
Primary OAGB is effective in weight loss and remission of T2DM and superior to RYGB in this respect, while being associated with a shorter operating time and slightly less post-operative complications [35]. As a primary procedure when compared to RYGB, percentage excess weight loss (EWL) five years post-surgery of OAGB has been reported as 72.9% vs. 60.1% with a complication rate of 3.2% vs. 1.8% [36,37,38,39,40,41]. The prevalence of gastric ulcers between OAGB and RYGB is similar [42,43,44]. A long-term concern after OAGB is symptomatic biliary reflux gastritis, which requires revisional surgery. More recent trials report a biliary reflux rate of 0.4-0.9% and clear implication of this in clinical practice still needs to be established.
Several studies showed the efficacy of OAGB as a revisional procedure as well, in terms of weight loss and reduction of comorbidity [44,45,46,47,48,49]. After failed restrictive operations, EBMIL of up to 66% is reported at five years follow up [45]. However, cohorts are small and no comparative research between OAGB and RGYB as a revisional procedure has been conducted up to this point.
The aim of the current study was to compare OAGB to RYGB as a revisional procedure after failed restrictive surgery in terms of weight loss, procedure time, complication rate, reduction of comorbidity, complication rate and mortality.
Methods
Study Objective and Design
The primary aim of this retrospective multicenter study was to compare effectiveness of OAGB and RYGB as a remedy for insufficient weight loss and weight regain after failed primary restrictive procedures in terms of additional weight loss. Secondary objectives were to evaluate procedure time, reduction of comorbidity, short- and long term complication rate, and mortality between the two procedures.
Patient selection and data collection
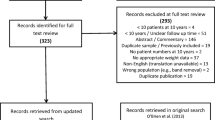
For this study, selected patients were retrospectively analyzed. Data were collected from hospital medical records. Adult patients who presented with insufficient weight loss and/or weight regain after failed LSG or LAGB after two years and who underwent revisional OAGB or RYGB at one of three Dutch high volume bariatric hospitals from 2012 to 2017, were included in this study. Patients who received revisional surgery for other indications such as comorbidity or complications of primary surgery were excluded from this study. In accordance with IFSO guidelines, all patients were between 18 and 65 years of age when the primary procedure was performed.
Preoperative assessments of patient eligibility for bariatric surgery included consultation with an endocrinologist, a dietician, and a psychologist to exclude patients with non-adjusted eating patterns or eating disorders. If detected, these issues were addressed and fully treated before surgery was considered. Insufficient weight loss or weight regain was defined as EWL <50% and/or TWL <25% and/or BMI >40 kg/m2 at 2 years follow-up. The medical-ethical committees of all participating hospitals approved this study prior to data collection. Exclusion criteria were known psychiatric illness or eating disorder, pregnancy, previous gastric surgery other than primary bariatric procedure.
Surgical Technique and Perioperative Management
One Anastomosis Gastric Bypass
A standardized operation protocol was used in all patients as reported previously [46, 55]. In case the previous procedure consisted of LAGB, the band was removed as well as dissection of the angle of His. The capsule of the band on the stomach was occasionally divided or removed. The linear stapler divides the stomach horizontally at the junction of the corpus and antrum at the level of crow’s foot. In case of a previous gastric sleeve, mostly only horizontal transection was used. Limb length varied from 150 to 250 cm based on the patient’s preoperative BMI. This tailored approach, which was modified from Lee’s recommendations [41, 43], involved a BP limb of 150 cm for patients with BMI 40 and 50.
Roux-en-Y Gastric Bypass
A standardized operation protocol was used in all patients. The technique of this procedure is also described by Emous. [55] In case the previous procedure consisted of LGB, the band was removed as well as adhesiolysis of the angle of His. The capsule of the band on the stomach was occasionally divided or removed. After this the bypass was performed. The mesenteric defects were not routinely closed in all centers.
Postoperative Care
All bariatric patients enrolled in an enhanced recovery program and received 3-12 months of postoperative PPI therapy to prevent marginal ulcers. Patients were advised to quit smoking prior to undergoing OAGB or RYGB. Postoperative daily multivitamin supplements were prescribed. Patients were put on a fluid diet for 2-3 weeks beginning on the first postoperative day. Most patients were discharged from the hospital 1–2 days after surgery. Patients received postoperative counseling by the surgeon or specialized bariatric nurse at 4-8 weeks after surgery, at 12 months after surgery, and yearly thereafter until five years after last surgery. After surgery, all patients were scheduled for a 1.5-year, sequential (monthly) group meeting program that included counseling by a bariatric nurse practitioner, a dietician, a psychologist, and a physiotherapist.
Outcome Measures
Baseline characteristics before revisional surgery were determined and entered into the database. Each patient’s ideal weight was estimated based on a target BMI of 25. The primary outcome was percentage total weight loss (%TWL) and percentage excess body mass index loss (%EBMIL) at 12, 24, and 36 months of follow-up, measuring the difference between weightrelated parameters before and after performing the revisional procedure. These measurements were performed by doctors or specialized bariatric nurses in one of the participating hospitals. %TWL, %EBMIL, and improvement of comorbidities was defined according to Brethauer et. al. [50]. Secondary outcomes were mortality, complications following revisional surgery (Clavien Dindo grade 3 or higher), operation time and reduction of comorbidity. Complications were divided into short-term (< 30 days) including anastomotic leak, bleeding, infection, perforation, myocardial infarction and stroke and long-term (> 30 days) including nutritional deficiencies, gastric ulceration, stricture and bile reflux, internal herniation and malnutrition. Comorbidities that were investigated included T2DM, CVD, OSAS, dyslipidemia and osteoarthritis.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 22. Normality of continuous data was tested with the Shapiro-Wilk test. Descriptive statistics were performed to report patient characteristics. For continuous data mean ± SE was calculated or median and percentiles for variables that were not normally distributed. For categorical data frequencies were calculated.
Differences between groups in continuous data will be tested by a two-sided Student’s t test or a Mann-Whitney U test for variables that were not normally distributed. Subgroup analysis will be conducted where applicable. A p-value <0.05 was taken as the threshold of statistical significance.
Results
Pre-operative Patient Characteristics
Between January 2012 and September 2017, 495 patients underwent either OAGB (n = 189) or RYGB (n = 310) as revisional surgery after a failed restrictive procedure. Demographics before revisional surgery are shown in Table 1. Patients receiving OAGB were younger (mean age 46 ± 9.0 vs. 48 ± 9.6, p = 0.018) and less often female (75.5% vs. 84.3%, p = 0.017). Sleeve gastrectomy was more often performed as primary procedure (35.1% vs. 24.5%, p = 0.012) in the OAGB group, and adjustable gastric banding was more often performed (64.9% vs. 75.5%, p = 0.012) in the RYGB group. Furthermore, there were no significant differences between groups. In cases where comorbidity was reported, dyslipidemia (19.0% vs. 27.7%, p = 0.033) was more frequent in the RYGB group. No differences in frequency of other comorbidities (T2DM, CVD, OSAS, osteoarthritis, and GERD) were found (Table 1).
Perioperative Details and Early Complications
Procedure time was significantly shorter in the OAGB group (median time 72 [56–95] minutes vs. 83 [66–103] minutes, p < 0.001). Compared with RYGB, length of biliary limb was 80 cm longer on average in the OAGB group (median length 180 [175–180] vs. 100 [80–150], p < 0.001). Early complication rate (< 30 days post-redo) is listed in Table 2. Significantly less intra-abdominal complications (leakage, bleeding, intra-abdominal abscess, and perforation) were present after revisional OAGB compared with RYGB (1.1% vs. 4.9%, p = 0.025). No significant difference in other early complications was present between groups. Two patients died in the follow-up period, one in the OAGB group (0.5%) and one in the RYGB group (0.3%), and this difference was not statistically significant. One patient committed suicide and one patient died due to abdominal sepsis after an incarcerated umbilical hernia, both not attributable to bariatric surgery.
Weight Loss
Annual BMI and weight loss parameters after revisional surgery are shown in Table 3. No significant difference in BMI was found 12 months post-redo, but BMI was significantly lower in the OAGB group at 24 months (mean 30.8 ± 5.2 vs. 32.6 ± 5.9, p = 0.016) and 36 months (mean 31.1 ± 5.1 vs. 34.3 ± 7.1, p = 0.012). %TWL was significantly larger in the OAGB group at 12 months (mean 24.1 ± 9.8 vs. 21.9 ± 9.7, p = 0.023) and 24 months (mean 23.9 ± 11.7 vs. 20.5 ± 11.2, p = 0.023) of follow-up.
%EBMIL was significantly larger in the OAGB group at 12 months (mean 69.0 ± 44.6 vs. 60.0 ± 30.1, p = 0.014) and 24 months (mean 68.6 ± 51.6 vs. 56.4 ± 35.4, p = 0.025) of follow-up. %TWL (22.5 ± 15.2 vs.17.4 ± 13.3, p = 0.056) and EBMIL% (mean 58.3 ± 36.0 vs. 46.5 ± 35.0, p = 0.084) were higher in the OAGB group at 36 months of follow-up as well, but these differences were not statistically significant.
Late Complications, Morbidity, and Surgical Intervention
Late complications (> 30 days post-redo) are listed in Table 4. No significant difference in the cumulative rate of surgical intervention for any cause due to long-term (> 30 days) complications was found between groups (OAGB vs. RYGB: 9.2% vs. 12.4%, p = 0.227). Two patients needed treatment in the intensive care, both in the RYGB group. Surgical intervention due to biliary reflux (5.4% vs. 0.3%, p < 0.001) was more prevalent in the OAGB group. Surgical intervention due to internal herniation (0.0% vs. 4.9%, p = 0.002) was more prevalent in the RYGB group. No significant difference between the rate of cholecystectomy, iron deficiency, hypoglycemia, hypoalbuminemia, gastric ulcer, or stricture formation of the anastomosis was found between groups. No significant differences in reduction of comorbidities (T2DM, CVD, OSAS, dyslipidemia, osteoarthritis, and GERD) were found (Table 5).
Discussion
In this large multi-center study, OAGB seems more successful in terms of weight loss in the short and mid-term (two years of follow-up) when compared to RYGB. OAGB has a shorter procedure time and a lower complication rate up to thirty days after surgery. No difference is seen in surgical re-interventions and reduction of comorbidity after up to three years of follow up between OAGB and RYGB.
To our knowledge, this is the first large study that compares and describes OAGB versus RYGB as revisional procedure in a large multicenter cohort.
Several studies already showed the effectiveness of OAGB as a primary procedure with noninferior weight loss and a lower complication rate when compared to primary RYGB [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. This study further substantiated the findings of previous publications, through a comparative design and a high-volume multicenter cohort investigating the effectiveness and safety of RYGB and OAGB as a revisional procedure. Thus providing limited evidence that OAGB is more effective for additional weight-loss and could be a safer alternative to RYGB after failed primary restrictive bariatric surgery.
Symptomatic bile reflux, requiring revisional surgery, has been reported as a complication of OAGB [42,43,44]. Surgical intervention due to bile reflux after redo-OAGB was found in this study as well. The bile reflux rates are relative high compared to those reported in literature, suggesting a possible learning curve is still involved. However, all bariatric surgeons in this study were experienced with OAGB [46] and have passed their learning curve. Another probable reason for this higher rate was a low threshold to convert one anastomosis gastric bypass to RYGB in case of suspicion of bile reflux. It could also be possible that bile reflux incidence is underreported in other studies. The diagnostic workup of bile reflux was not standardized in this trial and could be based on history taking alone. In cases where endoscopy was performed, no difference was found in this study in gastric ulcer formation after OAGB compared to RYGB, as has been described by previous studies before [42,43,44]. The more recent YOMEGA trial reported more reflux in the gastric pouch in revisional OAGB vs RYGB, without difference in quality of life. [35] A more recent trial failed to detect this difference altogether. [51]
Another concern, which was also found in the YOMEGA trial, are nutritional adverse events after OAGB [35]. In our study we found more malnutrition in the OAGB group as well, but no difference in hypoalbuminemia and no deficiencies that lead to re-intervention. The YOMEGA trial did not report on this and had a non-inferiority design.
Also, BP limb length was on average 200cm in the YOMEGA trial and 180cm in our study which also could explain difference found in the frequency of nutritional adverse events. Theoretically a longer BP limb length, as is common in OAGB when compared to RYGB, could explain the larger weight loss found in OAGB as well as the possibility of more nutritional adverse events. Another recent study, which also had a mean BP length of 200cm, did not find significant differences in nutritional status after revisional OAGB vs revisional RYGB, but did find a better resolution of metabolic syndrome after OAGB. [51] Hence this subject still remains a matter of debate.
High surgical revision rate after revisional RYGB (for internal herniation and abdominal pain) was observed in our study. Preventive closure of mesenteric defects with staples was not routinely performed but gradually became more common practice in the period this trial was conducted and this might have influenced results. The intervention rates due to internal herniation might have been lower if mesenteric defects were closed during all the revisional procedures, as is currently common practice in the participating centers. From earlier research it is known that the percentage of internal herniation could be reduced by halve in case of closure during gastric bypass surgery. Theoretically, if the same would have happened in our study the surgical intervention rate after both procedures could have been comparable. However more recent studies report an incidence of internal herniation of 3.4-4.2% after revisional laparoscopic RYGB, for which intervention was needed, which is still higher than the incidence we found after revisional OAGB. [52, 53]
Thus, we conclude that OAGB as a revisional procedure is at least as safe as RYGB concerning the development of late complications for which intervention is needed. No differences in reduction in comorbidity after up to three years of follow up between OAGB and RYGB. These findings are in line with results from other high-volume comparative trials. [54, 55]
One of the limitations of this study is relative heterogeneity of cohorts due to the retrospective nature of the data collection. Patients were younger and more often male in the OAGB group. Therefore, both selection and reporting bias might have been present and randomized controlled trials are indicated to extrapolate the results of this study to the general population. Another heterogeneity is the difference in primary restrictive procedure that was performed. Sleeve gastrectomy was more prevalent in the OAGB group, gastric banding was more prevalent in the RYGB group. However, this difference didn’t reflect in a difference in BMI, percentage of weight regain or percentage of insufficient weight loss between groups. Thus groups were comparable regarding weight-related parameters at baseline.
Therefore, we conclude that this heterogeneity in the performed primary procedure did not influence the positive results regarding the efficacy of OAGB in terms of weight loss. Our analysis shows superior weight loss in the OAGB group at 12 and 24 months of follow up compared to the RYGB group. Technical differences between revisional surgery after sleeve gastrectomy vs. gastric banding could have biased the lower early complication rate we found after OAGB compared to RYGB.
Another limitation is loss to follow up in medical records of long-term weight loss parameters and comorbidities. This is a well-known phenomenon after bariatric surgery and the reason of this is not completely understood. [56]
In conclusion, the assumption is made that the abovementioned differences between groups did not significantly influence the primary outcome of this trial that OAGB is more effective as a remedy for insufficient weight loss and weight regain after restrictive surgery.
However, more evidence from prospective studies with standardized diagnostic workup of comorbidities and perioperative protocols and randomized groups is needed to substantiate our findings.
Change history
08 May 2020
In the original article there was a discrepancy between the XML (online) version of the article and the PDF.
References
Maggard MA, Shugarman LR, Suttorp M, et al. Clinical Guidelines Meta-Analysis: Surgical Treatment of Obesity. 2005.
El-Hadi M, Birch DW, Gill RS, et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg. 2014;57(2):139–44.
O’Brien PE, Macdonald L, Anderson M, et al. Long-Term Outcomes After Bariatric Surgery. Ann Surg. 2013;257(1):87–94.
Franco JVA, Ruiz PA, Palermo M, et al. A review of studies comparing three laparoscopic procedures in bariatric surgery: Sleeve gastrectomy, roux-en-y gastric bypass and adjustable gastric banding. Obes Surg. 2011;21:1458–68.
Catheline J-M, Fysekidis M, Bachner I, et al. Five-year results of sleeve gastrectomy. J Visc Surg Elsevier Masson SAS. 2013;150(5):307–12.
Van Rutte PWJ, Smulders JF, De Zoete JP, et al. Outcome of sleeve gastrectomy as a primary bariatric procedure. Br J Surg. 2014;101(6):661–8.
Trastulli S, Desiderio J, Guarino S, et al. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. Elsevier. 2013;9(5):816–29.
Seki Y, Kasama K, Hashimoto K. Long-Term Outcome of Laparoscopic Sleeve Gastrectomy in Morbidly Obese Japanese Patients. Obes Surg. 2015.
Elnahas A, Graybiel K, Farrokhyar F, et al. Revisional surgery after failed laparoscopic adjustable gastric banding: A systematic review. Surg Endosc Other Interv Tech. 2013;27(3):740–5.
Gonzalez-Heredia R, Masrur M, Patton K, et al. Revisions after failed gastric band: sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Endosc Springer US. 2014:2533–7.
Smukalla S, Pitman M, Khan A, et al. Sleeve Gastrectomy is a Risk Factor for Barrett's Esophagus: A Systematic Review and Meta-Analysis. Gastroenterology. 2017;152(5, Supplement 1):S457–8.
Van Nieuwenhove Y, Ceelen W, Stockman A, et al. Long-term results of a prospective study on laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011;21(5):582–7.
Marsk R, Jonas E, Gartzios H, et al. High revision rates after lapa- roscopic vertical banded gastroplasty. Surg Obes Relat Dis. 2009;5(1):94–8.
De Maria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg. 2001;223:809–18.
Rabkin R. Distal Gastric Bypass/Duodenal Switch Procedure, Roux-en-Y Gastric Bypass and Biliopancreatic Diversion in a Community Practice. Obes Surg. 1998;8(1):53–60.
Madura JA, DiBaise JK. Quick fix or long-term cure? Pros and cons of bariatric surgery. F1000 Med Rep. 2012;4:19.
Bennett JMH, Mehta S, Rhodes M. Surgery for morbid obesity. Postgrad Med J. 2007;83(975):8–15.
Mann JP, Jakes AD, Hayden JD, et al. Systematic Review of Definitions of Failure in Revisional Bariatric Surgery. Obes Surg. 2015;25(3):571–4.
Kellogg TA. Revisional bariatric surgery. Surg Clin North Am Elsevier Inc. 2011;91(6):1353–71. x
Sanchez H, Cabrera A, Cabrera K, et al. Laparoscopic Roux-en-Y Gastric Bypass as a Revision Procedure after Restrictive Bariatric Surgery. 2008;1539–43.
Suter M, Ralea S, Millo P, et al. Laparoscopic Roux-en-Y Gastric Bypass After Failed Vertical Banded Gastroplasty: a Multicenter Experience with 203 Patients. 2012. 1554–61.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery. American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis Elsevier. 2014;10(5):1–21.
Apers JA, Wens C, Vlodrop V Van, et al. Perioperative outcomes of revisional laparoscopic gastric bypass after failed adjustable gastric banding and after vertical banded gastroplasty : experience with 107 cases and subgroup analysis. 2013;558–64.
Bands G. Revision to Malabsorptive Roux-En-Y Gastric Bypass ( MRNYGBP ) Provides Long-Term (10 Years ) Durable Weight Loss in Patients with Failed Anatomically Intact Gastric Restrictive Operations. 2011. 825–31.
Coakley BA, Deveney CW, Spight DH, et al. Revisional bariatric surgery for failed restrictive procedures. 2008;4:581–6.
Dessel E Van, Hubens ÆG, Ruppert ÆM, et al. Roux-en-Y gastric bypass as a re-do procedure for failed restricive gastric surgery. 2008;1014–8.
Aarts E, Koehestanie P, Dogan K, et al. Revisional surgery after failed gastric banding : results of one-stage conversion to RYGB in 195 patients. Surg Obes Relat Dis Elsevier. 2014;10(6):1077–83.
Edholm D, Näslund I, Karlsson FA, et al. Twelve-year results for revisional gastric bypass after failed restrictive surgery in 131 patients. Surg Obes Relat Dis [Internet] Elsevier. 2014;10(1):44–8.
Hedberg J, Gustavsson S, Sundbom M. Long-term follow-up in patients undergoing open gastric bypass as a revisional operation for previous failed restrictive procedures. SOARD. Elsevier Inc. 2012;8(6):696–701.
Gagné DJ, Dovec E, Urbandt JE. Laparoscopic revision of vertical banded gastroplasty to Roux-en- Y gastric bypass : outcomes of 105 patients. SOARD Elsevier Inc. 2011;7(4):493–9.
Almalki OM, Lee WJ, Chen JC, et al. Revisional Gastric Bypass for Failed Restrictive Procedures: Comparison of Single-Anastomosis (Mini-) and Roux-en-Y Gastric Bypass. Obes Surg. 2018;28(4):970–5.
Yorke E, Sheppard C, Switzer NJ, et al. Revision of sleeve gastrectomy to Roux-en-Y Gastric Bypass: A Canadian experience. Am J Surg. 2017;213(5):970–4.
Sadot E, Spivak H. Weight Loss After Laparoscopic Band-to-Bypass Revision Compared With Primary Gastric Bypass. Surg Laparos Endos Percu Tech. 2015;25(3):258–261.31.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80.
Robert M, Espalieu P, Pelascini E, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393(10178):1299–309.
Lee W-J, Lee Y-C, Ser K-H, et al. Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis. 2011;7(4):486–91.
Musella M, Apers J, Rheinwalt K, et al. Efficacy of Bariatric Surgery in Type 2 Diabetes Mellitus Remission: the Role of Mini Gastric Bypass/One Anastomosis Gastric Bypass and Sleeve Gastrectomy at 1 Year of Follow-up. A European survey. Obes Surg. 2015.
Lee W-J, Chong K, Lin Y-H, et al. Laparoscopic Sleeve Gastrectomy Versus Single Anastomosis (Mini-) Gastric Bypass for the Treatment of Type 2 Diabetes Mellitus: 5-Year Results of a Randomized Trial and Study of Incretin Effect. Obes Surg. 2014:1552–62.
Quan Y, Huang A, Ye M, et al. Efficacy of Laparoscopic Mini Gastric Bypass for Obesity and Type 2 Diabetes Mellitus : A Systematic Review and Meta-Analysis. Gastro Res Pract. 2015; 2015.
Guenzi M, Arman G, Rau C, et al. Remission of type 2 diabetes after omega loop gastric bypass for morbid obesity. Surg Endosc. 2015:2669–74.
Lee W-J, Yu P-J, Wang W, et al. Laparoscopic Roux-en-Y Versus Mini-Gastric Bypass for the Treatment of Morbid Obesity. Ann Surg. 2005;242(1):20–8.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28(1):156–63.
Lee W-J, Lin Y-H. Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes Surg. 2014;24(10):1749–56.
Moszkowicz D, Rau C, Guenzi M, et al. Laparoscopic omega-loop gastric bypass for the conversion of failed sleeve gastrectomy: early experience. J Visc Surg Elsevier Masson SAS. 2013;150(6):373–8.
Bruzzi M, Voron T, Zinzindohoue F, et al. Revisional singleanastomosis gastric bypass for a failed restrictive procedure: 5-year results. Surg Obes Relat Dis. 2016;12(2):240–5.
Apers J, Wijkmans R, Totte E, et al. Implementation of mini gastric bypass in the Netherlands: early and midterm results from a high-volume unit. Surg Endosc. 2018;32(9):3949–55. https://doi.org/10.1007/s00464-018-6136-x.
Lönroth H. Laparoscopic gastric bypass. Obes Surg. 1998;8(6):563–5.
Lee WJ, Yu PJ, Wang W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;242:20–8.
Lee WJ, Wang W, Lee YC, et al. Laparoscopic minigastric bypass: experience with tailored bypass limb according to body weight. Obes Surg. 2008;18:294–9.
Brethauer S, Kim J, Chaar M, et al. Standardized Outcomes Reporting in Metabolic and Bariatric Surgery. Obes Surg. 2015;25:587–606.
Lee WJ, Almalki OM, Ser KH, et al. Obes Surg. 2019;29:3047. https://doi.org/10.1007/s11695-019-04065-2.
Dakour Aridi HN, Wehbe M, Shamseddine G, et al. Long-Term Outcomes of Rouxen-Y Gastric Bypass Conversion of Failed Laparoscopic Gastric Band. Obes Surg. 2017;27:1401–8. https://doi.org/10.1007/s11695-016-2529-x.
Al-Kurd A, Grinbaum R, Abubeih A, et al. Conversion of Laparoscopic Adjustable Gastric Banding to Gastric Bypass: a Comparison to Primary Gastric Bypass. Obes Surg. 2018;28:1519–25. https://doi.org/10.1007/s11695-017-3047-1.
Navarrete S, Leyba JL, Borjas G, et al. Results of The Comparative Study of 200 Cases: One Anastomosis Gastric Bypass vs Roux-en-Y Gastric Bypass. Obes Surg. 2018;28:2597.
Emous M, Apers J, Hoff C, et al. Conversion of failed laparoscopic adjustable gastric banding to Roux-en-Y gastric bypass is safe as a single-step procedure. Surg Endosc. 2015;29:2217–23.
Haper J, Madan AK, Ternovits CA, et al. What happens to patients who do not follow-up after bariatric surgery? Am Surg. 2007;73(2):181–4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised to restore text and tables that were inadvertently omitted from the online PDF.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Poublon, N., Chidi, I., Bethlehem, M. et al. One anastomosis gastric bypass vs. Roux-en-Y gastric bypass, remedy for insufficient weight loss and weight regain after failed restrictive bariatric surgery. OBES SURG 30, 3287–3294 (2020). https://doi.org/10.1007/s11695-020-04536-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04536-x