Abstract
Introduction
Obesity is a chronic disease associated with other comorbidities, including atherogenic dyslipidemia (AD). Bariatric surgery (BS) has shown to reduce cardiovascular risk (CVR) by achieving a significant weight reduction and improving the lipid profile. Different surgical techniques may have a different effect on the lipoprotein profile.
Purpose
To evaluate the lipid profile at 3 years after BS according to the surgical technique used and to determine which variables predict variation in the lipid profile at 3 years after BS.
Methods
Retrospective observational study of 206 patients who underwent BS between 2010 and 2019. We analyzed the variation of lipid parameters in the 3 years of follow-up according to the surgical technique, including a group analysis of patients according to whether they had dyslipidemia and whether they were treated or untreated and determined which variables predict variation in the lipid profile at 3 years after BS.
Results
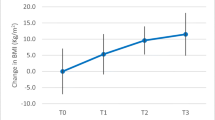
There was a significant increase in high-density lipoprotein cholesterol (HDL-c) with sleeve gastrectomy (SG) and a significant decrease in total cholesterol (TC), LDL-cholesterol (LDL-c), non-HDL, and LDL/non-HDL with biliopancreatic diversion (BPD). Variables predicting lipid profile variation were surgical technique and pre-surgery lipoprotein level.
Conclusions
Malabsorptive techniques achieve a greater decrease in TC and LDL-c throughout follow-up and could also improve residual cardiovascular risk (non-HDL and LDL/non-HDL). The type of surgical technique and the presurgery lipid profile predict variation after 3 years of BS.
Graphical abstract




Similar content being viewed by others
References
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019 May;15(5):288–98. https://doi.org/10.1038/s41574-019-0176-8.
Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22(7 Suppl):s176–85.
Langlois et al. Quantifying atherogenic lipoproteins: current and future challenges in the era of personalized medicine and very low concentrations of LDL cholesterol. A consensus statement from EAS and EFLM. Clinical Chemistry. 2018;64(7):1006–33. https://doi.org/10.1373/clinchem.2018.287037.
Sjöström L, Lindroos AK, Peltonen M, et al. Swedish Obese Subjects Study Scientific Group. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93. https://doi.org/10.1056/NEJMoa035622.
Heffron SP, Parikh A, Volodarskiy A, et al. Changes in lipid profile of obese patients following contemporary bariatric surgery: a meta-analysis. American Journal of Medicine. 2016;129(9):952–9. https://doi.org/10.1016/j.amjmed.2016.02.004.
Climent E, Benaiges D, Flores-Le Roux JA, et al. Changes in the lipid profile 5 years after bariatric surgery: laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy. Surgery for Obesity and Related Diseases. 2018;14(8):1099–105. https://doi.org/10.1016/j.soard.2018.05.006.
Boza C, Gamboa C, Salinas J, et al. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis. 2012;8:243–9. https://doi.org/10.1016/j.soard.2011.08.023.
Ðanić M, Stanimirov B, Pavlović N, et al. Pharmacological applications of bile acids and their derivatives in the treatment of metabolic syndrome. Frontiers in Pharmacology. 2018;9(December):1–20. https://doi.org/10.3389/fphar.2018.01382.
Hernández-Mijares A, et al. Riesgo cardiovascular residual de origen lipídico. Componentes y aspectos fisiopatológicos. Clin Investig Arterioscler. 2018. https://doi.org/10.1016/j.arteri.2018.06.007
Almenta, Ester, Ruiz-Tovar, Jaime, Santos, Raquel & Garcia-moreno, Francisca. Vía clínica en cirugía Bariátrica. 2017.
Zhu B, Zhang N. Evaluation of insulin resistance improvement after laparoscopic sleeve gastrectomy or gastric bypass surgery with HOMA-IR. BioScience Trends. 2017;11(6):675–81. https://doi.org/10.5582/bst.2017.01307.
Alejo Ramos M, Ballesteros Pomar MD, Urioste Fondo AM, et al. Cano Rodríguez IM. Bone metabolism and fracture risk after biliopancreatic diversion. Endocrinol Diabetes Nutr. 2021;68(3):144–52. English, Spanish. https://doi.org/10.1016/j.endinu.2020.08.005.
Sabench Pereferrer F, Domínguez-Adame Lanuza E, Ibarzabal A, et al. Quality criteria in bariatric surgery: consensus review and recommendations of the Spanish Association of Surgeons and the Spanish Society of Bariatric Surgery. Cir Esp. 2017;95(1):4–16.
Geltner C, Lechleitner M, Föger B, et al. Insulin improves fasting and postprandial lipemia in type 2 diabetes. Eur J Intern Med. 2002 Jun;13(4):256–63. https://doi.org/10.1016/s0953-6205(02)00038-9.
Millán Núñez-Cortés J, Pedro-Botet Montoya J, Pintó Sala X. Dislipidemia aterogénica y riesgo residual. Estado de la cuestión en 2014. Clínica e Investigación En Arteriosclerosis. 2014;26(6):287–92. https://doi.org/10.1016/j.arteri.2014.09.004.
Segal JB, Clark JM, Shore AD, et al. Prompt reduction in use of medications for comorbid conditions after bariatric surgery. Obes Surg. 2009;19:1646–56. https://doi.org/10.1007/s11695-009-9960-1.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. https://doi.org/10.1001/jama.292.14.1724.
Park JY. Prediction of type 2 diabetes remission after bariatric or metabolic surgery. J Obes Metab Syndr. 2018;27(4):213–22. https://doi.org/10.7570/jomes.2018.27.4.213.
Benetti A, Del Puppo M, Crosignani A, et al. Cholesterol metabolism after bariatric surgery in grade 3 obesity: differences between malabsorptive and restrictive procedures. Diabetes Care. 2013;36(6):1443–7. https://doi.org/10.2337/dc12-1737.
Lubrano C, Mariani S, Badiali M, et al. Metabolic or bariatric surgery Long-term effects of malabsorptive vs restrictive bariatric techniques on body composition and cardiometabolic risk factors. International Journal of Obesity. 2010;34(9):1404–14. https://doi.org/10.1038/ijo.2010.54.
Benaiges D, Flores-Le-Roux JA, Pedro-Botet J, et al. Goday A; Obemar Group. Impact of restrictive (sleeve gastrectomy) vs hybrid bariatric surgery (Roux-en-Y gastric bypass) on lipid profile. Obes Surg. 2012;22(8):1268–75. https://doi.org/10.1007/s11695-012-0662-8.
Scopinaro N, Marinari GM, Camerini GB, et al. Specific effects of biliopancreatic diversion on the major components of metabolic syndrome: a long-term follow-up study. Diabetes Care. 2005;28(10):2406–11. https://doi.org/10.2337/diacare.28.10.2406.
Nogueira JP. Efecto de la cirugía bariatrica sobre el metabolismo de lipoproteinas ricas en trigliceridos. Rev. Cienc. Salud UP. 2019;1(1):57–66.
Franssen R, Monajemi H, Stroes ES, et al. Obesity and dyslipidemia. Med Clin North Am. 2011;95(5):893–902. https://doi.org/10.1016/j.mcna.2011.06.003.
Genua I, Ramos A, Caimari F, et al. Effects of bariatric surgery on HDL cholesterol. Obes Surg. 2020;30(5):1793–8. https://doi.org/10.1007/s11695-020-04385-8.
Heffron SP, Lin BX, Parikh M, et al. Changes in high-density lipoprotein cholesterol efflux capacity after bariatric surgery are procedure dependent. Arterioscler Thromb Vasc Biol. 2018;38(1):245–54. https://doi.org/10.1161/ATVBAHA.117.310102.
Mukorako P, Lopez C, Baraboi ED, et al. Alterations of gut microbiota after biliopancreatic diversion with duodenal switch in Wistar rats. Obes Surg. 2019 Sep;29(9):2831–42. https://doi.org/10.1007/s11695-019-03911-7.
Fruchart J-C, Sacks FM, Hermans MP, et al. The residual risk reduction initiative: a call to action to reduce residual vascular risk in dyslipidaemic patients. Diabetes Vasc Dis Res. 2008;5(4):319–35. https://doi.org/10.3132/dvdr.2008.046.
Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014 Aug 16;384(9943):626–35. https://doi.org/10.1016/S0140-6736(14)61177-6.
Wang L, Gill R, Pedersen TL, et al. Triglyceride-rich lipoprotein lipolysis releases neutral and oxidized FFAs that induce endothelial cell inflammation. J Lipid Res. 2009;50(2):204–13. https://doi.org/10.1194/jlr.M700505-JLR200.
Carr SS, Hooper AJ, Sullivan DR, et al. Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment. Pathology. 2019 Feb;51(2):148–54. https://doi.org/10.1016/j.pathol.2018.11.006.
Handelsman Y, Jellinger PS, Guerin CK, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the management of dyslipidemia and prevention of cardiovascular disease algorithm – 2020 executive summary. Endocrine Practice. 2020;26(10):1196–224. https://doi.org/10.4158/CS-2020-0490.
Sniderman AD, Thanassoulis G, Glavinovic T, et al. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019;4(12):1287–95. https://doi.org/10.1001/jamacardio.2019.3780.
Kohli-Lynch CN, Thanassoulis G, Moran AE, et al. The clinical utility of apoB versus LDL-C/non-HDL-C. Clin Chim Acta. 2020 Sep;508:103–8. https://doi.org/10.1016/j.cca.2020.05.001.
Spivak H, Sakran N, Dicker D, et al. Different effects of bariatric surgical procedures on dyslipidemia: a registry-based analysis. Surg Obes Relat Dis. 2017 Jul;13(7):1189–94. https://doi.org/10.1016/j.soard.2017.03.013. Epub 2017 Mar 23
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
-BS improves lipid profile.
-BPD reduces TC and LDL-c and improves residual cardiovascular risk.
-Type of surgery and baseline lipid level predict lipid variation 3 years after BS.
Rights and permissions
About this article
Cite this article
Arnáiz, E.G., Ballesteros Pomar, M.D., Roza, L.G. et al. Evaluation of Lipoprotein Profile and Residual Risk Three Years After Bariatric Surgery. OBES SURG 31, 4033–4044 (2021). https://doi.org/10.1007/s11695-021-05543-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05543-2