Abstract
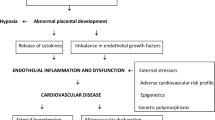
Pregnancy is a physiologically stressful condition that generates a series of functional adaptations by the cardiovascular system. The impact of pregnancy on this system persists from conception beyond birth. Recent evidence suggests that vascular changes associated with pregnancy complications, such as preeclampsia, affect the function of the maternal and offspring vascular systems, after delivery and into adult life. Since the vascular system contributes to systemic homeostasis, defective development or function of blood vessels predisposes both mother and infant to future risk for chronic disease. These alterations in later life range from fertility problems to alterations in the central nervous system or immune system, among others. It is important to note that rates of morbi-mortality due to pregnancy complications including preeclampsia, as well as cardiovascular diseases, have a higher incidence in Latin-American countries than in more developed countries. Nonetheless, there is a lack both in the amount and impact of research conducted in Latin America. An impact, although smaller, can be seen when research in vascular disorders related to problems during pregnancy is analyzed. Therefore, in this review, information about preeclampsia and endothelial dysfunction generated from research groups based in Latin-American countries will be highlighted. We relate the need, as present in many other countries in the world, for increased effective regional and international collaboration to generate new data specific to our region on this topic.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Xiong X, Demianczuk NN, Saunders LD, Wang FL, Fraser WD. Impact of preeclampsia and gestational hypertension on birth weight by gestational age. Am J Epidemiol. 2002;155(3):203–9.
Villar J, Carroli G, Wojdyla D, Abalos E, Giordano D, Ba’aqeel H, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194(4):921–31. https://doi.org/10.1016/j.ajog.2005.10.813.
Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365(9461):785–99.
Davis EF, Newton L, Lewandowski AJ, Lazdam M, Kelly BA, Kyriakou T, et al. Pre-eclampsia and offspring cardiovascular health: mechanistic insights from experimental studies. Clin Sci (Lond). 2012;123(2):53–72. https://doi.org/10.1042/CS20110627.
Glover V. Annual research review: prenatal stress and the origins of psychopathology: an evolutionary perspective. J Child Psychol Psychiatry. 2011;52(4):356–67. https://doi.org/10.1111/j.1469-7610.2011.02371.x.
Hanson MA, Gluckman PD. Developmental origins of health and disease: new insights. Basic Clin Pharmacol Toxicol. 2008;102(2):90–3. https://doi.org/10.1111/j.1742-7843.2007.00186.x.
Enkhmaa D, Wall D, Mehta PK, Stuart JJ, Rich-Edwards JW, Merz CN, et al. Preeclampsia and vascular function: a window to future cardiovascular disease risk. J Women’s Health (Larchmt). 2016;25(3):284–91. https://doi.org/10.1089/jwh.2015.5414.
Kattah AG, Scantlebury DC, Agarwal S, Mielke MM, Rocca WA, Weaver AL, et al. Preeclampsia and ESRD: the role of shared risk factors. Am J Kidney Dis. 2016; https://doi.org/10.1053/j.ajkd.2016.07.034.
Weissgerber TL, Milic NM, Milin-Lazovic JS, Garovic VD. Impaired flow-mediated dilation before, during, and after preeclampsia: a systematic review and meta-analysis. Hypertension. 2016;67(2):415–23. https://doi.org/10.1161/HYPERTENSIONAHA.115.06554.
Cirillo PM, Cohn BA. Pregnancy complications and cardiovascular disease death: 50-year follow-up of the child health and development studies pregnancy cohort. Circulation. 2015;132(13):1234–42. https://doi.org/10.1161/CIRCULATIONAHA.113.003901.
Seely EW, Rich-Edwards J, Lui J, Nicklas JM, Saxena A, Tsigas E, et al. Risk of future cardiovascular disease in women with prior preeclampsia: a focus group study. BMC Pregnancy Childbirth. 2013;13:240. https://doi.org/10.1186/1471-2393-13-240.
Mongraw-Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 2010;56(1):166–71. https://doi.org/10.1161/HYPERTENSIONAHA.110.150078.
Brunner H, Cockcroft JR, Deanfield J, Donald A, Ferrannini E, Halcox J, et al. Endothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. A statement by the working group on endothelins and endothelial factors of the European Society of Hypertension. J Hypertens. 2005;23(2):233–46.
Deanfield J, Donald A, Ferri C, Giannattasio C, Halcox J, Halligan S, et al. Endothelial function and dysfunction. Part I: methodological issues for assessment in the different vascular beds: a statement by the Working Group on Endothelin and Endothelial Factors of the European Society of Hypertension. J Hypertens. 2005;23(1):7–17.
• Roberts JM. Endothelial dysfunction in preeclampsia. Semin Reprod Endocrinol. 1998;16(1):5–15. https://doi.org/10.1055/s-2007-1016248.
• Roberts JM, Taylor RN, Musci TJ, Rodgers GM, Hubel CA, McLaughlin MK. Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol. 1989;161(5):1200–4.
Rodgers GM, Taylor RN, Roberts JM. Preeclampsia is associated with a serum factor cytotoxic to human endothelial cells. Am J Obstet Gynecol. 1988;159(4):908–14.
Wadsack C, Desoye G, Hiden U. The feto-placental endothelium in pregnancy pathologies. Wien Med Wochenschr. 2012;162(9–10):220–4. https://doi.org/10.1007/s10354-012-0075-2.
Sobrevia LG-G,E, Westermeier F, Salomón C, Arroyo P, Palacios E, Bugueño K, et al. Fetoplacental vascular pathophysiology in preeclampsia. In: Sobrevia L, editor. Recent research developments in physiology. India: Research Signpost; 2012. p. 105–58.
Kvehaugen AS, Dechend R, Ramstad HB, Troisi R, Fugelseth D, Staff AC. Endothelial function and circulating biomarkers are disturbed in women and children after preeclampsia. Hypertension. 2011;58(1):63–9. https://doi.org/10.1161/HYPERTENSIONAHA.111.172387.
• Jayet PY, Rimoldi SF, Stuber T, Salmon CS, Hutter D, Rexhaj E, et al. Pulmonary and systemic vascular dysfunction in young offspring of mothers with preeclampsia. Circulation. 2010;122(5):488–94. https://doi.org/10.1161/CIRCULATIONAHA.110.941203.
Lazdam M, de la Horra A, Pitcher A, Mannie Z, Diesch J, Trevitt C, et al. Elevated blood pressure in offspring born premature to hypertensive pregnancy: is endothelial dysfunction the underlying vascular mechanism? Hypertension. 2010;56(1):159–65. https://doi.org/10.1161/HYPERTENSIONAHA.110.150235.
Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33(3):130–7. https://doi.org/10.1053/j.semperi.2009.02.010.
Sliwa K, Bohm M. Incidence and prevalence of pregnancy-related heart disease. Cardiovasc Res. 2014;101(4):554–60. https://doi.org/10.1093/cvr/cvu012.
Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E, Sattar N, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation. 2012;125(11):1367–80. https://doi.org/10.1161/CIRCULATIONAHA.111.044784.
Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987-2004. Am J Hypertens. 2008;21(5):521–6. https://doi.org/10.1038/ajh.2008.20.
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000;183(1):S1-S22.
American College of O, Gynecologists, Task Force on Hypertension in P. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–31. https://doi.org/10.1097/01.AOG.0000437382.03963.88.
WHO. Maternal mortality. Data by WHO region. 2016. http://apps.who.int/gho/data/view.main.1370?lang=en. 2016.
• Roost M, Altamirano VC, Liljestrand J, Essen B. Priorities in emergency obstetric care in Bolivia—maternal mortality and near-miss morbidity in metropolitan La Paz. BJOG. 2009;116(9):1210–7. https://doi.org/10.1111/j.1471-0528.2009.02209.x.
Khowaja AR, Mitton C, Bryan S, Magee LA, Bhutta ZA, von Dadelszen P. Economic evaluation of community level interventions for pre-eclampsia (CLIP) in South Asian and African countries: a study protocol. Implement Sci. 2015;10(1):76. https://doi.org/10.1186/s13012-015-0266-5.
• Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–74. https://doi.org/10.1016/S0140-6736(06)68397-9.
• Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011;25(4):391–403. https://doi.org/10.1016/j.bpobgyn.2011.01.006.
• Foundation P. Preeclampsia: a decade of perspective, building a global call to action., Melbourne, Florida. 2010.
• Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):1–7. https://doi.org/10.1016/j.ejogrb.2013.05.005.
México. SdSCNdEdGySR. Prevención, diagnóstico y manejo de la preeclampsia/eclampsia. Lineamiento Técnico. Mexico 2007.
Teran E, Escudero C, Vivero S, Molina G, Calle A. NO in early pregnancy and development of preeclampsia. Hypertension. 2006;47(4):e17. https://doi.org/10.1161/01.HYP.0000205226.01641.fe.
Teran E, Hernandez I, Nieto B, Tavara R, Ocampo JE, Calle A. Coenzyme Q10 supplementation during pregnancy reduces the risk of pre-eclampsia. Int J Gynaecol Obstet. 2009;105(1):43–5. https://doi.org/10.1016/j.ijgo.2008.11.033.
Ronsmans C, Graham WJ. Lancet maternal survival series steering g. Maternal mortality: who, when, where, and why. Lancet. 2006;368(9542):1189–200. https://doi.org/10.1016/S0140-6736(06)69380-X.
Urquia ML, Glazier RH, Gagnon AJ, Mortensen LH, Nybo Andersen AM, Janevic T, et al. Disparities in pre-eclampsia and eclampsia among immigrant women giving birth in six industrialised countries. BJOG. 2014;121(12):1492–500. https://doi.org/10.1111/1471-0528.12758.
Porreco RP, Barkey R. Peripartum intensive care. J Matern Fetal Neonatal Med. 2010;23(10):1136–8. https://doi.org/10.3109/14767058.2010.490890.
Corominas AI BS, Palermo M, Maskin B, Damiano AE. Maternal hypertensive environment and postnatal susceptibility to disease. Placenta. 2013;34(A32).
Bertoglia PRA, Navarrete P, Castro L, Acurio J, Escudero C. Resultados clínicos y perinatales de los embarazos con hipertensión arterial en un hospital de referencia de la VIII región de Chile. Rev Chil Obstet Ginecol. 2010;75(3):162–71.
Burton GJ, Charnock-Jones DS, Jauniaux E. Regulation of vascular growth and function in the human placenta. Reproduction. 2009;138(6):895–902. https://doi.org/10.1530/REP-09-0092.
Burton GJ, Woods AW, Jauniaux E, Kingdom JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30(6):473–82.
Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005;308(5728):1592–4. https://doi.org/10.1126/science.1111726.
Redman CW, Sargent IL. Placental debris, oxidative stress and pre-eclampsia. Placenta. 2000;21(7):597–602. https://doi.org/10.1053/plac.2000.0560.
Tannetta DS, Dragovic RA, Gardiner C, Redman CW, Sargent IL. Characterisation of syncytiotrophoblast vesicles in normal pregnancy and pre-eclampsia: expression of flt-1 and endoglin. PLoS One. 2013;8(2):e56754. https://doi.org/10.1371/journal.pone.0056754.
Roberts JM, Escudero C. The placenta in preeclampsia. Hypertens Pregnancy. 2012;2(2):72–83.
Escudero C, Roberts JM, Myatt L, Feoktistov I. Impaired adenosine-mediated angiogenesis in preeclampsia: potential implications for fetal programming. Front Pharmacol. 2014;5:134. https://doi.org/10.3389/fphar.2014.00134.
Germain SJ, Sacks GP, Sooranna SR, Sargent IL, Redman CW. Systemic inflammatory priming in normal pregnancy and preeclampsia: the role of circulating syncytiotrophoblast microparticles. J Immunol. 2007;178(9):5949–56.
Agarwal I, Karumanchi SA. Preeclampsia and the anti-angiogenic state. Pregnancy Hypertens. 2011;1(1):17–21. https://doi.org/10.1016/j.preghy.2010.10.007.
Levine RJ, Karumanchi SA. Circulating angiogenic factors in preeclampsia. Clin Obstet Gynecol. 2005;48(2):372–86.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355(10):992–1005. https://doi.org/10.1056/NEJMoa055352.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672–83. https://doi.org/10.1056/NEJMoa031884.
Levine RJ, Qian C, Maynard SE, Yu KF, Epstein FH, Karumanchi SA. Serum sFlt1 concentration during preeclampsia and mid trimester blood pressure in healthy nulliparous women. Am J Obstet Gynecol. 2006;194(4):1034–41. https://doi.org/10.1016/j.ajog.2005.10.192.
Levine RJ, Thadhani R, Qian C, Lam C, Lim KH, Yu KF, et al. Urinary placental growth factor and risk of preeclampsia. JAMA. 2005;293(1):77–85. https://doi.org/10.1001/jama.293.1.77.
Maynard SE, Karumanchi SA. Angiogenic factors and preeclampsia. Semin Nephrol. 2011;31(1):33–46. https://doi.org/10.1016/j.semnephrol.2010.10.004.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111(5):649–58. https://doi.org/10.1172/JCI17189.
Silasi M, Cohen B, Karumanchi SA, Rana S. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin N Am. 2010;37(2):239–53. https://doi.org/10.1016/j.ogc.2010.02.013.
Sunderji S, Gaziano E, Wothe D, Rogers LC, Sibai B, Karumanchi SA, et al. Automated assays for sVEGF R1 and PlGF as an aid in the diagnosis of preterm preeclampsia: a prospective clinical study. Am J Obstet Gynecol. 2010;202(1):40 e1–7. https://doi.org/10.1016/j.ajog.2009.07.025.
Chen DB, Wang W. Human placental microRNAs and preeclampsia. Biol Reprod. 2013;88(5):130. https://doi.org/10.1095/biolreprod.113.107805.
Fu G, Brkic J, Hayder H, Peng C. MicroRNAs in human placental development and pregnancy complications. Int J Mol Sci. 2013;14(3):5519–44. https://doi.org/10.3390/ijms14035519.
Escudero CA, Herlitz K, Troncoso F, Acurio J, Aguayo C, Roberts JM, et al. Role of extracellular vesicles and microRNAs on dysfunctional angiogenesis during preeclamptic pregnancies. Front Physiol. 2016;7:98. https://doi.org/10.3389/fphys.2016.00098.
• Cheng PJ, Huang SY, Su SY, Hsiao CH, Peng HH, Duan T. Prognostic value of cardiovascular disease risk factors measured in the first-trimester on the severity of preeclampsia. Medicine (Baltimore). 2016;95(5):e2653. https://doi.org/10.1097/MD.0000000000002653.
Reyes LM, Garcia RG, Ruiz SL, Broadhurst D, Aroca G, Davidge ST, et al. Angiogenic imbalance and plasma lipid alterations in women with preeclampsia from a developing country. Growth Factors. 2012;30(3):158–66. https://doi.org/10.3109/08977194.2012.674035.
Parra M, Rodrigo R, Barja P, Bosco C, Fernandez V, Munoz H, et al. Screening test for preeclampsia through assessment of uteroplacental blood flow and biochemical markers of oxidative stress and endothelial dysfunction. Am J Obstet Gynecol. 2005;193(4):1486–91. https://doi.org/10.1016/j.ajog.2005.02.109.
Kienast C, Moya W, Rodriguez O, Jijon A, Geipel A. Predictive value of angiogenic factors, clinical risk factors and uterine artery Doppler for pre-eclampsia and fetal growth restriction in second and third trimester pregnancies in an Ecuadorian population. J Matern Fetal Neonatal Med. 2016;29(4):537–43. https://doi.org/10.3109/14767058.2015.1012063.
• Widmer M, Cuesta C, Khan KS, Conde-Agudelo A, Carroli G, Fusey S, et al. Accuracy of angiogenic biomarkers at 20 weeks’ gestation in predicting the risk of pre-eclampsia: a WHO multicentre study. Pregnancy Hypertens. 2015;5(4):330–8. https://doi.org/10.1016/j.preghy.2015.09.004.
Leanos-Miranda A, Mendez-Aguilar F, Ramirez-Valenzuela KL, Serrano-Rodriguez M, Berumen-Lechuga G, Molina-Perez CJ, et al. Circulating angiogenic factors are related to the severity of gestational hypertension and preeclampsia, and their adverse outcomes. Medicine (Baltimore). 2017;96(4):e6005. https://doi.org/10.1097/MD.0000000000006005.
Weel IC, Baergen RN, Romao-Veiga M, Borges VT, Ribeiro VR, Witkin SS, et al. Association between placental lesions, cytokines and angiogenic factors in pregnant women with preeclampsia. PLoS One. 2016;11(6):e0157584. https://doi.org/10.1371/journal.pone.0157584.
Perales A, Delgado JL, De La Calle M, Garcia-Hernandez JA, Escudero AI, Campillos JM, et al. sFlt-1/PlGF for early-onset pre-eclampsia prediction: STEPS (study of early pre-eclampsia in Spain). Ultrasound Obstet Gynecol. 2016; https://doi.org/10.1002/uog.17373.
Khalil A, Maiz N, Garcia-Mandujano R, Penco JM, Nicolaides KH. Longitudinal changes in maternal serum placental growth factor and soluble fms-like tyrosine kinase-1 in women at increased risk of pre-eclampsia. Ultrasound Obstet Gynecol. 2016;47(3):324–31. https://doi.org/10.1002/uog.15750.
Rios DR, Alpoim PN, Godoi LC, Perucci LO, de Sousa LP, Gomes KB et al. Increased levels of sENG and sVCAM-1 and decreased levels of VEGF in severe preeclampsia. Am J Hypertens. 2015.
March MI, Geahchan C, Wenger J, Raghuraman N, Berg A, Haddow H, et al. Circulating angiogenic factors and the risk of adverse outcomes among Haitian women with preeclampsia. PLoS One. 2015;10(5):e0126815. https://doi.org/10.1371/journal.pone.0126815.
Crovetto F, Figueras F, Triunfo S, Crispi F, Rodriguez-Sureda V, Peguero A, et al. Added value of angiogenic factors for the prediction of early and late preeclampsia in the first trimester of pregnancy. Fetal Diagn Ther. 2014;35(4):258–66. https://doi.org/10.1159/000358302.
Hund M, Allegranza D, Schoedl M, Dilba P, Verhagen-Kamerbeek W, Stepan H. Multicenter prospective clinical study to evaluate the prediction of short-term outcome in pregnant women with suspected preeclampsia (PROGNOSIS): study protocol. BMC Pregnancy Childbirth. 2014;14:324. https://doi.org/10.1186/1471-2393-14-324.
Herraiz I, Droge LA, Gomez-Montes E, Henrich W, Galindo A, Verlohren S. Characterization of the soluble fms-like tyrosine kinase-1 to placental growth factor ratio in pregnancies complicated by fetal growth restriction. Obstet Gynecol. 2014;124(2 Pt 1):265–73. https://doi.org/10.1097/AOG.0000000000000367.
Leanos-Miranda A, Campos-Galicia I, Isordia-Salas I, Rivera-Leanos R, Romero-Arauz JF, Ayala-Mendez JA, et al. Changes in circulating concentrations of soluble fms-like tyrosine kinase-1 and placental growth factor measured by automated electrochemiluminescence immunoassays methods are predictors of preeclampsia. J Hypertens. 2012;30(11):2173–81. https://doi.org/10.1097/HJH.0b013e328357c0c9.
Paez MC, Serrano NC, Diaz LA, Beltran MA, Ortiz R, Monterrosa A, et al. O2. Serum concentrations of angiogenic factors as predictors of severity of preeclampsia, in Colombian population. Pregnancy Hypertens. 2011;1(3–4):258. https://doi.org/10.1016/j.preghy.2011.08.034.
Kusanovic JP, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, et al. A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med. 2009;22(11):1021–38. https://doi.org/10.3109/14767050902994754.
Chedraui P, Lockwood CJ, Schatz F, Buchwalder LF, Schwager G, Guerrero C, et al. Increased plasma soluble fms-like tyrosine kinase 1 and endoglin levels in pregnancies complicated with preeclampsia. J Matern Fetal Neonatal Med. 2009;22(7):565–70. https://doi.org/10.1080/14767050902801769.
Giorgi VS, Witkin SS, Bannwart-Castro CF, Sartori MS, Romao-Veiga M, Borges VT, et al. Elevated circulatingadenosine deaminase activity in women with preeclampsia: association with pro-inflammatory cytokine production and uric acid levels. Pregnancy Hypertens. 2016;6(4):400–5.
Poveda NE, Garces MF, Ruiz-Linares CE, Varon D, Valderrama S, Sanchez E, et al. Serum adipsin levels throughout normal pregnancy and preeclampsia. Sci Rep. 2016;6:20073. https://doi.org/10.1038/srep20073.
Perucci LO, Vieira EL, Teixeira AL, Gomes KB, Dusse LM, Sousa LP. Decreased plasma concentrations of brain-derived neurotrophic factor in preeclampsia. Clin Chim Acta. 2017;464:142–7.
Teran E, Escudero C, Calle A. C-reactive protein during normal pregnancy and preeclampsia. Int J Gynaecol Obstet. 2005;89(3):299–300. https://doi.org/10.1016/j.ijgo.2005.02.002.
Lopez-Hernandez Y, Saldivar-Nava JA, Garza-Veloz I, Delgado-Enciso I, Martinez-de-Villarreal LE, Yahuaca-Mendoza P, et al. Nested case-control study reveals increased levels of urinary proteins from human kidney toxicity panels in women predicted to develop preeclampsia. Int Urol Nephrol. 2016;48(12):2051–9. https://doi.org/10.1007/s11255-016-1397-6.
Aban C, Leguizamon GF, Cella M, Damiano A, Franchi AM, Farina MG. Differential expression of endocannabinoid system in normal and preeclamptic placentas: effects on nitric oxide synthesis. Placenta. 2013;34(1):67–74. https://doi.org/10.1016/j.placenta.2012.10.009.
Parra-Cordero M, Sepulveda-Martinez A, Preisler J, Pasten J, Soto-Chacon E, Valdes E, et al. Role of the glucose tolerance test as a predictor of preeclampsia. Gynecol Obstet Investig. 2014;78(2):130–5. https://doi.org/10.1159/000358876.
Martinez-Fierro ML, Perez-Favila A, Garza-Veloz I, Espinoza-Juarez MA, Avila-Carrasco L, Delgado-Enciso I, et al. Matrix metalloproteinase multiplex screening identifies increased MMP-2 urine concentrations in women predicted to develop preeclampsia. Biomarkers. 2017:1–7. https://doi.org/10.1080/1354750X.2017.1279214.
Palei AC, Sandrim VC, Amaral LM, Machado JS, Cavalli RC, Duarte G, et al. Association between matrix metalloproteinase (MMP)-2 polymorphisms and MMP-2 levels in hypertensive disorders of pregnancy. Exp Mol Pathol. 2012;92(2):217–21. https://doi.org/10.1016/j.yexmp.2012.01.008.
Garces MF, Sanchez E, Cardona LF, Simanca EL, Gonzalez I, Leal LG, et al. Maternal serum meteorin levels and the risk of preeclampsia. PLoS One. 2015;10(6):e0131013. https://doi.org/10.1371/journal.pone.0131013.
Perez-Sepulveda A, Torres MJ, Valenzuela FJ, Larrain R, Figueroa-Diesel H, Galaz J, et al. Low 2-methoxyestradiol levels at the first trimester of pregnancy are associated with the development of pre-eclampsia. Prenat Diagn. 2012;32(11):1053–8. https://doi.org/10.1002/pd.3954.
Palacios de Franco Y, Velazquez K, Segovia N, Acosta C, Yanosky D, Franco Palacios YV, et al. Urinary podocalyxin as a marker of preeclampsia in a Hispanic population. Int J Physiol Pathophysiol Pharmacol. 2014;6(2):115–24.
Dietrich V, Szpilbarg N, Damiano AE. Reduced expression of Na(+)/H(+) exchanger isoform 3 (NHE-3) in preeclamptic placentas. Placenta. 2013;34(9):828–30. https://doi.org/10.1016/j.placenta.2013.06.005.
Chamy VM, Lepe J, Catalan A, Retamal D, Escobar JA, Madrid EM. Oxidative stress is closely related to clinical severity of pre-eclampsia. Biol Res. 2006;39(2):229–36.
Ayala-Ramirez P, Buitrago T, Poveda A, Rodriguez JL, Olaya CM, Garcia-Robles R. Increased tissue factor and thrombomodulin expression and histopathological changes in placentas of pregnancies with preeclampsia. J Neonatal Perinatal Med. 2016;9(1):31–9. https://doi.org/10.3233/NPM-16915034.
• von Dadelszen P, Payne B, Li J, Ansermino JM, Broughton Pipkin F, Cote AM, et al. Prediction of adverse maternal outcomes in pre-eclampsia: development and validation of the fullPIERS model. Lancet. 2011;377(9761):219–27. https://doi.org/10.1016/S0140-6736(10)61351-7.
• Almeida ST, Katz L, Coutinho I, Amorim MMR. Validation of fullPIERS model for prediction of adverse outcomes among women with severe pre-eclampsia. Int J Gynaecol Obstet. 2017; https://doi.org/10.1002/ijgo.12197.
Haukkamaa L, Moilanen L, Kattainen A, Luoto R, Kahonen M, Leinonen M, et al. Pre-eclampsia is a risk factor of carotid artery atherosclerosis. Cerebrovasc Dis. 2009;27(6):599–607. https://doi.org/10.1159/000216834.
• Agatisa PK, Ness RB, Roberts JM, Costantino JP, Kuller LH, McLaughlin MK. Impairment of endothelial function in women with a history of preeclampsia: an indicator of cardiovascular risk. Am J Physiol Heart Circ Physiol. 2004;286(4):H1389–93. https://doi.org/10.1152/ajpheart.00298.2003.
Davis EF, Lazdam M, Lewandowski AJ, Worton SA, Kelly B, Kenworthy Y, et al. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics. 2012;129(6):e1552–61. https://doi.org/10.1542/peds.2011-3093.
Evans CS, Gooch L, Flotta D, Lykins D, Powers RW, Landsittel D, et al. Cardiovascular system during the postpartum state in women with a history of preeclampsia. Hypertension. 2011; https://doi.org/10.1161/HYPERTENSIONAHA.111.173278.
Valdes G, Quezada F, Marchant E, von Schultzendorff A, Moran S, Padilla O, et al. Association of remote hypertension in pregnancy with coronary artery disease: a case-control study. Hypertension. 2009;53(4):733–8. https://doi.org/10.1161/HYPERTENSIONAHA.108.127068.
• Germain AM, Romanik MC, Guerra I, Solari S, Reyes MS, Johnson RJ, et al. Endothelial dysfunction: a link among preeclampsia, recurrent pregnancy loss, and future cardiovascular events? Hypertension. 2007;49(1):90–5. https://doi.org/10.1161/01.HYP.0000251522.18094.d4.
• Galvão ACAdA. Sindrome metabólica e fatores de risco associados: estudo comparativo entre mulheres que apresentaram pre-eclampsia e gravidez normal, acompanhadas 5 anos após o parto. Tese de Doutorado, Universidade Federal do Rio Grande do Norte. 2013.
Silva MdLCd, Araújo ACPFd. Doenças cardiovasculares em mulheres com histórico de pré-eclampsia e segmento no Sistema Único de Saúde. Tese de Doutorado: Universidade Federal do Rio Grande do Norte. 2013.
Ferreira RM, Bazan SGZ, Martin LC. Cardiovascular risk factors in women with preeclampsia history and their association with myocardial hypertrophy and intima-media thickening of the carotids. Tese de Doutorado, Faculdade de Medicina, Universidade Estadual de São Paulo, Botucatu. 2016.
• Henriques AC, Carvalho FH, Feitosa HN, Macena RH, Mota RM, Alencar JC. Endothelial dysfunction after pregnancy-induced hypertension. Int J Gynaecol Obstet. 2014;124(3):230–4. https://doi.org/10.1016/j.ijgo.2013.08.016.
• Torrado J, Farro I, Zocalo Y, Farro F, Sosa C, Scasso S, et al. Preeclampsia is associated with increased central aortic pressure, elastic arteries stiffness and wave reflections, and resting and recruitable endothelial dysfunction. Int J Hypertens. 2015;2015:720683. https://doi.org/10.1155/2015/720683.
• Serrano-Diaz N, Paez-Leal M, Beltran-Avendano M, Colmenares-Mejia C, Guio-Mahecha E, Bautista-Nino P, et al. Preeclampsia y riesgo cardiovascular: estudio de seguimiento en la poblacion de GenPE en Colombia. Revista Colombiana de Obstetricia y Ginecologia. 2012;63(3):241–51.
Goynumer G, Yucel N, Adali E, Tan T, Baskent E, Karadag C. Vascular risk in women with a history of severe preeclampsia. J Clin Ultrasound. 2013;41(3):145–50. https://doi.org/10.1002/jcu.21962.
Blaauw J, van Pampus MG, Van Doormaal JJ, Fokkema MR, Fidler V, Smit AJ, et al. Increased intima-media thickness after early-onset preeclampsia. Obstet Gynecol. 2006;107(6):1345–51.
Blaauw J, Souwer ET, Coffeng SM, Smit AJ, van Doormaal JJ, Faas MM, et al. Follow up of intima-media thickness after severe early-onset preeclampsia. Acta Obstet Gynecol Scand. 2014;93(12):1309–16. https://doi.org/10.1111/aogs.12499.
Sandvik MK, Leirgul E, Nygard O, Ueland PM, Berg A, Svarstad E, et al. Preeclampsia in healthy women and endothelial dysfunction 10 years later. Am J Obstet Gynecol. 2013;209(6):569 e1–e10. https://doi.org/10.1016/j.ajog.2013.07.024.
Franz MB, Burgmann M, Neubauer A, Zeisler H, Sanani R, Gottsauner-Wolf M, et al. Augmentation index and pulse wave velocity in normotensive and pre-eclamptic pregnancies. Acta Obstet Gynecol Scand. 2013;92(8):960–6. https://doi.org/10.1111/aogs.12145.
Karkkainen H, Saarelainen H, Laitinen T, Heiskanen N, Valtonen P, Vanninen E, et al. Ambulatory arterial stiffness index and nocturnal blood pressure dipping in pregnancies complicated by hypertension. Clin Physiol Funct Imaging. 2014;34(1):39–46. https://doi.org/10.1111/cpf.12063.
• Ehrenthal DB, Goldstein ND, Wu P, Rogers S, Townsend RR, Edwards DG. Arterial stiffness and wave reflection 1 year after a pregnancy complicated by hypertension. J Clin Hypertens (Greenwich). 2014;16(10):695–9. https://doi.org/10.1111/jch.12398.
• Grand’Maison S, Pilote L, Okano M, Landry T, Dayan N. Markers of vascular dysfunction after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Hypertension. 2016;68(6):1447–58.
Harville EW, Juonala M, Viikari JS, Kahonen M, Raitakari OT. Vascular ultrasound measures before pregnancy and pregnancy complications: a prospective cohort study. Hypertens Pregnancy. 2016;36:1–6. https://doi.org/10.1080/10641955.2016.1237643.
Akhter T, Wikstrom AK, Larsson M, Larsson A, Wikstrom G, Naessen T. Association between angiogenic factors and signs of arterial aging in women with pre-eclampsia. Ultrasound Obstet Gynecol. 2016; https://doi.org/10.1002/uog.15981.
Marin R, Gorostidi M, Portal CG, Sanchez M, Sanchez E, Alvarez J. Long-term prognosis of hypertension in pregnancy. Hypertens Pregnancy. 2000;19(2):199–209.
Dantas EM, Pereira FV, Queiroz JW, Dantas DL, Monteiro GR, Duggal P, et al. Preeclampsia is associated with increased maternal body weight in a northeastern Brazilian population. BMC Pregnancy Childbirth. 2013;13:159. https://doi.org/10.1186/1471-2393-13-159.
Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG. 2014;121(Suppl 1):14–24. https://doi.org/10.1111/1471-0528.12629.
Wiegman MJ, Zeeman GG, Aukes AM, Bolte AC, Faas MM, Aarnoudse JG, et al. Regional distribution of cerebral white matter lesions years after preeclampsia and eclampsia. Obstet Gynecol. 2014;123(4):790–5. https://doi.org/10.1097/AOG.0000000000000162.
Aukes AM, de Groot JC, Aarnoudse JG, Zeeman GG. Brain lesions several years after eclampsia. Am J Obstet Gynecol. 2009;200(5):504 e1–5. https://doi.org/10.1016/j.ajog.2008.12.033.
Aukes AM, De Groot JC, Wiegman MJ, Aarnoudse JG, Sanwikarja GS, Zeeman GG. Long-term cerebral imaging after pre-eclampsia. BJOG. 2012;119(9):1117–22. https://doi.org/10.1111/j.1471-0528.2012.03406.x.
• Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28(1):1–19. https://doi.org/10.1007/s10654-013-9762-6.
• Siepmann T, Boardman H, Bilderbeck A, Griffanti L, Kenworthy Y, Zwager C, et al. Long-term cerebral white and gray matter changes after preeclampsia. Neurology. 2017;88(13):1256–64. https://doi.org/10.1212/WNL.0000000000003765.
• Logue OC, George EM, Bidwell GL 3rd. Preeclampsia and the brain: neural control of cardiovascular changes during pregnancy and neurological outcomes of preeclampsia. Clin Sci (Lond). 2016;130(16):1417–34. https://doi.org/10.1042/CS20160108.
Alves Borges JH, Goes DA, de Araujo LB, Dos Santos MC, Debs Diniz AL. Prospective study of the hemodynamic behavior of ophthalmic arteries in postpartum preeclamptic women: a Doppler evaluation. Hypertens Pregnancy. 2016;35(1):100–11. https://doi.org/10.3109/10641955.2015.1116553.
Wiegman MJ, de Groot JC, Jansonius NM, Aarnoudse JG, Groen H, Faas MM, et al. Long-term visual functioning after eclampsia. Obstet Gynecol. 2012;119(5):959–66. https://doi.org/10.1097/AOG.0b013e31824da5a8.
Vikse BE, Irgens LM, Bostad L, Iversen BM. Adverse perinatal outcome and later kidney biopsy in the mother. J Am Soc Nephrol. 2006;17(3):837–45.
Henao DE, Arias LF, Mathieson PW, Ni L, Welsh GI, Bueno JC, et al. Preeclamptic sera directly induce slit-diaphragm protein redistribution and alter podocyte barrier-forming capacity. Nephron Exp Nephrol. 2008;110(3):e73–81. https://doi.org/10.1159/000166993.
Penning ME, Bloemenkamp KW, van der Zon T, Zandbergen M, Schutte JM, Bruijn JA, et al. Association of preeclampsia with podocyte turnover. Clin J Am Soc Nephrol. 2014;9(8):1377–85. https://doi.org/10.2215/CJN.12811213.
White WM, Garrett AT, Craici IM, Wagner SJ, Fitz-Gibbon PD, Butters KA, et al. Persistent urinary podocyte loss following preeclampsia may reflect subclinical renal injury. PLoS One. 2014;9(3):e92693. https://doi.org/10.1371/journal.pone.0092693.
Shahbazian N, Shahbazian H, Ehsanpour A, Aref A, Gharibzadeh S. Hypertension and microalbuminuria 5 years after pregnancies complicated by pre-eclampsia. Iran J Kidney Dis. 2011;5(5):324–7.
Gaugler-Senden IP, Berends AL, de Groot CJ, Steegers EA. Severe, very early onset preeclampsia: subsequent pregnancies and future parental cardiovascular health. Eur J Obstet Gynecol Reprod Biol. 2008;140(2):171–7. https://doi.org/10.1016/j.ejogrb.2008.03.004.
Shammas AG, Maayah JF. Hypertension and its relation to renal function 10 years after pregnancy complicated by pre-eclampsia and pregnancy induced hypertension. Saudi Med J. 2000;21(2):190–2.
Bar J, Kaplan B, Wittenberg C, Erman A, Boner G, Ben-Rafael Z, et al. Microalbuminuria after pregnancy complicated by pre-eclampsia. Nephrol Dial Transplant. 1999;14(5):1129–32.
Nisell H, Lintu H, Lunell NO, Mollerstrom G, Pettersson E. Blood pressure and renal function seven years after pregnancy complicated by hypertension. Br J Obstet Gynaecol. 1995;102(11):876–81.
Sandvik MK, Hallan S, Svarstad E, Vikse BE. Preeclampsia and prevalence of microalbuminuria 10 years later. Clin J Am Soc Nephrol. 2013;8(7):1126–34. https://doi.org/10.2215/CJN.10641012.
Vikse BE, Hallan S, Bostad L, Leivestad T, Iversen BM. Previous preeclampsia and risk for progression of biopsy-verified kidney disease to end-stage renal disease. Nephrol Dial Transplant. 2010;25(10):3289–96. https://doi.org/10.1093/ndt/gfq169.
• Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974. https://doi.org/10.1136/bmj.39335.385301.BE.
Lawlor DA, Macdonald-Wallis C, Fraser A, Nelson SM, Hingorani A, Davey Smith G, et al. Cardiovascular biomarkers and vascular function during childhood in the offspring of mothers with hypertensive disorders of pregnancy: findings from the Avon Longitudinal Study of Parents and Children. Eur Heart J. 2012;33(3):335–45. https://doi.org/10.1093/eurheartj/ehr300.
• Kajantie E, Eriksson JG, Osmond C, Thornburg K, Barker DJ. Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki birth cohort study. Stroke. 2009;40(4):1176–80.
Wu CS, Nohr EA, Bech BH, Vestergaard M, Catov JM, Olsen J. Health of children born to mothers who had preeclampsia: a population-based cohort study. Am J Obstet Gynecol. 2009;201(3):269 e1–e10. https://doi.org/10.1016/j.ajog.2009.06.060.
Wu CS, Nohr EA, Bech BH, Vestergaard M, Catov JM, Olsen J. Diseases in children born to mothers with preeclampsia: a population-based sibling cohort study. Am J Obstet Gynecol. 2011;204(2):157 e1–5. https://doi.org/10.1016/j.ajog.2010.08.046.
• Bellizzi S, Ali MM, Abalos E, Betran AP, Kapila J, Pileggi-Castro C, et al. Are hypertensive disorders in pregnancy associated with congenital malformations in offspring? Evidence from the WHO multicountry cross sectional survey on maternal and newborn health. BMC Pregnancy Childbirth. 2016;16(1):198. https://doi.org/10.1186/s12884-016-0987-8.
• Alsnes IV, Vatten LJ, Fraser A, Bjorngaard JH, Rich-Edwards J, Romundstad PR, et al. Hypertension in pregnancy and offspring cardiovascular risk in young adulthood: prospective and sibling studies in the HUNT study (Nord-Trondelag Health Study) in Norway. Hypertension. 2017;69(4):591–8. https://doi.org/10.1161/HYPERTENSIONAHA.116.08414.
Yu GZ, Leeson P. Hypertension: hypertension in pregnancy: a risk factor for the whole family? Nat Rev Nephrol. 2017;13(6):326–7. https://doi.org/10.1038/nrneph.2017.54.
Timpka S, Macdonald-Wallis C, Hughes AD, Chaturvedi N, Franks PW, Lawlor DA et al. Hypertensive disorders of pregnancy and offspring cardiac structure and function in adolescence. J Am Heart Assoc. 2016;5(11). https://doi.org/10.1161/JAHA.116.003906.
• Yesil GD, Gishti O, Felix JF, Reiss I, Ikram MK, Steegers EA, et al. Influence of maternal gestational hypertensive disorders on microvasculature in school-age children: the generation R study. Am J Epidemiol. 2016;184(9):605–15. https://doi.org/10.1093/aje/kww059.
• Yu GZ, Aye CY, Lewandowski AJ, Davis EF, Khoo CP, Newton L, et al. Association of maternal antiangiogenic profile at birth with early postnatal loss of microvascular density in offspring of hypertensive pregnancies. Hypertension. 2016;68(3):749–59. https://doi.org/10.1161/HYPERTENSIONAHA.116.07586.
• Ratsep MT, Paolozza A, Hickman AF, Maser B, Kay VR, Mohammad S, et al. Brain structural and vascular anatomy is altered in offspring of pre-eclamptic pregnancies: a pilot study. AJNR Am J Neuroradiol. 2016;37(5):939–45. https://doi.org/10.3174/ajnr.A4640.
Dang F, Croy BA, Stroman PW, Figueiro-Filho EA. Impacts of preeclampsia on the brain of the offspring. Rev Bras Ginecol Obstet. 2016;38(8):416–22. https://doi.org/10.1055/s-0036-1584515.
Ratsep MT, Hickman AF, Croy BA. The Elsevier trophoblast research award lecture: impacts of placental growth factor and preeclampsia on brain development, behaviour, and cognition. Placenta. 2016;48(Suppl 1):S40–S6.
Tuovinen S, Raikkonen K, Kajantie E, Pesonen AK, Heinonen K, Osmond C, et al. Depressive symptoms in adulthood and intrauterine exposure to pre-eclampsia: the Helsinki Birth Cohort Study. BJOG. 2010;117(10):1236–42. https://doi.org/10.1111/j.1471-0528.2010.02634.x.
Szymonowicz W, Yu VY. Severe pre-eclampsia and infants of very low birth weight. Arch Dis Child. 1987;62(7):712–6.
Cheng SW, Chou HC, Tsou KI, Fang LJ, Tsao PN. Delivery before 32 weeks of gestation for maternal pre-eclampsia: neonatal outcome and 2-year developmental outcome. Early Hum Dev. 2004;76(1):39–46.
Griffith MI, Mann JR, McDermott S. The risk of intellectual disability in children born to mothers with preeclampsia or eclampsia with partial mediation by low birth weight. Hypertens Pregnancy. 2011;30(1):108–15. https://doi.org/10.3109/10641955.2010.507837.
Johnson S, Evans TA, Draper ES, Field DJ, Manktelow BN, Marlow N, et al. Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed. 2015;100(4):F301–8. https://doi.org/10.1136/archdischild-2014-307684.
Ratsep MT, Hickman AF, Maser B, Pudwell J, Smith GN, Brien D, et al. Impact of preeclampsia on cognitive function in the offspring. Behav Brain Res. 2016;302:175–81. https://doi.org/10.1016/j.bbr.2016.01.030.
Whitehouse AJ, Robinson M, Newnham JP, Pennell CE. Do hypertensive diseases of pregnancy disrupt neurocognitive development in offspring? Paediatr Perinat Epidemiol. 2012;26(2):101–8. https://doi.org/10.1111/j.1365-3016.2011.01257.x.
Robinson M, Mattes E, Oddy WH, de Klerk NH, Li J, McLean NJ, et al. Hypertensive diseases of pregnancy and the development of behavioral problems in childhood and adolescence: the Western Australian Pregnancy Cohort Study. J Pediatr. 2009;154(2):218–24. https://doi.org/10.1016/j.jpeds.2008.07.061.
Alsnes IV, Janszky I, Asvold BO, Okland I, Forman MR, Vatten LJ. Maternal preeclampsia and androgens in the offspring around puberty: a follow-up study. PLoS One. 2016;11(12):e0167714. https://doi.org/10.1371/journal.pone.0167714.
Boeldt DS, Bird IM. Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol. 2017;232(1):R27–44. https://doi.org/10.1530/JOE-16-0340.
Sanchez-Aranguren LC, Prada CE, Riano-Medina CE, Lopez M. Endothelial dysfunction and preeclampsia: role of oxidative stress. Front Physiol. 2014;5:372. https://doi.org/10.3389/fphys.2014.00372.
Weissgerber TL, Turner ST, Mosley TH Jr, Kardia SL, Hanis CL, Milic NM, et al. Hypertension in pregnancy and future cardiovascular event risk in siblings. J Am Soc Nephrol. 2016;27(3):894–902. https://doi.org/10.1681/ASN.2015010086.
Teran E, Chedraui P, Vivero S, Villena F, Duchicela F, Nacevilla L. Plasma and placental nitric oxide levels in women with and without pre-eclampsia living at different altitudes. Int J Gynaecol Obstet. 2009;104(2):140–2. https://doi.org/10.1016/j.ijgo.2008.09.010.
Teran E, Escudero C, Moya W. Abnormal release of nitric oxide from nitrosoprotein in preeclampsia. Int J Gynaecol Obstet. 2006;92(3):260–1. https://doi.org/10.1016/j.ijgo.2005.12.015.
Acauan Filho BJ, Pinheiro da Costa BE, Ogando PB, Vieira MC, Antonello IC, Poli-de-Figueiredo CE. Serum nitrate and NOx levels in preeclampsia are higher than in normal pregnancy. Hypertens Pregnancy. 2016;35(2):226–33. https://doi.org/10.3109/10641955.2016.1139718.
• Serrano NC, Casas JP, Diaz LA, Paez C, Mesa CM, Cifuentes R, et al. Endothelial NO synthase genotype and risk of preeclampsia: a multicenter case-control study. Hypertension. 2004;44(5):702–7. https://doi.org/10.1161/01.HYP.0000143483.66701.ec.
Corthorn J, Germain AA, Chacon C, Rey S, Soto GX, Figueroa CD, et al. Expression of kallikrein, bradykinin b2 receptor, and endothelial nitric oxide synthase in placenta in normal gestation, preeclampsia, and placenta accreta. Endocrine. 2006;29(3):491–9. https://doi.org/10.1385/ENDO:29:3:491.
Smith-Jackson K, Hentschke MR, Poli-de-Figueiredo CE, Pinheiro da Costa BE, Kurlak LO, Broughton Pipkin F, et al. Placental expression of eNOS, iNOS and the major protein components of caveolae in women with pre-eclampsia. Placenta. 2015;36(5):607–10. https://doi.org/10.1016/j.placenta.2015.02.001.
Casanello P, Escudero C, Sobrevia L. Equilibrative nucleoside (ENTs) and cationic amino acid (CATs) transporters: implications in foetal endothelial dysfunction in human pregnancy diseases. Curr Vasc Pharmacol. 2007;5(1):69–84.
Sandrim VC, Palei AC, Metzger IF, Gomes VA, Cavalli RC, Tanus-Santos JE. Nitric oxide formation is inversely related to serum levels of antiangiogenic factors soluble fms-like tyrosine kinase-1 and soluble endogline in preeclampsia. Hypertension. 2008;52(2):402–7. https://doi.org/10.1161/HYPERTENSIONAHA.108.115006.
Gishti O, Jaddoe VW, Felix JF, Klaver CC, Hofman A, Wong TY, et al. Retinal microvasculature and cardiovascular health in childhood. Pediatrics. 2015;135(4):678–85. https://doi.org/10.1542/peds.2014-3341.
de Oliveira CA, de Sa RA, Velarde LG, da Silva FC, doVale FA, Netto HC. Changes in ophthalmic artery Doppler indices in hypertensive disorders during pregnancy. J Ultrasound Med. 2013;32(4):609–16.
Oliveira CA, Sa RA, Velarde LG, Silva FC, Netto HC. PP082. Ophthalmic artery Doppler for identification of severe preeclampsia in pregnancies complicated by hypertension. Pregnancy Hypertens. 2012;2(3):284–5. https://doi.org/10.1016/j.preghy.2012.04.193.
Wenceslau CF, McCarthy CG, Szasz T, Spitler K, Goulopoulou S, Webb RC. Mitochondrial damage-associated molecular patterns and vascular function. Eur Heart J. 2014;35(18):1172–7. https://doi.org/10.1093/eurheartj/ehu047.
Goulopoulou S, Matsumoto T, Bomfim GF, Webb RC. Toll-like receptor 9 activation: a novel mechanism linking placenta-derived mitochondrial DNA and vascular dysfunction in pre-eclampsia. Clin Sci (Lond). 2012;123(7):429–35. https://doi.org/10.1042/CS20120130.
McCarthy CM, Kenny LC. Mitochondrial [dys]function; culprit in pre-eclampsia? Clin Sci (Lond). 2016;130(14):1179–84. https://doi.org/10.1042/CS20160103.
Huppertz B, Kingdom JC. Apoptosis in the trophoblast—role of apoptosis in placental morphogenesis. J Soc Gynecol Investig. 2004;11(6):353–62. https://doi.org/10.1016/j.jsgi.2004.06.002.
McCarthy CM, Kenny LC. Immunostimulatory role of mitochondrial DAMPs: alarming for pre-eclampsia? Am J Reprod Immunol. 2016;76(5):341–7. https://doi.org/10.1111/aji.12526.
Verdegem D, Moens S, Stapor P, Carmeliet P. Endothelial cell metabolism: parallels and divergences with cancer cell metabolism. Cancer Metab. 2014;2:19. https://doi.org/10.1186/2049-3002-2-19.
Afzal-Ahmed I, Mann GE, Shennan AH, Poston L, Naftalin RJ. Preeclampsia inactivates glucose-6-phosphate dehydrogenase and impairs the redox status of erythrocytes and fetal endothelial cells. Free Radic Biol Med. 2007;42(12):1781–90. https://doi.org/10.1016/j.freeradbiomed.2007.02.032.
Wadhwani N, Patil V, Pisal H, Joshi A, Mehendale S, Gupte S, et al. Altered maternal proportions of long chain polyunsaturated fatty acids and their transport leads to disturbed fetal stores in preeclampsia. Prostaglandins Leukot Essent Fatty Acids. 2014;91(1–2):21–30. https://doi.org/10.1016/j.plefa.2014.05.006.
Diaz-Olguin L, Coral-Vazquez RM, Canto-Cetina T, Canizales-Quinteros S, Ramirez Regalado B, Fernandez G, et al. Endothelial nitric oxide synthase haplotypes are associated with preeclampsia in Maya mestizo women. Dis Markers. 2011;31(2):83–9. https://doi.org/10.3233/DMA-2011-0804.
Sandrim VC, Palei AC, Cavalli RC, Araujo FM, Ramos ES, Duarte G, et al. eNOS haplotypes associated with gestational hypertension or preeclampsia. Pharmacogenomics. 2008;9(10):1467–73. https://doi.org/10.2217/14622416.9.10.1467.
Leonardo DP, Albuquerque DM, Lanaro C, Baptista LC, Cecatti JG, Surita FG, et al. Association of nitric oxide synthase and matrix metalloprotease single nucleotide polymorphisms with preeclampsia and its complications. PLoS One. 2015;10(8):e0136693. https://doi.org/10.1371/journal.pone.0136693.
• Julian CG, Pedersen BS, Salmon CS, Yang IV, Gonzales M, Vargas E, et al. Unique DNA methylation patterns in offspring of hypertensive pregnancy. Clin Transl Sci. 2015;8(6):740–5. https://doi.org/10.1111/cts.12346.
Van Noorden R. The impact gap: South America by the numbers. Nature. 2014;510(7504):202–3. https://doi.org/10.1038/510202a.
Fisberg M, Kovalskys I, Gomez G, Rigotti A, Cortes LY, Herrera-Cuenca M, et al. Latin American Study of Nutrition and Health (ELANS): rationale and study design. BMC Public Health. 2016;16:93. https://doi.org/10.1186/s12889-016-2765-y.
Acknowledgements
We would like to thank all research staff from the Red Iberoamericana de alteraciones Vasculares Asociadas a TRastornos del EMbarazo (RIVA-TREM). We appreciate Ms. Lee Rager for her editorial assistance in the preparation of this manuscript.
Funding
Carlos Escudero is financially supported by Fondecyt Regular 1140586, Fondequip EQM140104, DIUBB 166709 3/R, and GI 171709/VC. Carlos Galaviz-Hernandez is financially supported by CONACYT-México FOSISS 162338 and 162368. María P. Ramos is financially supported by SAF2014-56671-R.
Author information
Authors and Affiliations
Consortia
Contributions
This work was carried out as a full collaboration among all the authors. Carlos Escudero defined the research topic. Fernanda Regina Giachini and Victor Vitorino Lima conducted data analysis and epidemiology. Carlos Galaviz-Hernandez and Martha Sosa-Macias contributed with the diagnostic criteria section and drafted the article, as well as elaborated tables and epidemiology section figures. All authors contributed in the discussion and review of the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.x
Additional information
This article is part of the Topical Collection on Preeclampsia
Rights and permissions
About this article
Cite this article
Giachini, F.R., Galaviz-Hernandez, C., Damiano, A.E. et al. Vascular Dysfunction in Mother and Offspring During Preeclampsia: Contributions from Latin-American Countries. Curr Hypertens Rep 19, 83 (2017). https://doi.org/10.1007/s11906-017-0781-7
Published:
DOI: https://doi.org/10.1007/s11906-017-0781-7