Abstract
Purpose of Review
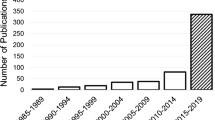
As rates of suicide continue to rise, there is urgent need for innovative approaches to better understand, predict, and care for those at high risk of suicide. Numerous mobile and sensor technology solutions have already been proposed, are in development, or are already available today. This review seeks to assess their clinical evidence and help the reader understand the current state of the field.
Recent Findings
Advances in smartphone sensing, machine learning methods, and mobile apps directed towards reducing suicide offer promising evidence; however, most of these innovative approaches are still nascent. Further replication and validation of preliminary results is needed.
Summary
Whereas numerous promising mobile and sensor technology based solutions for real time understanding, predicting, and caring for those at highest risk of suicide are being studied today, their clinical utility remains largely unproven. However, given both the rapid pace and vast scale of current research efforts, we expect clinicians will soon see useful and impactful digital tools for this space within the next 2 to 5 years.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kessler RC, Hwang I, Hoffmire CA, McCarthy JF, Petukhova MV, Rosellini AJ, Sampson NA, Schneider AL, Bradley PA, Katz IR, Thompson C. Developing a practical suicide risk prediction model for targeting high-risk patients in the Veterans health Administration. Int J Methods Psychiatr Res. 2017;26(3). https://doi.org/10.1002/mpr.1575.
Bernecker SL, Rosellini AJ, Nock MK, Chiu WT, Gutierrez PM, Hwang I, et al. Improving risk prediction accuracy for new soldiers in the US Army by adding self-report survey data to administrative data. BMC Psychiatry. 2018;18(1):87.
Stein MB, Ware EB, Mitchell C, Chen CY, Borja S, Cai T, et al. Genomewide association studies of suicide attempts in US soldiers. Am J Med Genet B Neuropsychiatr Genet. 2017;174(8):786–97.
Larsen ME, Cummins N, Boonstra TW, O’Dea B, Tighe J, Nicholas J, Shand F, Epps J, Christensen H. The use of technology in suicide prevention. Proceedings of the 37th Annual Conference of the Engineering in Medicine and Biology Conference (EMBC). 2015. 7316–7319.
Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187.
Nock MK, Kessler RC, Franklin JC. Risk factors for suicide ideation differ from those for the transition to suicide attempt: the importance of creativity, rigor, and urgency in suicide research. Clin Psychol Sci Pract. 2016;23(1):31–4.
• Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3):S176–80. This paper outlines the need for short-term prediction and clearly outlines future strategies and methods that remain of relevance today.
Robinson J, Cox G, Bailey E, Hetrick S, Rodrigues M, Fisher S, Herrman H. Social media and suicide prevention: a systematic review. Early Interv Psychiatry. 2016;10(2):103-21.
Frison E, Eggermont S. Browsing, posting, and liking on Instagram: the reciprocal relationships between different types of instagram use and adolescents’ depressed mood. Cyberpsychol Behav Soc Netw. 2017;20(10):603–9.
Reece AG, Danforth CM. Instagram photos reveal predictive markers of depression. EPJ Data Sci. 2017;6(1):15.
Shakya HB, Christakis NA. Association of Facebook use with compromised well-being: a longitudinal study. Am J Epidemiol. 2017;185(3):203–11.
Inkster B, Stillwell D, Kosinski M, Jones P. A decade into Facebook: where is psychiatry in the digital age? Lancet Psychiatry. 2016;3(11):1087–90.
Li A, Huang X, Zhu T. A systematic analysis of online broadcasts of suicidality in China. Asia-Pacific Psychiatry. In press. Accepted 12 September 2017. https://doi.org/10.1111/appy.12302
Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32.
Torous J, Staples P, Shanahan M, Lin C, Peck P, Keshavan M, et al. Utilizing a personal smartphone custom app to assess the patient health questionnaire-9 (PHQ-9) depressive symptoms in patients with major depressive disorder. JMIR Mental Health. 2015;2(1):e8.
•• Saeb S, Lattie EG, Schueller SM, Kording KP, Mohr DC. The relationship between mobile phone location sensor data and depressive symptom severity. PeerJ. 2016;4:e2537. This paper features novel smartphone geolocation and mood data that offers a clear example of the feasibility and potential of using smartphone sensors to capture novel real-time data about depression.
Dogan E, Sander C, Wagner X, Hegerl U, Kohls E. Smartphone-based monitoring of objective and subjective data in affective disorders: where are we and where are we going? Systematic review. J Med Internet Res. 2017;19(7):e262.
• Barnett I, Torous J, Staples P, Sandoval L, Keshavan M, Onnela JP. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;22:1. This paper features multimodal smartphone sensor and survey collection and offers links to both the algorithms used to process the data as well as links to the source code for the app used to collect the data
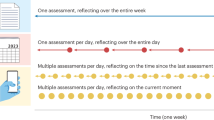
•• Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnorm Psychol. 2017;126(6):726. This paper presents two studies which represent the most fine-grained examination of suicidal ideation to date.
Husky M, Olié E, Guillaume S, Genty C, Swendsen J, Courtet P. Feasibility and validity of ecological momentary assessment in the investigation of suicide risk. Psychiatry Res. 2014;220(1):564–70.
Lyon J. New data on suicide risk among military veterans. JAMA. 2017;318(16):1531.
Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clin Psychol Sci. 2017;5(3):457–69.
Morales S, Barros J, Echávarri O, García F, Osses A, Moya C, et al. Acute mental discomfort associated with suicide behavior in a clinical sample of patients with affective disorders: ascertaining critical variables using artificial intelligence tools. Front Psych. 2017;8:7.
Burnap P, Colombo G, Amery R, Hodorog A, Scourfield J. Multi-class machine classification of suicide-related communication on Twitter. Online Soc Netw Media. 2017;2:32–44.
O'dea B, Larsen ME, Batterham PJ, Calear AL, Christensen H. A linguistic analysis of suiciderelated Twitter posts. Crisis. 2017;38(5):319-329. https://doi.org/10.1027/0227-5910/a000443.
Desjardins I, Cats-Baril W, Maruti S, Freeman K, Althoff R. Suicide risk assessment in hospitals: an expert system-based triage tool. J Clin Psychiatry. 2016;77(7):e874–82.
Depp CA, Thompson WK, Frank E, Swartz HA. Prediction of near-term increases in suicidal ideation in recently depressed patients with bipolar II disorder using intensive longitudinal data. J Affect Disord. 2017;208:363–8.
Thompson WK, Gershon A, O’hara R, Bernert RA, Depp CA. The prediction of study-emergent suicidal ideation in bipolar disorder: a pilot study using ecological momentary assessment data. Bipolar Disord. 2014;16(7):669–77.
Czyz EK, Horwitz AG, Eisenberg D, Kramer A, King CA. Self-reported barriers to professional help seeking among college students at elevated risk for suicide. J Am Coll Heal. 2013;61(7):398–406.
de la Torre I, Castillo G, Arambarri J, López-Coronado M, Franco MA. Mobile apps for suicide prevention: review of virtual stores and literature. JMIR Mhealth Uhealth. 2017;5(10):e130.
Larsen ME, Nicholas J, Christensen H. A systematic assessment of smartphone tools for suicide prevention. PLoS One. 2016;11(4):e0152285.
Torous J, Roberts LW. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437–8.
Berrrouiguet S, Larsen ME, Mesmeur C, Gravey M, Billot R, Walter M, et al. Toward mHealth brief contact interventions in suicide prevention: case series from the Suicide Intervention Assisted by Messages (SIAM) randomized controlled trial. JMIR mHealth uHealth. 2018;6(1):e8.
Luxton DD, Thomas EK, Chipps J, Relova RM, Brown D, McLay R, et al. Caring letters for suicide prevention: implementation of a multi-site randomized clinical trial in the US military and veteran affairs healthcare systems. Contemp Clin Trials. 2014;37(2):252–60.
van Spijker BAJ, van Straten A, Kerkhof AJFM. Effectiveness of online self-help for suicidal thoughts: results of a randomised controlled trial. PLoS One. 2014;9(2):e90118.
van Spijker BAJ, Majo C, Smit F, van Straten A, Kerkhof AJFM. Reducing suicidal ideation: cost-effectiveness analysis of a randomized controlled trial of unguided web-based self-help. J Med Internet Res. 2012;14(5):e141.
van Spijker BAJ, Werner-Seidler A, Batterham PJ, Mackinnon A, Calear AL, Gosling JA, et al. Effectiveness of a web-based self-help program for suicidal thinking in an Australian community sample: randomized controlled trial. J Med Internet Res. 2018;20(2):e15.
Franklin JC, Fox KR, Franklin CR, Kleiman EM, Ribeiro JD, Jaroszewski AC, et al. A brief mobile app reduces nonsuicidal and suicidal self-injury: evidence from three randomized controlled trials. J Consult Clin Psychol. 2016;84(6):544.
McManama O'Brien KH, LeCloux M, Ross A, Gironda C, Wharff EA. A pilot study of the acceptability and usability of a smartphone application intervention for suicidal adolescents and their parents. Arch Suicide Res. 2017;21(2):254–64.
Lee N. Trouble on the radar. Lancet. 2014;384(9958):1917.
Torous JB, Chan SR, Gipson SY, Kim JW, Nguyen TQ, Luo J, et al. A hierarchical framework for evaluation and informed decision making regarding smartphone apps for clinical care. Psychiatr Serv. 2018;69(5):498–500.
Faurholt-Jepsen M, Bauer M, Kessing LV. Smartphone-based objective monitoring in bipolar disorder: status and considerations. Int J Bipolar Disord. 2018;6(1):6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Torous, Colin Depp, Theodore D. Cosco, Ian Barnett, Matthew K. Nock, and Joe Firth declare that they have no conflict of interest.
Mark E. Larsen reports a grant from the National Health and Medical Research Council.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Psychiatry in the Digital Age
Rights and permissions
About this article
Cite this article
Torous, J., Larsen, M.E., Depp, C. et al. Smartphones, Sensors, and Machine Learning to Advance Real-Time Prediction and Interventions for Suicide Prevention: a Review of Current Progress and Next Steps. Curr Psychiatry Rep 20, 51 (2018). https://doi.org/10.1007/s11920-018-0914-y
Published:
DOI: https://doi.org/10.1007/s11920-018-0914-y