Abstract
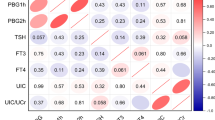
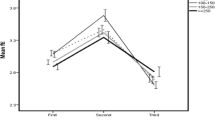
Many studies focused on the association between thyroid disease and pregnancy outcomes. The present study explored the effect of iodine nutrition during the first trimester on pregnancy outcomes. One thousand five hundred sixty-nine pregnant, euthyroid women at ≤12 weeks of gestation in an iodine-sufficient area in China were recruited. According to the World Health Organization (WHO) criteria for iodine nutrition during pregnancy, participants were divided into four groups: adequate iodine (median urinary iodine concentration (UIC), 150–249 μg/L), mild deficiency (UIC, 100–150 μg/L), moderate and severe deficiency (UIC, <100 μg/L), and more than adequate and excessive (UIC, ≥250 μg/L) groups. Pregnancy outcomes, including abortion, gestational hypertension, pre-eclampsia, gestational diabetes mellitus (GDM), placenta previa, placental abruption, preterm labor, low birth weight infants, macrosomia, breech presentation, and cord entanglement, were obtained during follow-up. The results showed that there was no significant difference in general characteristics, including age, body mass index, abdominal circumference, systolic blood pressure, diastolic blood pressure, heart rate, smoking rate, and drinking rate, among the four groups. In the more than adequate and excessive group, thyroid-stimulating hormone (TSH) was greater and free thyroxine (FT4) was lower than any other groups but still within normal range. The thyroglobulin (Tg) level was greater in the moderate and severe deficiency group. The incidence of GDM was significantly greater in women with mild iodine deficiency than in women with adequate iodine nutriture (18.38 vs. 13.70%, p < 0.05). Compared with the adequate group, incidence of macrosomia was significantly greater in the more than adequate and excessive group (12.42 vs. 9.79%, p < 0.05). Mild iodine deficiency was an independent risk factor for GDM (odds ratio = 1.566, 95% confidence interval = 1.060–2.313, p = 0.024); more than adequate and excessive iodine was an independent risk factor for macrosomia (OR = 1.917, CI = 1.128–3.256, p = 0.016). In summary, during 1st trimester, both mild iodine deficiency and excessive iodine intake had adverse impacts on pregnancy outcomes in an iodine-sufficient area.
Similar content being viewed by others
References
Andersson M, de Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the technical consultation. Public Health Nutr 10(12A):1606–1611. doi:10.1017/s1368980007361004
Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J, Zhang S, Gao Z, Zhang X, Fan C, Shan Z, Teng W (2015) Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab 100(4):1630–1638. doi:10.1210/jc.2014-3704
Xie X, Gou W (2013) The eighth edition of obstetrics and gynecology. People’s Medical Publishing House (article in Chinese)
Wolff J, Chaikoff IL (1948) Plasma inorganic iodide as a homeostatic regulator of thyroid function. J Biol Chem 174(2):555–564
Zimmermann MB (2012) The effects of iodine deficiency in pregnancy and infancy. Paediatr Perinat Epidemiol 26(Suppl 1):108–117. doi:10.1111/j.1365-3016.2012.01275.x
Yu J, Luan H, Li Y (2013) Gestational diabetes mellitus status in Shenyang. Chin Pract J Rural Dr(article In Chinese) 21:27–28
Hao B, Shen J, Wan H, Lv M, Li Y, Li J et al (2014) A retrospective survey of the incidence of gestational diabetes mellitus in Guangzhou Tianhe district. Chinese Journal of Diabetes (article in Chinese) 22(7):620–621
Cui Z, Cui X, Xu J (2016) Incidence and clinical data analysis of gestational diabetes mellitus in Qingdao area. Chinese Journal of Woman and Child Health Research (article in Chinese) 27(3):348–351
Yang H, Wei Y, Gao X, Xu X, Fan L, He J, Hu Y, Liu X, Chen X, Yang Z, Zhang C (2009) Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16,286 pregnant women in China. Diabetic Medicine: a Journal of the British Diabetic Association 26(11):1099–1104. doi:10.1111/j.1464-5491.2009.02845.x
Chen G, Wu J, Lin Y, Huang B, Yao J, Jiang Q, Wen J, Lin L (2010) Associations between cardiovascular risk, insulin resistance, beta-cell function and thyroid dysfunction: a cross-sectional study in She ethnic minority group of Fujian Province in China. Eur J Endocrinol 163(5):775–782. doi:10.1530/EJE-10-0710
Al-Attas OS, Al-Daghri NM, Alkharfy KM, Alokail MS, Al-Johani NJ, Abd-Alrahman SH, Yakout SM, Draz HM, Sabico S (2012) Urinary iodine is associated with insulin resistance in subjects with diabetes mellitus type 2. Exp Clin Endocrinol Diabetes 120(10):618–622. doi:10.1055/s-0032-1323816
Kurku H, Gencer A, Pirgon O, Buyukinan M, Aslan N (2016) Increased oxidative stress parameters in children with moderate iodine deficiency. J Pediatr Endocrinol Metab 29(10):1159–1164. doi:10.1515/jpem-2016-0077
Moser M, Buchberger W, Mayer H, Winkler R (1991) Influence of an iodine-drinking cure on the antioxidative status of diabetic patients. Wien Klin Wochenschr 103(6):183–186
Rydbeck F, Rahman A, Grander M, Ekstrom EC, Vahter M, Kippler M (2014) Maternal urinary iodine concentration up to 1.0 mg/L is positively associated with birth weight, length, and head circumference of male offspring. J Nutr 144(9):1438–1444. doi:10.3945/jn.114.193029
Leon G, Murcia M, Rebagliato M, Alvarez-Pedrerol M, Castilla AM, Basterrechea M, Iniguez C, Fernandez-Somoano A, Blarduni E, Foradada CM, Tardon A, Vioque J (2015) Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente cohort. Spain Paediatric and Perinatal Epidemiology 29(2):113–122. doi:10.1111/ppe.12172
Anees M, Anis RA, Yousaf S, Murtaza I, Sultan A, Arslan M, Shahab M (2015) Effect of maternal iodine supplementation on thyroid function and birth outcome in goiter endemic areas. Curr Med Res Opin 31(4):667–674. doi:10.1185/03007995.2015.1011779
Medici M, Korevaar TI, Schalekamp-Timmermans S, Gaillard R, de Rijke YB, Visser WE, Visser W, de Muinck Keizer-Schrama SM, Hofman A, Hooijkaas H, Bongers-Schokking JJ, Tiemeier H, Jaddoe VW, Visser TJ, Peeters RP, Steegers EA (2014) Maternal early-pregnancy thyroid function is associated with subsequent hypertensive disorders of pregnancy: the generation R study. J Clin Endocrinol Metab 99(12):E2591–E2598. doi:10.1210/jc.2014-1505
Mannisto T, Mendola P, Grewal J, Xie Y, Chen Z, Laughon SK (2013) Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J Clin Endocrinol Metab 98(7):2725–2733. doi:10.1210/jc.2012-4233
Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R (2012) Effect of women's nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Paediatr Perinat Epidemiol 26(Suppl 1):285–301. doi:10.1111/j.1365-3016.2012.01281.x
Akturk M, Oruc AS, Danisman N, Erkek S, Buyukkagnici U, Unlu E, Tazebay UH (2013) Na+/I- symporter and type 3 iodothyronine deiodinase gene expression in amniotic membrane and placenta and its relationship to maternal thyroid hormones. Biol Trace Elem Res 154(3):338–344. doi:10.1007/s12011-013-9748-y
Rayman MP (2012) Selenium and human health. Lancet 379(9822):1256–1268
Acknowledgments
We gratefully acknowledged the residents who participated in this study. The study was supported by the National Science and Technology Support Program (grant number 2014BAI06B02); Chinese National Natural Science Foundation (grant numbers 81170730 and 81570709); Research Foundation of Key Laboratory of Endocrine Diseases, Department of Education in Liaoning Province of China (grant number LZ2014035); and Key Platform Foundation of Science and Technology for the Universities in Liaoning Province of China (grant number 16010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiao, Y., Sun, H., Li, C. et al. Effect of Iodine Nutrition on Pregnancy Outcomes in an Iodine-Sufficient Area in China. Biol Trace Elem Res 182, 231–237 (2018). https://doi.org/10.1007/s12011-017-1101-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-017-1101-4