Abstract
Objectives
Central nervous system (CNS) metastases are very common in patients with non-small-cell lung cancer (NSCLC). We aimed to explore the clinical impact of osimertinib, a third-generation epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI), on CNS metastases in patients with advanced NSCLC in real-world setting.
Methods
Patients with advanced NSCLC who received osimertinib after progression of early-generation EGFR-TKIs and CNS metastases on baseline brain scan were retrospectively collected. Primary outcomes were disease control rate (DCR) and progression-free survival (PFS), and secondary objectives were objective response rate (ORR), time to tumor response, median best percentage change from baseline in CNS target lesion (TL) size and safety.
Results
Between Apr 1, 2017, and Dec 30, 2017, 22 patients met selection criteria, 15 with ≥ 1 measurable CNS lesion (RECIST 1.1) were included in CNS evaluable for response (cEFR) set. Among the 22 patients, ORR and DCR were 40.9% and 86.4%, respectively, with median PFS of 8.5 months (95% CI 4.1, 13.0). Median intracranial PFS was not reached. Of 15 patients in cEFR set, CNS DCR was 80.0% with complete response reported in 3 patients (20.0%). Median best percentage change from baseline in CNS TL size was − 40% (range − 100 to + 60%) and median time to CNS tumor response was 1.3 months. CNS ORR was 53.3%. The safety profile was acceptable and no new unexpected findings were found.
Conclusion
This real-world analysis further confirmed that osimertinib indeed demonstrated clinically meaningful efficacy against CNS metastases in Chinese patients with advanced NSCLC.
Similar content being viewed by others
Introduction
Central nervous system (CNS) metastases, such as leptomeningeal metastasis (LM) and brain metastasis (BM), are very common in non-small cell lung cancer (NSCLC) patients and are associated with a significant neurological deficit [1]. CNS metastases accounts for 10–15% at the time of diagnosis and affects 30–50% of NSCLC patients throughout the course of the disease [2]. For advanced NSCLC patients with epidermal growth factor receptor (EGFR) activating mutations, epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs) including gefitinib, erlotinib, and afatinib are now considered to be standard first-line therapy based on evidence from several trials [3,4,5]. Although several researchers have demonstrated a certain activity of first- or second-generation EGFR-TKIs in EGFR-mutated NSCLC patients with CNS metastases [6], it was demonstrated that EGFR + NSCLC patients have a much higher risk of developing CNS metastases [7]. Treatment options for CNS metastases during or after first- or second-generation EGFR-TKIs include surgical resection, stereotactic radiosurgery (SRS), whole-brain radiotherapy (WBRT) and chemotherapy, but with severe adverse effects or limited inability to cross the blood–brain barrier (BBB) [8,9,10,11]. These observations suggest that a drug with much better CNS penetration and acceptable safety profile is needed to effectively treat patients with CNS metastases. Osimertinib is a third-generation EGFR-TKI, which inhibits both EGFR and T790M mutations [12]. It demonstrated greater penetration of the BBB than gefitinib or afatinib in preclinical studies [13], and promising intracranial efficacy in patients with advanced NSCLC from several large-scale randomized control trials [14,15,16]. Among advanced NSCLC patients who have progressed on early-generation EGFR-TKI treatment, the CNS objective response rate (ORR) from those trials range from 50 to 70%, which showed significantly greater efficacy than chemotherapy [17]. However, there was lack of real-world evidence to illustrate the effectiveness and safety of osimertinib on the CNS metastases. Therefore, we retrospectively assessed the real-world clinical impact of osimertinib on CNS metastases in patients with advanced NSCLC in our cancer center.
Materials and methods
Data source and study population
Patients with advanced NSCLC who received osimertinib after progression of early-generation EGFR-TKIs and CNS metastases were retrospectively collected in our cancer center between Apr 1, 2017, and Dec 30, 2017. Eligible patients were required to have histologically or cytologically confirmed NSCLC, stage IV cancer based on the AJCC Cancer Staging Manual (7th Edition) with CNS metastatic lesion on baseline brain CT or MRI scan, treated with osimertinib after progression of early-generation EGFR-TKIs and/or chemotherapy. And only patients with ≥ 1 measurable lesion on baseline brain scan were included in CNS evaluable for response (cEFR) set. A total of 22 patients met selection criteria, and 15 were included in the cEFR set.
Assessments
Primary outcomes were disease control rate (DCR) and progression-free survival (PFS), and secondary objectives were ORR, time to tumor response, median best percentage change from baseline in the sum of CNS target lesion (TL) size and safety. Disease response to treatment and tumor shrinkage was assessed according to Response Evaluation Criteria in Solid Tumor (RECIST) criteria (version 1.1). DCR was defined as the occurrence of complete response (CR), partial response (PR), or stable disease (SD) ≥ 6 weeks, while ORR pointed to CR or PR. PFS was defined as the time interval from the start of the treatment until progressive disease (PD) or death from any other causes, whichever occurs first. Time to tumor response refers to the time from the date of first dose until first response. CNS response evaluation of cEFR set included evaluable metastatic lesions in the brain only, regardless of extracranial response. Adverse events (AEs) were recorded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE, version 4.0).
Statistics analysis
Statistical analyses were carried out by the SPSS 23.0 statistical software (SPSS, Inc., Chicago, IL, USA) and alpha = 0.05 was used as significant level for all statistical testing. The distribution of patients’ baseline demographic/clinical characteristics and treatment patterns were described using frequency analysis. Fisher’s exact test was used to assess the difference of ORR and DCR between various EGFR mutation type subgroups. Kaplan–Meier method was applied to calculate PFS, and log-rank test was used to evaluate the difference between subgroups.
Results
Patients and characteristics
Between Apr 1, 2017, and Dec 30, 2017, 22 patients with advanced NSCLC and CNS metastases on baseline brain scan who received osimertinib from our hospital met the selection criteria, in which 15 were of the cEFR set. All of them were tested for EGFR mutation types before the treatment of osimertinib, 20/22 were T790M positive and received osimertinib after progression of early-generation EGFR-TKIs. The other two patients were demonstrated to have no T790M mutation by plasma ctDNA analysis and cerebrospinal fluid (CSF) analysis, respectively, but received osimertinib after progression of gefitinib and erlotinib based on the presence of EGFR exon21 L858R mutation. All patients received osimertinib 80 mg orally once daily.
The median age of patients for this analysis was 59.5 years (range, 40–82 years), most of them (20/22, 90.9%) were nonsmokers, and 15/22 (68.2%) underwent plasma ctDNA analysis for EGFR mutation detection. As for EGFR genotypes, 11/22 (50.0%) patients were EGFR T790M +/exon19del, 7/22 (31.8%) were T790M +/exon21 L858R, 2/22 (9.1%) were EGFR T790M +/19del negative/L858R negative and 2/22 (9.1%) were T790M negative, other EGFR mutation sites were negative. At the time of osimertinib use, patients’ ECOG PS was 0 (16/22, 72.7%), 1 (4/22, 18.2%), and 2 (2/22, 9.1%). All the patients had received at least one early-generation EGFR-TKIs, among which 9 (40.9%) had gefitinib only, 3 (13.6%) erlotinib only, 4 (18.2%) icotinib only, 3 (13.6%) gefitinib and erlotinib, 1 (4.5%) erlotinib and icotinib, while 2 (9.1%) had avitinib, a third-generation irreversible EGFR-TKI which targets both EGFR and T790M mutation, after progression of first-generation EGFR-TKI gefitinib or icotinib. Nine patients (40.9%) had received previous platinum-containing chemotherapy, and 11 patients (50.0%) had received various EGFR-TKIs only. Patients receiving osimertinib as the second-, third- or > third-line of treatment were 8 (36.4%), 8 (36.4%) and 6 (27.3%), respectively. Six patients (6/22, 27.3%) received brain radiotherapy prior to osimertinib (≤ 6 months: n = 3; > 6 months, n = 3), including three of WBRT and three of SRS. Baseline characteristics of study population are shown in Table 1.
Clinical outcomes
At data cutoff (Mar 1, 2018), the median duration of follow-up was 6.5 months, 17 (77.3%) patients remained on osimertinib treatment, 4 had died and were considered to be related to the disease under investigation, 1 received chemotherapy after osimertinib treatment. These five failures of osimertinib treatment were attributed to intrathoracic progression in three patients, and CNS in two. None discontinued osimertinib before disease progression. The median duration of osimertinib treatment was 5.7 months (range 2.1–12.0 months).
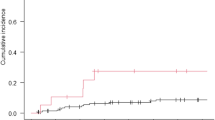
Of the 22 patients, 9 had PR (40.9%), 10 had SD (45.5%) and 3 had PD (13.6%). DCR was 86.4% (19/22; 95% confidence interval [CI] 70.8, 101.9). ORR was 40.9% (9/22; 95% CI 18.6, 63.2) with median time to tumor response: 2.6 months. Events of systemic progression (regardless of intracranially or extracranially) were observed in ten patients (45.5%), and the median PFS was 8.5 months (95% CI 4.1, 13.0) (Fig. 1), while intracranial progression were observed in four patients (18.2%), median intracranial PFS (iPFS) was not reached (95% CI not reached [NC], NC). As for EGFR genotypes, events of systemic progression were lower in T790M +/exon19del group (3/11, 27.3%) than in T790M +/exon21 group (4/7, 57.1%) (p = 0.332). And, events of intracranial progression were observed in 0/11 (0.0%) and 1/7 (14.3%) patients in T790M +/exon19del and T790M +/exon21 population (p = 0.389), respectively. Median PFS of T790M +/exon19del population was not reached, compared to 8.5 months (95% CI 3.2, 13.8) of T790M +/exon21 L858R group. The systemic tumor response to osimertinib is shown in Table 2. Univariate and multivariate analyses using a Cox proportional-hazards model were performed to explore the potential prognostic factors for PFS. Variables (including gender, age, smoking history, ECOG PS scores, treatment line and genotypes) that contributed to significantly longer PFS was not dicovered.
Of the 15 patients in the cEFR set, 8 had CNS CR (3 patients) or PR (5 patients), 4 had SD, and 3 had PD. CNS DCR was 80.0% (12/15; 95% CI 57.1, 102.9), among whom two patients died of intrathoracic progression, but not CNS. The other three patients experienced CNS PD by the time of first CNS assessment, and post-progression therapies were consecutive osimertinib treatment with acceptable stable disease. CNS ORR was 53.3% (8/15; 95% CI 24.7, 81.9) with CR reported in three patients (3/15, 20.0%), regardless of prior radiotherapy to the brain. Of those patients experiencing a CNS response, median time to CNS tumor response was 1.3 months, and none of them subsequently progressed in the CNS. Among patients without prior local treatment to the brain in nearly 6 months, CNS DCR and CNS ORR were 83.3% (10/12) and 66.7% (8/12), respectively. Taking the basis of EGFR mutation status before the initiation of osimertinib into consideration, seven patients were EGFR T790M +/exon19del, five were T790M +/exon21 L858R, two were EGFR T790M +/19del-negative/L858R negative, and one was T790M negative. CNS DCR of T790M +/exon19del group and T790M +/exon21 L858R group were 100.0% (7/7) and 80.0% (4/5), respectively, (p = 0.417), and CNS ORR was 57.1% (4/7) in the T790M/19del group, compared with 60.0% (3/5) in the T790M/L858R group (p = 1.000). There was no statistical difference between the two groups as for CNS DCR and CNS ORR. Of the only patient in cEFR set with no detectable EGFR-T790M mutation but EGFR exon21 L858R, a CNS CR was achieved with osimertinib treatment at the first brain MRI scan. CNS response to osimertinib is shown in Table 3. Tumor shrinkage was seen in most patients (12/15, 80.0%) (Fig. 2). Median baseline CNS TL size was 1.6 cm (range 1.0–4.4), and median best percentage change from baseline in CNS TL size was − 40% (range − 100 to + 60%).
Safety
All patients reported at least one AE. The most common AEs of all grades were stomatitis and increased creatinine (CRE) level. Grade 3 AEs occurred in five patients (22.7%), and no grade 4 AEs were observed. The grade 3 AEs include anorexia (two patients), stomatitis (one patient), fatigue (one patient) and the platelet count decreased (one patient). One patient had a dose interruption due to decrease in the platelet count in grade 3. No one experienced a dose reduction, and none of the patients discontinued or died due to AEs. Table 4 summarizes AEs of any grade and of grade 3 or higher.
Discussion
In this real-world study, 19 of 22 (86.4%) NSCLC patients with CNS metastasis and 12 of 15 (80.0%) CNS response-evaluable patients treated with osimertinib achieved a systemic and intracranial disease control, respectively, and the median PFS was 8.5 months. The study findings confirm the intracranial efficacy evidence and manageable safety profile of osimertinib in the real world.
The ORR and DCR of our study in overall population seemed to be obviously inferior to most large-scale clinical trials including AURA [18], AURA2 [16] and AURA3 [14]. Of the cEFR set, the CNS ORR of our study (53.3%) was similar to that seen in a pooled analysis [17] from two phase II studies: AURA extension and AURA2 (54%), but CNS DCR (80.0%) was lower than this pooled analysis (92%). The lower systemic and CNS ORR/DCR in our study possibly were mainly attributed to the following reasons: 14/22 (63.6%) patients in our study and 11/15 (73.3%) in the cEFR set were treated with osimertinib as ≥ third-line systemic therapy (most of them received chemotherapy as first-line treatment and first-generation EGFR-TKIs in second-line therapy), while osimertinib acted as the second-line treatment in AURA3 [14] trial. In addition, patients with CNS metastases account for about 30–45% of overall population in AURA2 [16] and AURA3 [14], and Asians account for about 60–65% in these clinical trials. Moreover, the rather small sample size of our study may also be attributed to this relatively lower ORR and DCR. Besides a promising response rate in our study, the median time to CNS tumor response in cEFR set with osimertinib is encouraging (1.3 months), which is consistent with the results of clinical trials: 6.1 weeks in AURA3 [14]. And in AURA extension and AURA2 pooled analysis [17], the majority (81%) of patients had responded by the time of first assessment (6 weeks). This rapid onset of response may aid in nursing the neurological symptoms caused by CNS metastases and improving the quality of life.
The median PFS of our study was 8.5 months, which is comparable to 8.5 months of CNS subgroup in AURA3 [14] and longer than chemotherapy (4.2 months). Median CNS PFS was neither reached in our study, nor in the pooled analysis [17] of AURA extension and AURA2. Although these large-scale clinical trials had demonstrated promising survival benefits with osimertinib than chemotherapy or first-generation EGFR-TKIs, mature overall survival is still lacking.
Most of NSCLC patients harboring EGFR activating mutations eventually acquire resistance to the first-generation EGFR-TKIs therapy after varying periods of treatment, and approximately one-third of those patients develop brain metastases [2, 19]. Prior to osimertinib, treatment options for CNS metastases during or after early generation EGFR-TKIs include locoregional therapy with continuation of EGFR-TKI, chemotherapy and combination therapy (combination of chemotherapy and radiotherapy) [20, 21]. However, the accessible limitation for brain lesions of surgical resection [10], the potential long-term cognitive deterioration of WBRT [8, 22], the risk of failure in non-treated brain regions of SRS [9], and the inferior penetration of cytotoxic agents to BBB [23] were gradually be valued. In addition, pulsatile high-dose EGFR-TKI, and the switch from gefitinib to erlotinib were used in an attempt to increase intracranial control based on previous data [24, 25], but the evidence is insufficient.
Several researchers demonstrated heterogenicity between CNS metastases and extracranial lesions [26, 27]. For patients who were re-biopsied after TKI progression, only 17% were T790M positive within CNS metastases, while 41% in systemic lesions [26], suggested that there is lower selection pressure for T790M mutation intracranially, and that current TKIs cannot achieve and maintain efficacious concentrations within the CNS. Thus, a drug with superior BBB penetration is required to achieve optimal intracranial effect. Osimertinib was demonstrated with a higher penetration of BBB than gefitinib, rociletinib, afatinib, and induced sustained tumor regression of brain lesion in the preclinical study [13]. In the FLAURA [28] study, osimertinib demonstrated superior efficacy in advanced EGFR mutation NSCLC, compared with first-generation EGFR-TKI as first-line therapy, including CNS subgroup, which support these preclinical data. As brain radiotherapy was performed in only six patients prior to osimertinib (≤ 6 months: n = 3; > 6 months, n = 3), and median intracranial PFS (iPFS) was not reached in our study, the role of radiotherapy in the patients receiving osimertinib was unclear and needs further researches. We recommended that brain radiotherapy should be used in patients with symptomatic CNS metastases, and be avoided if patients performed asymptomatic, as median time to CNS tumor response in cEFR set with osimertinib was encouraging in our study (1.3 months).
As for EGFR genotypes’ analysis detected before osimertinib treatment, we found that CNS DCR was higher in patients with EGFR T790M + /exon19del mutations than in patients with EGFR T790M + /exon21 L858R mutations, and the events of intracranial progression were lower in T790M + /exon19del group than in T790M + /exon21 L858R population, although the differences in CNS DCR and rates of intracranial progression were not statistically significant. This was consistent with the results of overall population of AURA2 [16] study, and previous studies has reported a superior efficacy of EGFR-TKI in patients with EGFR exon 19del, compared to EGFR L858R mutations [29]. Our study suggests that patients with T790M + /exon21 L858R mutated disease may have less efficacy and more CNS progression than T790M + /exon19del mutation positive disease among osimertinib treatment. However, the conclusion should be taken into careful interpretation because of the small sample size, unbalanced previous treatment and patient characteristics, and we still need further investigations to predict the population that may obtain the maximum benefits from osimertinib.
The advantage of our study is the data are relatively new, which can reflect the current medical practice. Nevertheless, there were several limitations in our study, including its single-center, retrospective design and rather small sample size. It is possible that the lack of an independent review committee (IRC) and evaluation of efficacy of osimertinib by different treating oncologists in our study may have impacted the ORR outcomes, and for this reason, we used DCR and PFS as our primary objectives. Additionally, because of the relatively short follow-up time, median iPFS and overall survival (OS) were not reached. Thus, a long-term follow-up and a multicenter prospective study would be required to further confirm our results.
In conclusion, osimertinib can be an effective treatment option for EGFR-mutated advanced NSCLC patients with CNS metastases in a Chinese population, with tolerable and manageable adverse events.
References
Peters S, Bexelius C, Munk V, Leighl N. The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer. Cancer Treat Rev. 2016;45:139–62.
Heon S, Yeap BY, Britt GJ, Costa DB, Rabin MS, Jackman DM, et al. Development of central nervous system metastases in patients with advanced non-small cell lung cancer and somatic EGFR mutations treated with gefitinib or erlotinib. Clin Cancer Res. 2010;16(23):5873–82.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57.
Sequist LV, Yang JC, Yamamoto N, O’Byrne K, Hirsh V, Mok T, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31(27):3327–34.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46.
Proto C, Imbimbo M, Gallucci R, Brissa A, Signorelli D, Vitali M, et al. Epidermal growth factor receptor tyrosine kinase inhibitors for the treatment of central nervous system metastases from non-small cell lung cancer: the present and the future. Transl Lung Cancer Res. 2016;5(6):563–78.
Hsu F, De Caluwe A, Anderson D, Nichol A, Toriumi T, Ho C. EGFR mutation status on brain metastases from non-small cell lung cancer. Lung Cancer. 2016;96:101–7.
McDuff SG, Taich ZJ, Lawson JD, Sanghvi P, Wong ET, Barker FN, et al. Neurocognitive assessment following whole brain radiation therapy and radiosurgery for patients with cerebral metastases. J Neurol Neurosurg Psychiatry. 2013;84(12):1384–91.
Nieder C, Grosu AL, Gaspar LE. Stereotactic radiosurgery (SRS) for brain metastases: a systematic review. Radiat Oncol. 2014;9:155.
Tsao MN, Rades D, Wirth A, Lo SS, Danielson BL, Gaspar LE, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): an American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol. 2012;2(3):210–25.
Grimm SA. Treatment of brain metastases: chemotherapy. Curr Oncol Rep. 2012;14(1):85–90.
Cross DA, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–61.
Ballard P, Yates JW, Yang Z, Kim DW, Yang JC, Cantarini M, et al. Preclinical comparison of osimertinib with other EGFR-TKIs in EGFR-mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity. Clin Cancer Res. 2016;22(20):5130–40.
Mok TS, Wu Y, Ahn M, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376(7):629–40.
Yang JC, Ahn MJ, Kim DW, Ramalingam SS, Sequist LV, Su WC, et al. Osimertinib in pretreated T790M-positive advanced non-small-cell lung cancer: AURA study phase II extension component. J Clin Oncol. 2017;35(12):1288–96.
Goss G, Tsai CM, Shepherd FA, Bazhenova L, Lee JS, Chang GC, et al. Osimertinib for pretreated EGFR Thr790Met-positive advanced non-small-cell lung cancer (AURA2): a multicentre, open-label, single-arm, phase 2 study. Lancet Oncol. 2016;17(12):1643–52.
Goss G, Tsai CM, Shepherd FA, Ahn MJ, Bazhenova L, Crino L, et al. CNS response to osimertinib in patients with T790M-positive advanced NSCLC: pooled data from two Phase II trials. Ann Oncol. 2018;29(3):687–93.
Janne PA, Yang JC, Kim DW, Planchard D, Ohe Y, Ramalingam SS, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–99.
Park SJ, Kim HT, Lee DH, Kim KP, Kim SW, Suh C, et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer. 2012;77(3):556–60.
Vaca SD, Connolly ID, Ho C, Neal J, Hayden GM. Commentary: treatment considerations for patients with epidermal growth factor receptor-mutated non-small cell lung cancer brain metastases in the era of tyrosine kinase inhibitors. Neurosurgery. 2018;82(1):E6–14.
Yu HA, Sima CS, Huang J, Solomon SB, Rimner A, Paik P, et al. Local therapy with continued EGFR tyrosine kinase inhibitor therapy as a treatment strategy in EGFR-mutant advanced lung cancers that have developed acquired resistance to EGFR tyrosine kinase inhibitors. J Thorac Oncol. 2013;8(3):346–51.
Li J, Bentzen SM, Li J, Renschler M, Mehta MP. Relationship between neurocognitive function and quality of life after whole-brain radiotherapy in patients with brain metastasis. Int J Radiat Oncol Biol Phys. 2008;71(1):64–70.
Zimmermann S, Dziadziuszko R, Peters S. Indications and limitations of chemotherapy and targeted agents in non-small cell lung cancer brain metastases. Cancer Treat Rev. 2014;40(6):716–22.
Katayama T, Shimizu J, Suda K, Onozato R, Fukui T, Ito S, et al. Efficacy of erlotinib for brain and leptomeningeal metastases in patients with lung adenocarcinoma who showed initial good response to gefitinib. J Thorac Oncol. 2009;4(11):1415–9.
Zhu Y, Du Y, Liu H, Ma T, Shen Y, Pan Y. Study of efficacy and safety of pulsatile administration of high-dose gefitinib or erlotinib for advanced non-small cell lung cancer patients with secondary drug resistance: a single center, single arm, phase II clinical trial. Thorac Cancer. 2016;7(6):663–9.
Hata A, Katakami N, Yoshioka H, Takeshita J, Tanaka K, Nanjo S, et al. Rebiopsy of non-small cell lung cancer patients with acquired resistance to epidermal growth factor receptor-tyrosine kinase inhibitor: comparison between T790M mutation-positive and mutation-negative populations. Cancer Am Cancer Soc. 2013;119(24):4325–32.
Sasaki S, Yoshioka Y, Ko R, Katsura Y, Namba Y, Shukuya T, et al. Diagnostic significance of cerebrospinal fluid EGFR mutation analysis for leptomeningeal metastasis in non-small-cell lung cancer patients harboring an active EGFR mutation following gefitinib therapy failure. Respir Investig. 2016;54(1):14–9.
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25.
Jackman DM, Yeap BY, Sequist LV, Lindeman N, Holmes AJ, Joshi VA, et al. Exon 19 deletion mutations of epidermal growth factor receptor are associated with prolonged survival in non-small cell lung cancer patients treated with gefitinib or erlotinib. Clin Cancer Res. 2006;12(13):3908–14.
Acknowledgements
The authors would like to thank all study patients and their family members.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was in accordance with the ethical standards of our institutional review board and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Xing, P., Mu, Y., Hao, X. et al. Data from real world to evaluate the efficacy of osimertinib in non-small cell lung cancer patients with central nervous system metastasis. Clin Transl Oncol 21, 1424–1431 (2019). https://doi.org/10.1007/s12094-019-02071-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02071-5