Abstract
Background
Central lymph node metastasis (LNM) in papillary thyroid carcinoma (PTC) is common. But the association between primary tumor characteristics and specific features of metastatic lymph nodes in PTC has not been fully identified. Determining risk factors for LNM may help surgeons determine rational extent of lymph node dissection.
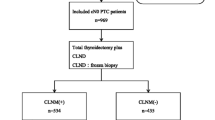
Methods
Data from 432 patients who underwent thyroidectomy with cervical lymph node dissection for PTC were retrospectively analyzed. The relationships between LNM to central compartment or lateral compartment and clinicopathologic factors were analyzed. Cox regression model was used to determine the risk factors for recurrence-free survival (RFS).
Results
Central lymph node metastasis (CLNM) and lateral lymph node metastasis (LLNM) were found in 216 (50.0%) and 65 (15.0%) patients, respectively. In the multivariate analysis for CLNM, patients < 45 years of age (OR 2.037, 95% CI 1.388–2.988, P < 0.001), extrathyroidal invasion (OR: 2.144, 95% CI 0.824–5.457, P = 0.011), vascular invasion (OR 13.817, 95% CI 1.694–112.693, P = 0.014), LLNM (OR 2.851, 95% CI 1.196–6.797, P = 0.014) and TNM Stage III–IV (OR 465.307, 95% CI 113.903–1900.826, P < 0.001) were independent predictors for high prevalence of CLNM. In the multivariate analysis for LLNM, tumor size more than 1cm (OR 3.474, 95% CI 1.728–6.985, P < 0.001) and CLNM (OR 5.532, 95% CI 2.679–11.425, P < 0.001) were independent predictors for high prevalence of LLNM. Moreover, tumor with T3–T4 stage, extrathyroidal invasion and CLNM were the significant factors related to the RFS.
Conclusion
For patients with pre-operative risk factors of LNM, an accurate preoperative evaluation of central compartment or lateral compartment is needed to find suspicious lymph nodes. And prophylactic lymph node dissection should be performed in patients with high risk of CLNM. Moreover, we suggest performing close follow-up for patients with high risk of RFS.




Similar content being viewed by others
References
Lim H, Devesa SS, Sosa JA, et al. rends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017;317(13):1338–48.
Morris LGT, Sikora AG, Tosteson TD, et al. The increasing incidence of thyroid cancer: the influence of access to care. Thyroid. 2013;23(7):885–91.
Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994;97(5):418–28.
Shaha A. Prognostic factors in papillary thyroid carcinoma and implications of large nodal metastasis. Surgery. 2004;135(2):237–9.
Kyu Eun L, Il Yong C, Eunyoung K, et al. Ipsilateral and contralateral central lymph node metastasis in papillary thyroid cancer: patterns and predictive factors of nodal metastasis. Head Neck. 2013;35(5):672–6.
Grogan RH, Kaplan SP, Cao H, et al. A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery. 2013;154(6):1436–47.
Beasley NJ, Lee J, Eski S, et al. Impact of nodal metastases on prognosis in patients with well-differentiated thyroid cancer. Arch Otolaryngol Head Neck Surg. 2002;128(7):825.
Ito Y, Kudo T, Kobayashi K, et al. Prognostic factors for recurrence of papillary thyroid carcinoma in the lymph nodes, lung, and bone: analysis of 5768 patients with average 10-year follow-up. World J Surg. 2012;36(36):1274–8.
Carty SE, Cooper DS, Doherty GM, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009;19(11):1153–8.
Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167–214.
Tuttle RM, Ball DW, Byrd D, et al. Thyroid carcinoma. J Natl Compr Canc Netw. 2010;8(11):1228–744.
Inoue H, Nibu K, Saito M, et al. Quality of life after neck dissection. Arch Otolaryngol Head Neck Surg. 2006;132(132):662–6.
Terrell JE, Welsh DE, Bradford CR, et al. Pain, quality of life, and spinal accessory nerve status after neck dissection. Laryngoscope. 2010;110(4):620–6.
Jr SB, Ferris RL, Goldenberg D, et al. American Thyroid Association consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid. 2012;22(5):501.
Group ATASW, Carty SE, Cooper DS, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid, 2009, 19(11):1153–1158.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol, 2010, 17(6):1471–1474.
Parameswaran R, Sohail A, Ezzat TM, et al. The number of positive lymph nodes in the central compartment has prognostic impact in papillary thyroid cancer. Langenbecks Arch Surg. 2013;398(3):377–82.
Ji JM, Jong Ho Y, Ji Min H, et al. The prognostic value of the metastatic lymph node ratio and maximal metastatic tumor size in pathological N1a papillary thyroid carcinoma. Eur J Endocrinol. 2013;168(2):219–25.
Wang LY, Palmer FL, Nixon IJ, et al. Central lymph node characteristics predictive of outcome in patients with differentiated thyroid cancer. Thyroid. 2014;24(12):1790–5.
Noguchi S, Noguchi A, Murakami N Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer,2015,26(5):1053-1060.
Takami H, Ito Y, Okamoto T, et al. Therapeutic strategy for differentiated thyroid carcinoma in japan based on a newly established guideline managed by Japanese Society of Thyroid Surgeons and Japanese Association of Endocrine Surgeons. World J Surg. 2011;35(1):111–21.
Yuan J, Gang Z, Du J, et al. To identify predictors of central lymph node metastasis in patients with clinically node-negative conventional papillary thyroid carcinoma. Int J Endocrinol. 2016;2016:1–6.
Koo BS, Choi EC, Yoon YH, et al. Predictive factors for ipsilateral or contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma. Ann Surg. 2009;249(5):840–4.
Kim H, Kim J-A, Son EJ, et al. Preoperative prediction of the extrathyroidal extension of papillary thyroid carcinoma with ultrasonography versus MRI: a retrospective cohort study. Int J Surg. 2014;12(5):544–8.
Kim E, Park JS, Son KR, et al. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid. 2008;18(4):411.
Guidoccio F, Grosso M, Orsini F, et al. Thyroid ultrasound and other imaging procedures in the pediatric age. Curr Pediatr Rev. 2016;12(4):253–64.
Nobuyuki W, Quan-Yang D, Kiminori S, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003;237(3):399–407.
Mirallié E, Visset J, Sagan C, et al. Localization of cervical node metastasis of papillary thyroid carcinomaa. World J Surg. 1999;23(9):970–4.
Arora N, Turbendian HK, Scognamiglio T, et al. Extrathyroidal extension is not all equal: implications of macroscopic versus microscopic extent in papillary thyroid carcinoma. Surgery. 2008;144(6):942–8.
Clain JB, Sophie S, Laura DR, et al. Extrathyroidal extension predicts extranodal extension in patients with positive lymph nodes: an important association that may affect clinical management. Thyroid. 2014;24(6):951–7.
Noguchi S, Yamashita H, Uchino S, et al. Papillary microcarcinoma. World J Surg. 2008;32(5):747–53.
Acknowledgements
Bao-Qiang Wu took charge of conceiving and designing the study; Xing-Hai Yang were responsible for collecting the data and analyzing and interpreting the data; Jia-Wei Feng took charge of writing the manuscript; Dong-Lin Sun was responsible for providing critical revisions; approving the final version of the manuscript was in charge of Yong Jiang and Zhen Qu. Lei Qin, the english language editor, was responsible for correcting language and grammar issues.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
This manuscript has not been published nor submitted for publication elsewhere. All authors have contributed significantly, and agree with the content of the manuscript. The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Ethical approval
This study has been approved by the Institutional Review Board of Changzhou First People’s Hospital ethics committee, and has been performed according to the ethical standards laid down in the 1964 Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Feng, JW., Yang, XH., Wu, BQ. et al. Predictive factors for central lymph node and lateral cervical lymph node metastases in papillary thyroid carcinoma. Clin Transl Oncol 21, 1482–1491 (2019). https://doi.org/10.1007/s12094-019-02076-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02076-0