Abstract
Objective
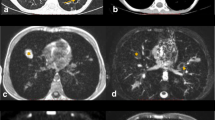
To explore the utility of lung magnetic resonance imaging (MRI) in children with thoracic tuberculosis (TB).
Methods
This prospective study of forty children (age range of 5 to 15 y) with thoracic TB was approved by the institutional ethics committee. Chest radiograph, lung MRI and computed tomography (CT) scan were performed in all children. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) of MRI were calculated and kappa test of agreement was used to determine the strength of agreement between the MRI and CT findings.
Results
MRI performed equivalent to CT scan in detection of mediastinal and hilar lymphadenopathy, pleural effusion and lung cavitation (considered typical for TB) with sensitivity and specificity of 100%. MRI also yielded a sensitivity of 88.2% and specificity of 95.7% for nodules, with sensitivity of 100% and specificity of 92.9% for consolidation. Kappa agreement between CT and MRI in detection of each finding was almost perfect (k: 0.8–1).
Conclusions
Although CT scan is still superior to MRI in detection of smaller nodules, MRI demonstrates a very high degree of correlation and agreement with CT scan for detecting lung and mediastinal pathology related to TB, in children with thoracic TB and can be particularly useful in select population and follow-up of these children to avoid repeated radiation exposures.


Similar content being viewed by others
References
World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. Geneva: WHO; 2006.
World Health Organization. Global tuberculosis report 2012. Geneva: World Health Organization; 2012.
Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis. 2004;8:636–47.
Munoz FM, Starke JR. Childhood tuberculosis. In: Raviglione MC, editor. Reichman and Hershfield’s Tuberculosis. A Comprehensive International Approach. Part A. 3rd ed. New York: Informa Health Care; 2006. p. 307–44.
Rigouts L. Clinical practice: diagnosis of childhood tuberculosis. Eur J Pediatr. 2009;168:1285–90.
Shingadia D, Novelli V. Diagnosis and treatment of tuberculosis in children. Lancet Infect Dis. 2003;3:624–32.
McAdams HP, Samei E, Dobbins J 3rd, Tourassi GD, Ravin CE. Recent advances in chest radiograph. Radiology. 2006;241:863–83.
De Villiers RV, Andronikou S, Van de Westhuizen S. Specificity and sensitivity of chest radiographs in the diagnosis of paediatric pulmonary tuberculosis and the value of additional high-kilovolt radiographs. Australas Radiol. 2004;48:148–53.
Kaguthi G, Nduba V, Nyokabi J, Onchiri F, Gie R, Borgdorff M. Chest radiographs for pediatric TB diagnosis: interrater agreement and utility. Interdiscip Perspect Infect Dis. 2014;2014:291841.
Sharma M, Sandhu MS, Gorsi U, Gupta D, Khandelwal N. Role of digital tomosynthesis and dual energy subtraction digital radiograph in detection of parenchymal lesions in active pulmonary tuberculosis. Eur J Radiol. 2015;84:1820–7.
Kim WS, Moon WK, Kim IO, et al. Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol. 1997;168:1005–9.
Sodhi KS, Lee EY. What all physicians should know about the potential radiation risk that computed tomography poses for paediatric patients. Acta Paediatr. 2014;103:807–11.
Rupprecht T, Böwing B, Kuth R, Deimling M, Rascher W, Wagner M. Steady-state free precession projection MRI as a potential alternative to the conventional chest X-ray in pediatric patients with suspected pneumonia. Eur Radiol. 2002;12:2752–6.
Yikilmaz A, Koc A, Coskun A, Ozturk MK, Mulkern RV, Lee EY. Evaluation of pneumonia in children: comparison of MRI with fast imaging sequences at 1.5T with chest radiographs. Acta Radiol. 2011;52:914–9.
Abolmaali ND, Schmitt J, Krauss S, et al. MR imaging of lung parenchyma at 0.2 T: evaluation of imaging techniques, comparative study with chest radiograph and interobserver analysis. Eur Radiol. 2004;14:703–8.
Sodhi KS, Khandelwal N, Saxena AK, et al. Rapid lung MRI in children with pulmonary infections: time to change our diagnostic algorithms. J Magn Reson Imaging. 2016;43:1196–206.
Sodhi KS, Khandelwal N, Saxena AK, et al. Rapid lung MRI-paradigm shift in evaluation of febrile neutropenia in children with leukemia: a pilot study. Leuk Lymphoma. 2016;57:70–5.
Sodhi KS, Khandelwal N. Magnetic resonance imaging of lungs as a radiation-free technique for lung pathologies in immunodeficient patients. J Clin Immunol. 2016;36:621–3.
Kumar A, Gupta D, Nagaraja SB, Singh V, Sethi GR, Prasad J. Updated national guidelines for pediatric tuberculosis in India, 2012. Indian Pediatr. 2013;50:301–6.
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722.
World Health Organization. Roadmap for childhood tuberculosis: towards zero deaths. Geneva: WHO; 2013.
Rajaram S, Swift AJ, Capener D, et al. Lung morphology assessment with balanced steady-state free precession MR imaging compared with CT. Radiology. 2012;263:569–77.
Montella S, Maglione M, Bruzzese D, et al. Magnetic resonance imaging is an accurate and reliable method to evaluate non-cystic fibrosis paediatric lung disease. Respirology. 2012;17:87–91.
Montella S, Santamaria F, Salvatore M, et al. Assessment of chest high-field magnetic resonance imaging in children and young adults with noncystic fibrosis chronic lung disease: comparison to high-resolution computed tomography and correlation with pulmonary function. Investig Radiol. 2009;44:532–8.
Sileo C, Corvol H, Boelle PY, Blondiaux E, Clement A, Le Pointe HD. HRCT and MRI of the lung in children with cystic fibrosis: comparison of different scoring systems. J Cyst Fibros. 2014;13:198–204.
Montella S, Santamaria F, Salvatore M, et al. Lung disease assessment in primary ciliary dyskinesia: a comparison between chest high-field magnetic resonance imaging and high-resolution computed tomography findings. Ital J Pediatr. 2009;35:24.
Rizzi EB, Schinina V, Cristofaro M, et al. Detection of pulmonary tuberculosis: comparing MR imaging with HRCT. BMC Infect Dis. 2011;11:243.
Johnson J, Kline JA. Intraobserver and interobserver agreement of the interpretation of pediatric chest radiographs. Emerg Radiol. 2010;17:285–90.
Sarria E, Fischer GB, Lima JA, Barreto SS, Flôres JA, Sukiennik R. Interobserver agreement in the radiological diagnosis of lower respiratory tract infections in children. J Pediatr. 2003;79:497–503.
Author information
Authors and Affiliations
Contributions
KSS, MS and JLM: Conception and design of the study and acquisition of the data; KSS, AKS, MS, NK and JLM: Analysis and interpretation of the data; AKS, KSS and MS: Drafted the article; NK and MS: Review and revision. NK will act as guarantor for the paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Sodhi, K.S., Sharma, M., Saxena, A.K. et al. MRI in Thoracic Tuberculosis of Children. Indian J Pediatr 84, 670–676 (2017). https://doi.org/10.1007/s12098-017-2392-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2392-3