Abstract
Objective
To find a correlation between inferior vena cava (IVC) diameters, IVC compressibility index (CI) and central venous pressure (CVP).
Methods
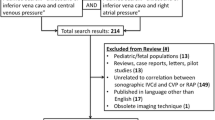
Prospective observational study was done at pediatric intensive care unit (PICU) of Kalawati Saran Children’s Hospital (KSCH). Fifty children aged 5-18 y, presenting with shock were enrolled for the study. IVC diameters, CI and relevant clinical data were noted at enrollment, 30 min, 1 h, 6 h, and 12 h. Central line was placed at the time of admission.
Results
Of 50 children enrolled, 28 were boys, with a mean age of 11 y. More than 80% of cases were diagnosed as septic shock. Mean maximum and minimum IVC diameter of 8.3 ± 2 mm and 3.7 ± 1.7 mm, respectively CI 58.2 ± 7% and CVP of 5.4 ± 1.5 cm of H2O was observed at admission. CVP and IVC diameters showed a serial improvement with treatment; CI showed a serial decrease with treatment. Heart rate (HR) and systolic blood pressure (SBP) also showed a serial improvement at 12 h (p < 0.05). CVP showed a positive correlation with IVC diameter (r +0.312; p < 0.05), and a negative correlation with CI (r −0.343; p < 0.05).
Conclusions
Effective fluid resuscitation improves IVC diameters with a decrease in CI. IVC diameter has a positive correlation to CVP and CI has a negative correlation to CVP.




Similar content being viewed by others
References
Johansson E, Hammarskjöld F, Lundberg D, Arnlind MH. Advantages and disadvantages of peripherally inserted central venous catheters (PICC) compared to other central venous lines: a systematic review of the literature. Acta Oncol. 2013;52:886–92.
Nayeemuddin M, Pherwani AD, Asquith JR. Imaging and management of complications of central venous catheters. Clin Radiol. 2013;68:529–44.
Jevon P, Ewens B. Monitoring the Critically Ill Patient. 3rd ed. Chichester: Wiley-Blackwell; 2012. p. 115–54.
Lyon M, Blaivas M, Brannam L. Sonographic measurement of the inferior vena cava as a marker of blood loss. Am J Emerg Med. 2005;23:45–50.
Pittman JA, Ping JS, Mark JB. Arterial and central venous pressure monitoring. Int Anesthesiol Clin. 2004;42:13–30.
Robinson JF, Robinson WA, Cohn A, Garg K, Armstrong JD. Perforation of great vessels during central venous line placement. Arch Intern Med. 1995;155:1225–8.
Field JM, Bresler MJ. The Textbook of Emergency Cardiovascular Care and CPR. Philadelphia: Lipincott; 2009.
Lyon M, Verma N. Ultrasound guided volume assessment using inferior vena cava diameter. Open Emerg Med J. 2010;3:22–4.
Mauro MA, Murphy K, Thomson K, Venbrux A, Zollikofe CL. Image-Guided Intervention. Philadelphia: Elsevier; 2008.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients. Chest. 2002;121:2000–8.
Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–6.
Sefidbakht S, Assadsangabi R, Abbasi HR, Nabavizadeh A. Sonographic measurement of the inferior vena cava as a predictor of shock in trauma patients. Emerg Radiol. 2007;14:181–5.
Zengin S, Al B, Genc S, et al. Role of inferior vena cava and right ventricular diameter in assessment of volume status: a comparative study: ultrasound and hypovolemia. Am J Emerg Med. 2013;31:763–7.
Nagdev AD, Merchant RC, Tirado-Gonzalez A, Sisson CA, Murphy MC. Emergency department bedside ultrasonographic measurement of the caval index for noninvasive determination of low central venous pressure. Ann Emerg Med. 2009;55:290–5.
Citilcioglu S, Sebe A, Ay MO, Icme F. The relationship between inferior vena cava diameter measured by bedside ultrasonography and central venous pressure value. Pak J Med Sci. 2014;30:310–5.
Acknowledgements
The authors would like to thank Director Professor, Jagdish Chandra, Kalawati Saran Children’s Hospital, New Delhi for his valuable suggestions on the manuscript.
Author information
Authors and Affiliations
Contributions
HV: Acquisition of data, analysis and interpretation of data, drafting of manuscript; VK: Study conception and design, critical revision, final approval of the version to be published; RA: Ultrasonography training, study conception and design, critical revision; VC: Acquisition of data, analysis and interpretation of data; SKK: Critical revision of the manusript. VK will act as guarantor for the paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Appendix
Appendix
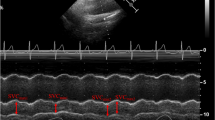
A low-frequency phased array transducer (3.5–5 MHz) of the machine Toshiba Nemio XG SSA-580A was used to evaluate the IVC, which lies in the retroperitoneum, to the right of aorta. IVC was measured at or near the junction with the hepatic veins [4]. To image the IVC, the probe was placed in the subxiphoid 4-chamber position with the probe marker oriented vertically to identify the right ventricle and right atrium. As the probe is progressively aimed toward the spine, the convergence of the IVC with the right atrium was seen. The IVC was then followed inferiorly, specifically looking for the confluence of the hepatic veins with the IVC. M-mode Doppler sonography of the IVC was used to graphically document the absolute size and dynamic changes in the caliber of the vessel during the patient’s respiratory cycle in both inspiration and expiration. After the inferior vena cava was visualized, freeze button was pressed on the Ultrasound console. Using the caliper function on the ultrasound machine, maximum and minimum diameters of the IVC were noted (Fig. 1).
Rights and permissions
About this article
Cite this article
Vaish, H., Kumar, V., Anand, R. et al. The Correlation Between Inferior Vena Cava Diameter Measured by Ultrasonography and Central Venous Pressure. Indian J Pediatr 84, 757–762 (2017). https://doi.org/10.1007/s12098-017-2433-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2433-y