Abstract
Second-line treatment options for patients with relapsed, extensive-stage small cell lung cancer (ES-SCLC) are limited, and even with currently available treatments, prognosis remains poor. Until recently, topotecan (a topoisomerase I inhibitor) was the only drug approved by the United States (US) Food and Drug Administration (FDA) for the management of ES-SCLC following progression after first-line treatment with etoposide plus a platinum derivative (EP; carboplatin preferred). With the most recent approval of EP plus a programmed death ligand 1 (PD-L1) inhibitor, there are now more therapeutic options for managing ES-SCLC. A number of novel agents have emerging data for activity in relapsed ES-SCLC, and single-agent lurbinectedin (an alkylating drug and selective inhibitor of oncogenic transcription and DNA repair machinery in tumor cells) has conditional FDA approval for use in this patient population. Trilaciclib, a short-acting cyclin-dependent kinase 4/6 (CDK 4/6) inhibitor, has also been recently approved as a supportive intervention for use prior to an EP or a topotecan-containing regimen to diminish the incidence of chemotherapy-induced myelosuppression. The current review is based on a recent expert roundtable discussion and summarizes current therapeutic agents and emerging data on newer agents and biomarkers. It also provides evidence-based clinical considerations and a treatment decision tool for oncologists treating patients with relapsed ES-SCLC. This paper discusses the importance of various factors to consider when selecting a second-line treatment option, including prior first-line treatment, available second-line treatment options, tumor platinum sensitivity, and patient characteristics (such as performance status, comorbidities, and patient-expressed and perceived values).
Similar content being viewed by others
Despite recent therapeutic advances, extensive-stage small cell lung cancer (ES-SCLC) remains an extremely aggressive and difficult-to-treat disease. |
The recent approvals of programmed death ligand 1 (PD-L1) immunotherapies for use in combination with etoposide plus a platinum derivative (EP) chemotherapy have introduced a new first-line standard of care for patients with ES-SCLC. |
On the basis of currently available data in the immunotherapy era, the best second-line therapy after combination of chemo-immunotherapy is not well defined, as many second-line therapies have been studied only after the use of EP. Lurbinectedin and topotecan are reasonable second-line treatment options for relapsed ES-SCLC; however, second-line treatment options for patients with relapsed ES-SCLC are limited and include the reintroduction of EP (with or without immunotherapy). |
Supportive care remains an integral part of the treatment course for ES-SCLC. |
It is important to have a shared-decision process with the patient, including a discussion of the risks and benefits of available treatment options, clinical trials, and hospice. |
Introduction
Lung cancer remains the leading cause of cancer-related deaths in the USA, accounting for approximately one-quarter of estimated cancer-related deaths in 2020, which is more than the total number of deaths resulting from breast, prostate, and colorectal cancers [1]. Small cell lung cancer (SCLC) comprises approximately 13–15% of all lung cancers, with 30,000–35,000 new cases diagnosed in the USA per year [2,3,4]. SCLC is a poorly differentiated neuroendocrine tumor that is strongly associated with smoking and is characterized by its aggressive nature, with a rapid doubling time, high growth fraction, and early development of metastases [4,5,6]. The most common sites of metastasis include the brain, liver, and bone [6].
SCLC has known pathologic, clinical, and molecular characteristics [7]. Prognosis remains poor, and without active treatment, median survival is 2–4 months; even with treatment, less than 5% of patients survive for 5 years [8]. At the time of diagnosis, up to 70% of patients with SCLC have extensive-stage (ES) disease, which has a worse prognosis compared with limited-stage (LS) disease [6, 9]. However, even in LS-SCLC, median overall survival (OS) is less than 2 years due to the high risk of disease recurrence and progression, with only 15% of patients experiencing long-term survival. Almost all patients with ES-SCLC who respond to first-line systemic treatment will eventually develop disease progression [6, 9].
A major challenge in the management of recurrent disease is the lack of effective treatment options to induce durable disease control. Despite few therapeutic successes in SCLC over the last 3 decades, increased research interest and the recent approval of new drugs are translating into changes in clinical practice and an improvement in outcomes for patients with ES-SCLC. Furthermore, a better understanding of the pathologic and molecular characteristics of SCLC may lead to the identification of biomarkers that will aid in drug development and/or better match patients’ tumor subtypes with available treatment options.
The objectives of this review are to evaluate second-line treatment options for patients with relapsed ES-SCLC, including discussions of how greater use of immunotherapies as first-line therapy may affect patient outcomes and the choice of second-line strategies; to develop a practical decision tool for the management of relapsed ES-SCLC based on patient characteristics and real-world experience; and to put into clinical context novel biomarkers and their potential association with experimental therapies and implications for the future outlook of ES-SCLC treatment.
Methods
A literature search of the PubMed database was conducted for English language articles (research articles, systematic reviews, and meta-analyses) published between January 1, 1998 and December 15, 2020. Search categories and terms included disease: “extensive-stage,” “small cell lung cancer (SCLC),” “relapsed disease”; immunotherapy: “atezolizumab,” “CASPIAN,” “checkpoint inhibitors,” “durvalumab,” “immunotherapy,” “Impower133,” “ipilimumab,” “nivolumab,” “pembrolizumab,” “RRx-001”; chemotherapy: “etoposide,” “etoposide-platinum,” “platinum,” “irinotecan,” “lurbinectedin,” “temozolomide,” “topotecan”; targeted therapy: “cyclin-dependent kinase 4/6 (CDK 4/6),” “delta-like ligand 3 (DLL-3),” “PARP,” “trilaciclib”; biomarkers: “biomarkers,” “Schlafen 11 (SLEN11)”; other: “current,” “epidemiology,” “guidelines,” “real-world,” “second-line treatment,” “treatments.”
The results of this literature search were reviewed by the authors, who are researchers and clinicians experienced in the treatment of SCLC, and the evidence was discussed and consensus points developed during two virtual meetings. The proceedings from these meetings, supplemented by published literature and the clinical experience of the authors, are presented in this review.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Current Standard of Care: ES-SCLC
Patients with SCLC often have a variety of comorbidities associated with tobacco smoking, such as chronic obstructive pulmonary disease and cardiovascular disease, and these can be associated with poor performance status [10]. Negative prognostic factors for OS identified in patients with SCLC include history of smoking, poor performance status, male sex, and older age (≥ 70 years), along with social factors, such as being unmarried and low socioeconomic status [11, 12]. At the time of diagnosis, the majority of patients with SCLC present with extensive-stage disease [7].
First-Line Treatment Options
First-line treatment of ES-SCLC with etoposide plus a platinum derivative (EP) chemotherapy has been a standard therapy for more than 30 years, with a general preference for carboplatin over cisplatin owing to a more tolerable toxicity profile and comparable efficacy [6, 13]. However, despite high initial response rates to first-line EP therapy in patients with ES-SCLC, relapse rates are high and overall prognosis of relapsed disease is poor—most likely because of rapid development of drug resistance [14]. In response to this challenge, a number of trials have explored the use of alkylating agents (e.g., ifosfamide), anthracyclines (e.g., epirubicin, amrubicin), antifolates (e.g., pemetrexed), camptothecins (e.g., irinotecan, topotecan), or taxanes (e.g., paclitaxel) in combination with platinum drugs as first-line treatment for ES-SCLC (Table 1) [14,15,16,17,18]. However, none of these regimens have proven superiority over EP, which had remained the standard-of-care frontline treatment regimen until the advent of programmed death ligand 1 (PD-L1) immune-checkpoint therapy [6, 14].
New First-Line Immunotherapy Treatment Options
More recently, improved OS was demonstrated in randomized phase 3 clinical trials of PD-L1 immunotherapies combined with EP regimens as first-line treatment for ES-SCLC [19, 20]. This development represents a paradigm shift and the most significant move forward in this setting in the last 3 decades [6, 21,22,23].
Durvalumab is a PD-L1 immunotherapy that was evaluated in the randomized, controlled, open-label, phase 3 CASPIAN trial that compared durvalumab (with or without tremelimumab, a cytotoxic T-lymphocyte-associated antigen 4 [CTLA-4] inhibitor) in combination with EP (with either cisplatin or carboplatin) versus EP alone in treatment-naïve patients with ES-SCLC and a World Health Organization (WHO) performance status of 0 or 1 [20]. Patients were randomly assigned to durvalumab plus EP, durvalumab plus tremelimumab plus EP, or EP alone. Treatment consisted of up to four cycles of durvalumab plus EP with or without tremelimumab every 3 weeks followed by maintenance treatment with durvalumab (with or without tremilimumab) every 4 weeks in the immunotherapy groups and up to six cycles of EP every 3 weeks in the EP-alone group. Durvalumab (without tremelimumab) plus EP significantly reduced the risk of death at the planned interim analysis (18 months) by 27% compared with EP alone (hazard ratio [HR] 0.73 [95% confidence interval (CI) 0.59, 0.91]; P = 0.0047) [20].
Updated results after a median follow-up of 25.1 month (IQR 22.3–27.9) showed that durvalumab (without tremelimumab) plus EP produced a sustained improvement in OS versus EP alone (HR 0.75 [95% CI 0.62, 0.91]; nominal P = 0.0032); median OS was 12.9 months (95% CI 11.3, 14.7) versus 10.5 months (95% CI 9.3, 11.2) [24]. Importantly, the addition of tremelimumab to durvalumab plus EP did not improve OS compared with EP alone, suggesting that the combination immunotherapeutic approach has no added benefit in this setting [24]. The lack of benefit with CTLA-4 inhibition was also shown with ipilimumab in combination with EP, which failed to prolong OS compared with EP alone in patients with newly diagnosed ES-SCLC [25].
Atezolizumab, another PD-L1 monoclonal antibody, has also demonstrated effectiveness when used in combination with EP as first-line treatment for ES-SCLC [19]. In the IMpower133 double-blind, placebo-controlled, phase 3 trial, treatment-naïve patients with ES-SCLC and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 were randomized to receive EP (with carboplatin) with either atezolizumab or placebo for four 21-day cycles (induction phase) followed by a maintenance phase during which they received either atezolizumab or placebo [19]. Both primary endpoints of OS and investigator-assessed progression-free survival (PFS) were significantly improved when atezolizumab was added to EP as first-line therapy in patients with ES-SCLC compared with EP alone [19]. A follow-up analysis showed that atezolizumab plus EP had a comparable safety profile to placebo plus EP and did not have a negative impact on health-related quality of life [26]. In an updated OS analysis with a median follow-up of 22.9 months, median OS was 12.3 months (95% CI 10.8, 15.8) with atezolizumab plus EP versus 10.3 months (95% CI 9.3, 11.3) with placebo plus EP (HR 0.76 [95% CI 0.60, 0.95]; descriptive P = 0.0154) in patients with ES-SCLC [27]. At 18 months, 34% and 21% of patients were alive in the atezolizumab plus EP and placebo plus EP groups, respectively [27].
It is worth noting that in both the CASPIAN and IMpower133 trials, the Kaplan–Meier curves for OS and PFS did not diverge until about 6 months, suggesting that only a subset of patients benefited from the addition of immunotherapy to EP and that the impact was somewhat delayed even in patients who derived benefit [19, 20]. There are differences in the inclusion criteria regarding brain metastases between the studies, which is worth highlighting since patients with asymptomatic and untreated brain metastases were allowed in CASPIAN whereas they were excluded from IMpower133 [19, 20]. Currently, no biomarkers exist to differentiate between patient subsets who may benefit from the addition of a PD-L1 inhibitor to standard EP chemotherapy and those who may not. Notably, patients derived similar benefit from the addition of atezolizumab to EP in IMpower133 independent of PD-L1 immunohistochemistry or blood-based tumor mutational burden (bTMB) status [27]; however, the bTMB biomarker needs further refinement and validation as there are variable gene panel sizes, algorithms, and cutoffs that may vary on the basis of the tumor type such that a bTMB cutoff of 16 mutations per megabase may be sufficiently high for non-small cell lung cancer (NSCLC) but not for SCLC [28, 29].
In a meta-analysis of four immune-checkpoint-inhibitor trials, including two with PD-L1 inhibitors that are currently approved by the FDA for the first-line treatment of patients with ES-SCLC (CASPIAN [durvalumab] and IMpower133 [atezolizumab]) and two with programmed death 1 (PD-1) inhibitors that are not currently approved by the FDA (KEYNOTE-604 [pembrolizumab] and ECOG-ACRIN EA5161 [nivolumab]), a pooled analysis of all four of these trials showed that frontline immune-checkpoint inhibitors provide significant survival benefits when combined with EP chemotherapy in patients with ES-SCLC [30]. Further, in the pooled analysis of all four trials, the addition of a PD-1/PD-L1 inhibitor to EP chemotherapy led to a significant benefit in OS (HR 0.76 [95% CI 0.68, 0.85]; P < 0.00001), PFS (HR 0.75 [95% CI 0.68, 0.84]; P < 0.00001), and objective response rate (ORR; odds ratio 1.28 [95% CI 1.04, 1.57]; P = 0.02) compared with EP chemotherapy alone [30]. Despite the promising results noted in the phase III KEYNOTE-604 trial, it should be noted that the P value did not meet the required significance threshold in the planned hierarchical OS analysis, and pembrolizumab is not currently FDA approved as a frontline option in patients with ES-SCLC [30, 31].
In summary, on the basis of the results from the CASPIAN and IMpower133 trials, the FDA approved either durvalumab or atezolizumab in combination with EP as first-line treatment of patients with ES-SCLC [32, 33], introducing a treatment paradigm shift in frontline therapy. However, even with these advances, almost all patients with ES-SCLC who respond to first-line systemic treatment will eventually develop progressive disease and require second-line therapy, with very few patients achieving long-term response to maintenance PD-L1 therapy [6, 13]. For these patients with disease progression, therapeutic options are limited, long-term survival is often less than 10 months [13, 34], and the general goal of systemic therapy is to palliate symptoms and prolong quality of life [6].
Second-Line Treatment Options
Two time-based criteria (i.e., 90 days or 180 days) are most commonly used to characterize relapsed ES-SCLC according to the duration of treatment-free interval since the last platinum dose given as part of frontline treatment. Thus, a tumor with durable tumor response lasting longer than 90 days from the last dose of frontline platinum doublet is termed “platinum sensitive,” while recurrence within 90 days of chemotherapy is termed “platinum resistant.” A “refractory” case is one in which the patient’s tumors either never responded or progressed within 45 days of treatment [4]. These are not definitive cutoffs as other studies have used various thresholds (e.g., 60 days) for classifying a relapsed SCLC as chemotherapy sensitive [35]. In general, a prolonged treatment-free interval beyond 6 months typically leads to the consideration of platinum-doublet re-treatment at the time of relapse.
Prognosis for patients who relapse or progress after first-line chemotherapy is poor: a median survival of 2–3 months was observed in patients who did not receive second-line therapy and typically 6 months or less in those who did receive second-line therapy [36]. Hence, second- or third-line treatment for ES-SCLC is primarily considered palliative, with a focus on maintaining or improving quality of life to the extent possible. Treatment options, and the likelihood of their success, may vary depending on whether the initial tumor response was considered platinum sensitive, resistant, or refractory [36]. A systematic analysis of second-line chemotherapy efficacy in sensitive and refractory SCLC determined that patients with SCLC whose tumors were platinum-sensitive (> 90 days’ relapse-free interval after first-line therapy) derived greater benefit compared with those whose tumors were platinum-resistant (< 90 days’ relapse-free interval after first-line therapy) [37].
Because of first-line use of immunotherapy (durvalumab or atezolizumab) plus EP, the treatment landscape for second-line therapy is rapidly evolving, albeit with limited long-term data. Most of what is currently known about second-line therapy outcomes involves patients treated only with first-line EP chemotherapy without a PD-L1 inhibitor. Moreover, whether it is beneficial to continue immunotherapy into the second-line setting for patients progressing while on maintenance immunotherapy administered as part of frontline treatment remains to be determined.
Topotecan
Since its initial approval in 1996 and until recently, topotecan has been the only FDA-approved agent as a second-line treatment option for patients with SCLC and is only approved for those with chemotherapy-sensitive, relapsed SCLC [38, 39]. Topotecan is a topoisomerase I inhibitor with cytotoxic effects [38] that has demonstrated efficacy in several second-line therapy trials of patients with relapsed SCLC, with ORRs ranging from 8% to 27% and a median OS ranging from 3.7 to 12.5 months, although the efficacy reported is largely limited to chemotherapy-sensitive disease (Table 2) [35, 40,41,42,43,44,45,46,47,48]. Topoisomerase I expression, as evaluated by immunohistochemistry, has been shown to be highly prevalent in patients with SCLC and has been shown to be associated with increased disease control in patients with platinum-sensitive, relapsed SCLC who received topotecan as second-line therapy [49]. Topotecan is available for injection or oral administration [38, 39], with similar efficacy and tolerability between the two formulations (Table 2) [44].
In patients with platinum-sensitive, platinum-resistant, or platinum-refractory relapsed SCLC, the main adverse event with topotecan infusions is myelosuppression [40, 41, 44,45,46,47]. The standard intravenous (IV) dosing of topotecan is 1.5 mg/m2 daily on days 1–5 of a 21-day cycle [39]. A less burdensome schedule of a higher weekly dose of topotecan (6 mg/m2 IV for 6 weeks) in 38 patients with relapsed SCLC yielded no responses in those with refractory tumors and three responses (all partial, none complete) in those with sensitive tumors, which was offset by even higher levels of hematologic toxicity [45]. Irinotecan, another topoisomerase I inhibitor, is sometimes used as an alternative to topotecan in the second-line setting owing to its less frequent dosing (i.e., weekly) and lower probability of myelosuppressive adverse events [50].
Re-treatment with Platinum Chemotherapy for Platinum-Sensitive Relapse
Until recently, in both the USA and Europe, topotecan has been the go-to second-line therapy for patients with platinum-sensitive, relapsed SCLC. However, in platinum-sensitive patients (relapse ≥ 90 days) with ECOG performance status 0–2, a recent study has shown platinum-based chemotherapy rechallenge to be superior to topotecan. This multicenter, open-label, randomized, phase 3 trial conducted in Japan (JCOG0605) compared topotecan alone with combination chemotherapy consisting of EP (with cisplatin) plus irinotecan [47]. OS was significantly longer in the combined chemotherapy arm versus the topotecan arm (median 18.2 months vs 12.5 months; HR 0.67 [90% CI 0.51, 0.88]; P = 0.0079), as was PFS (median 5.7 months vs 3.6 months; HR 0.50 [95% CI 0.37, 0.68]; P < 0.0001). However, grade 3 or 4 febrile neutropenia, thrombocytopenia, and anemia were more common in the combination chemotherapy arm [47]. Given the unfavorable toxicity profile of this triplet regimen, it is unlikely to be widely adopted.
Similar results were shown for PFS in a randomized, open-label, phase 3 French study that compared orally administered topotecan with EP in patients with platinum-sensitive, relapsed SCLC [48]. Although median PFS was significantly longer in the combination EP chemotherapy arm compared with the topotecan arm (4.7 months [90% CI 3.9, 5.5] vs 2.7 months [90% CI 2.3, 3.2; HR 0.57 [90% CI 0.41, 0.73]; P = 0.0041), there were no significant differences between the treatment arms for median OS. Unlike the JCOG0605 triplet regimen, there were no major differences between the platinum-doublet chemotherapy and topotecan treatment arms with respect to percentages of grade 3 or 4 neutropenia, thrombocytopenia, anemia, or febrile neutropenia in this study [48]. Given the importance of platinum-based chemotherapy in SCLC—including platinum-sensitive, relapsed disease—there are agents being developed to induce or re-induce platinum sensitivity [51].
Lurbinectedin
Lurbinectedin is an alkylating drug and selective inhibitor of oncogenic transcription and DNA repair machinery in tumor cells, triggering tumor cell apoptosis and altering the inflammatory tumor microenvironment [52,53,54]. Lurbinectedin received an orphan drug designation in 2018 [55], and on the basis of the results of a phase 2 basket trial, received an accelerated approval in June 2020 as a second-line treatment option in patients with ES-SCLC who develop disease progression on or after platinum-based chemotherapy [52, 56].
The phase 2 basket trial was a single-arm, open-label study of lurbinectedin 3.2 mg/m2 every 21 days as second-line treatment for patients with relapsed SCLC and documented progression after treatment with only one prior chemotherapy (prior immunotherapy was allowed but only 8% of patients received prior immunotherapy) [57]. All patients in the study had an ECOG performance status of 2 or better. At data cutoff, with a median follow-up of 17.1 months, responses were observed in 37 of 105 study participants, for an ORR of 35.2% (95% CI 26.2, 45.2) (Table 3) [57]. The ORR was higher for patients with platinum-sensitive tumors (45.0%) compared with those with platinum-resistant tumors (22.2%). Moreover, 43% of all patients with a response had a durable response of 6 months or longer. The median OS was 11.9 months for patients with platinum-sensitive tumors versus 5.0 months for those with platinum-resistant tumors, and the median OS of the entire cohort was 9.3 months [57]. The most common grade 3 or 4 adverse events were neutropenia (46%), leukopenia (29%), abnormal γ-glutamyl transferase (15%), anemia (9%), fatigue (7%), and thrombocytopenia (7%) [57].
The phase 3 ATLANTIS open-label, randomized, multicenter trial examined lurbinectedin in patients with ES-SCLC but did not include an investigational treatment arm of lurbinectedin alone. The trial treatment arms compared the combination of lurbinectedin plus doxorubicin with standard of care (investigator’s choice of topotecan or cyclophosphamide/doxorubicin/vincristine [CAV]) in 613 patients with SCLC, disease progression after one prior platinum-containing chemotherapy regimen, and a chemotherapy-free interval of 30 days or more [58, 59]. In December 2020, a press release reported that the trial did not meet the primary endpoint of OS for significance in the intent-to-treat patient population. The safety and tolerability data of ATLANTIS were consistent with the known safety profile of lurbinectedin, and there were no new safety signals in the lurbinectedin treatment arm [59]. The ATLANTIS trial has not yet been published since the press release, and without the full study outcomes, a full understanding of the implications of the results is not possible. On the basis of the limited information currently available, it is hypothesized that the lower lurbinectedin dose used in the phase 3 trial (2.0 mg/m2 every 21 days) compared with the phase 2 trial (3.2 mg/m2 every 21 days) may have affected the outcomes [57,58,59]. This hypothesis is in line with an exposure–response analysis of lurbinectedin dosage in SCLC that determined the 3.2 mg/m2 dose every 21 days (same dose as used in the phase 2 trial and FDA approved) provided the most benefit in patients with SCLC who had disease progression on or after platinum-based chemotherapy and had a manageable risk of grade 4 neutropenia [60]. Given that the single-arm, open-label, phase 2 study in 105 patients resulted in conditional accelerated approval of lurbinectedin by the FDA on the basis of ORR and duration of response, “continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials” [61].
There was also preliminary data from the phase 1b/2 study of lurbinectedin in combination with irinotecan among 21 patients with SCLC with disease progression after no more than two prior therapies which reported an ORR of 62% and a median PFS of 6.2 months (95% CI 4.3, 8.5) [62, 63], suggesting that additional combination studies may be warranted. Given the limited treatment options in the second-line setting and the lethality of previously treated ES-SCLC, in spite of the phase 3 lurbinectedin plus doxorubicin combination failing to meet the primary endpoint with the caveats mentioned above, lurbinectedin monotherapy offers preliminary efficacy with a favorable safety profile, a facile dosing schedule, and is a reasonable second-line treatment option for patients with relapsed SCLC.
Immunotherapies
SCLC has long been considered an immunogenic disease because of high tumor mutational burden secondary to tobacco exposure related to tumor development and the occurrence of paraneoplastic disorders in 15–20% of newly diagnosed cases, providing a rational basis for consideration of immunotherapies in the treatment of SCLC [64,65,66]. As previously discussed, the immune-checkpoint inhibitors durvalumab and atezolizumab have an established efficacy as part of frontline therapy for ES-SCLC in combination with EP [19, 20]. Although pembrolizumab and nivolumab, both PD-1 monoclonal antibodies, had received accelerated FDA approval for patients with relapsed SCLC who had received two prior lines of treatment (including platinum-based chemotherapy), both applications have been recently withdrawn [67,68,69]. Pembrolizumab initially received accelerated approval based on the pooled data from two basket trials (KEYNOTE-028 and KEYNOTE-158) [68, 70, 71]. In a pooled analysis of SCLC cohorts (N = 83) from KEYNOTE-028 (enrolled patients with PD-L1-positive tumors) and KEYNOTE-158 (enrolled patients irrespective of PD-L1 status of tumors), the ORR was 19.3% (95% CI 11.4, 29.4) [68]. The confirmatory phase 3 KEYNOTE-604 trial, however, did not reach statistical significance for the primary endpoint of OS, leading to voluntary withdrawal by the manufacturer of the US SCLC indication for pembrolizumab in March 2021 [31, 72].
Nivolumab was initially studied alone or in combination with ipilimumab in patients with relapsed ES-SCLC in the Checkmate-032 phase 1/2 trial. Although the study treatments were not initially designed to be compared with one another, the ORRs of nivolumab monotherapy versus nivolumab plus ipilimumab in patients with relapsed SCLC were 11.6% and 21.9%, respectively. Median OS was 5.7 months with nivolumab monotherapy versus 4.7 months with nivolumab plus ipilimumab combination therapy. Not surprisingly, combining ipilimumab with nivolumab increased grade 3–4 toxicity from 12.9% with nivolumab monotherapy to 37.5% with nivolumab plus ipilimumab [73]. In the confirmatory phase III trial comparing nivolumab with chemotherapy (topotecan or amrubicin) in patients with relapsed SCLC, Checkmate 331, the primary endpoint of superior OS was not met [74, 75]. In addition, examination of immunotherapy maintenance strategies after first-line chemotherapy of nivolumab plus ipilimumab or nivolumab monotherapy in patients with ES-SCLC in the randomized, phase III Checkmate 451 study did not result in a prolongation of OS versus placebo [74]. On the basis of these results, the nivolumab indication for relapsed ES-SCLC was withdrawn in January 2021 from the USA by its manufacturer [69].
Since no immune-checkpoint inhibitors are FDA approved in relapsed SCLC and the current use of PD-L1 inhibitors is in the frontline setting in combination with EP and as continuation maintenance therapy, there is very limited use for immunotherapies in the standard-of-care second-line setting despite some preliminary efficacy results.
Management Considerations
A number of factors, including available treatments, efficacy and safety profiles, prior treatment history, disease characteristics (chemotherapy-sensitive or chemotherapy-resistant disease), and patient characteristics (performance status, comorbidities, and values) need to be taken into account when considering treatment recommendations for patients with relapsed SCLC. A balance between the benefits and risks of therapy versus those associated with untreated disease is often dependent on a joint decision between the physician and the patient. Patients with SCLC commonly present with shortness of breath or chest pain that often rapidly improve following initial chemotherapy administration. However, the probability of controlling SCLC with available systemic treatments decreases in the relapsed setting, particularly in those patients with platinum-resistant disease. Hence, quality of life is frequently an important goal of care along with the expectation of increased duration of life. These perceived conflicting value propositions sometimes still lead to aggressive therapy when the suffering from the cancer exceeds the suffering expected with side effects of treatment.
Performance Status
Poor performance status (3–4) is commonly recognized as a negative prognostic factor for outcome in patients with ES-SCLC [6, 11] and is a consideration when choosing a second-line treatment option in this patient population [76]. Patients with poor performance status may be unable to undergo a chemotherapy regimen because of its toxicity [77], especially when the probability of response, and therefore improvement in performance status, is also lower in the second-line setting compared with the first-line setting for patients with ES-SCLC [6, 65, 66, 77]. Most of the clinical trials evaluating treatments in this setting restrict patient enrollment to those with a performance status of 2 or better.
Patient Values
The importance of patient values in the decision to continue with a second-line treatment plan for relapsed ES-SCLC is critical and is recognized by many institutions and reflected in their treatment protocols. For example, ethicists at Emory University in the USA developed a “patient value tool” called Patient Preference Assessment Tool (PPAT) based on a small study of phase I clinical trial participants that ranked what was most important to patients, which included “spend more time with family,” “travel concerns,” “avoidance of side effects,” “living longer,” and may differ from what the physician considers most important [78, 79]. Therefore, consideration of the most important factors to the patient is as critical as the information about the pros and cons associated with various therapies in the shared-decision plan. Some patients may choose hospice care as their preferred option, wishing to avoid hospitalization at all costs, especially when family members may be restricted from visiting (as has been experienced during the coronavirus disease 2019 [COVID-19] pandemic), while others may choose an experimental therapy on a clinical trial.
A Treatment Decision Tree
Several clinical practice guidelines are available for consultation when deciding management strategies for patients with ES-SCLC in the second-line setting [80,81,82,83,84]. Clinical practice frequently varies from guideline recommendations, reflecting regional, institutional, and patient factors, as well as because of convenience and cost considerations [9, 76, 80]. This review incorporates the most current evidence and the clinical experience of the authors to provide practical guidance.
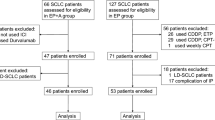
The roundtable panel’s recommendations (Fig. 1) are largely consistent with published guidelines [6, 80], recent decision-making analyses [76], and real-world practices [85,86,87]. For first-line therapy, current data and clinical experience suggest that all patients who are able to tolerate treatment should be treated with EP in combination with a PD-L1 inhibitor (i.e., atezolizumab, durvalumab) when there is no contraindication to the use of immunotherapy (e.g., severe autoimmune disease) [6]. In patients with platinum-sensitive, relapsed SCLC—especially if the treatment-free interval has been greater than 180 days—reintroduction of EP may be a consideration [6, 80]. Patients with platinum-sensitive, relapsed SCLC whose initial therapy did not include immunotherapy (e.g., relapse after chemoradiotherapy for LS disease) may be offered EP rechallenge with the addition of a PD-L1 inhibitor (i.e., durvalumab or atezolizumab). For patients with relapse, regardless of platinum sensitivity and/or whether they received frontline immunotherapy, a clinical trial, lurbinectedin, and topoisomerase I inhibitors are all reasonable second-line therapeutic options [6, 80].
A practical management guide for ES-SCLC. aEP + immunotherapy is the preferred first-line standard of care for all patients with extensive-stage-small-cell lung cancer (ES-SCLC). In the case of a patient who previously received EP alone and remains platinum sensitive, EP rechallenge with immunotherapy may be considered. bPlatinum-sensitive is defined as either chemotherapy naive or relapse > 90 days after cessation of prior chemotherapy and platinum-resistant as relapse ≤ 90 days after prior chemotherapy. cTopotecan and irinotecan remain possible second-line options
Several guidelines vary on their preferred treatment option for relapsed SCLC on the basis of tumor sensitivity at the time of relapse and performance status. The National Comprehensive Cancer Network (NCCN) guidelines recommend (category 2A) the use of the preferred regimens of topotecan, lurbinectedin, or a clinical trial for patients with SCLC who have relapsed 6 months or less after first-line therapy [6]. Likewise, the Spanish Society of Medical Oncology (SEOM) guidelines recommend a clinical trial (preferred) as well as topotecan for patients with a relapse 3 months or less from their last platinum dose [80]. In 2020, European SCLC expert analysis identified CAV as the preferred option in fit patients with a relapse less than 3 months from the last platinum dose and a preference for topotecan in unfit patients with a relapse less than 3 months after the last platinum dose [76]. However, on the basis of the review of the most current evidence along with the clinical concerns for using topotecan (schedule, limited efficacy, and myelosuppressive toxicity), the authors do not frequently use topotecan as second-line treatment for patients with relapsed SCLC, although it is still approved on the basis of evidence from randomized phase 3 data and is used in this setting both in the USA and elsewhere. Irinotecan remains an alternative topoisomerase I inhibitor option in this setting. In the absence of head-to-head comparative data, given the more favorable risk–benefit profile with regards to myelosuppression, and given the less frequent dosing schedule, lurbinectedin monotherapy may be considered as the preferred agent over topotecan as a second-line treatment option in patients with chemotherapy-sensitive and chemotherapy-resistant relapsed ES-SCLC. However, the one major limitation is that lurbinectedin is under conditional accelerated approval based only on data from a phase 2, open-label, single-arm trial in 105 patients and the phase 3 randomized study of combination lurbinectedin and doxorubicin that failed to show OS benefit, without a full publication available to examine the implications of this result. For many patients with relapsed ES-SCLC, a clinical trial with a novel investigational agent may be the preferred approach, while transition to hospice care remains an option for those with poor performance status (i.e., 3–4) and/or those who wish to focus on comfort.
Biomarkers and Experimental Therapies: Future Outlook
Presently, there are no biomarkers with sufficient evidence to guide second-line treatment choices for patients with relapsed SCLC, although some potential biomarkers and investigational targeted therapies offer future promise [22, 33, 88,89,90,91]. Ongoing clinical trials aim to explore potential biomarkers to predict responsiveness to certain agents, which—it is hoped—will allow for greater advances in the field.
Biomarkers in Development and Therapeutic Targets
Delta-Like Ligand 3 (DLL-3)
DLL-3 has been postulated as a biomarker with prognostic implications in SCLC. DLL-3 is a protein that is expressed at a high level in SCLC tumor cells and at low-to-minimal levels in normal tissues [33, 92]. A 2017 phase 1 study suggested that DLL-3 expression may have prognostic significance in SCLC [93], while three other studies indicated that it did not [94,95,96]. Rovalpituzumab tesirine (Rova-T), the first DLL-3-targeted antibody–drug conjugate, initially showed promise as a treatment in SCLC [97], but later failed to demonstrate superiority in a randomized phase 3 trial when compared with topotecan, with inferior OS, PFS, and ORR seen in patients receiving Rova-T. Additionally, Rova-T was noted to have a challenging toxicity profile of significant cutaneous reactions and fluid accumulation [98]. Other DLL-3 inhibitors are currently being investigated in clinical trials of SCLC, most notably, bispecific T cell engagers and chimeric antigen receptor T cells (CAR-T) [99].
Poly (ADP-Ribose) Polymerase (PARP) and Promising Biomarker Schlafen 11 (SLFN11)
PARPs are a family of enzymes that play a key role in repairing damaged DNA, including that caused by chemotherapeutic agents, by detecting and mending single-stranded DNA breaks [22, 35]. PARP inhibitors may enhance DNA-damaging or cytotoxic effects when co-administered with other chemotherapeutic agents [35, 100]. PARP is highly expressed in SCLC tissue and has become a target for therapeutic drug development [22, 35]. PARP inhibitors currently being investigated in SCLC clinical trials include veliparib (NCT02289690, NCT01642251, NCT01638546, and NCT03227016), olaparib (NCT04728230, NCT03923270, and NCT02446704), and niraparib (NCT04701307, NCT03830918, and NCT04592237).
SLFN11, a DNA/RNA helicase that irreversibly induces a block of replication and leads to cell death, is emerging as a biomarker of response for PARP inhibitors [101]. SLFN11 has also been purported to predict sensitivity to cytotoxic or DNA-damaging chemotherapies, such as topoisomerase I inhibitors (i.e., topotecan, irinotecan) and topoisomerase II inhibitors (i.e., etoposide), as well as DNA cross-linkers and alkylating agents (e.g., cisplatin) [97]. A recent study reported that PARP activity correlates with SLFN11 expression in SCLC cell lines and patient-derived xenograft models [102]. These findings suggest that SLFN11 may be a relevant predictive biomarker of sensitivity to PARP inhibitors, which are currently being explored in clinical trials in SCLC.
For example, in a phase 2 study of temozolomide plus veliparib or placebo in patients with relapsed SCLC, PFS and OS did not differ significantly between the two treatment arms. However, SLFN11 expression was associated with a significant improvement in PFS and OS in patients receiving temozolomide plus veliparib compared with those receiving temozolomide plus placebo, suggesting that SLFN11 is a promising biomarker of PARP-inhibitor sensitivity that may identify patients who benefit from this therapy [100]. An ongoing phase II study (NCT04334941) in the frontline setting of maintenance atezolizumab versus atezolizumab in combination with talazoparib in patients with SLFN11-positive ES-SCLC will examine the value of the SLFN11 biomarker in a prospective manner.
Cyclin-Dependent Kinase 4/6 (CDK 4/6)
Trilaciclib is a short-acting CDK 4/6 inhibitor designed to arrest bone marrow progenitors in the G1 phase of the cycle during cytotoxic chemotherapy with the goal of preventing myelosuppression. On the basis of three successful randomized phase 2 studies (NCT03041311, NCT02499770, and NCT02514447), trilaciclib was FDA approved in February 2021 to decrease the incidence of chemotherapy-induced myelosuppression when administered prior to an EP-containing regimen or a topotecan-containing regimen for ES-SCLC [103, 104]. The myeloprotective effects of trilaciclib have been shown when combined with EP in patients with treatment-naïve ES-SCLC [105], in previously treated patients with ES-SCLC before beginning topotecan treatment [106], and when administered prior to EP plus atezolizumab in patients with treatment-naïve ES-SCLC [107]. Although no significant differences in efficacy were observed in the pooled analysis from three phase 2 studies that resulted in the approval of trilaciclib, the addition of trilaciclib prior to chemotherapy resulted in clinically meaningful reduction in chemotherapy-induced myelosuppression [108]. Moreover, in preclinical models, it was noted that the addition of trilaciclib to combination chemotherapy/immune-checkpoint inhibitor enhanced antitumor responses compared with combination chemotherapy/immune-checkpoint alone [109]. Furthermore, peripheral lymphocyte counts increased and T cell activation was enhanced following transient exposure of patients with SCLC to trilaciclib during chemotherapy, suggesting that trilaciclib may also enhance immune function when coadministered with chemotherapy [109]. There is an ongoing phase 2 study (NCT03041311) of trilaciclib with EP and atezolizumab in the frontline setting for ES-SCLC.
Conclusions
Prognosis for patients with ES-SCLC remains poor, even with treatment. EP has been the standard-of-care, first-line treatment option for nearly 30 years. Only recently have PD-L1 immunotherapies (atezolizumab and durvalumab) begun to enter the therapeutic armamentarium, with standard use in combination with EP. The best second-line therapy after combination of chemo-immunotherapy is not well defined, as many second-line therapies were studied only after use of EP. However, second-line treatment options for patients with relapsed ES-SCLC are limited and include reintroduction of EP (with or without an immunotherapy), lurbinectedin, and topotecan. For many patients, participation in a clinical trial and transition to hospice care are preferred options. Research efforts continue in the identification of biomarkers with potential prognostic significance and predictive value with certain therapeutics. Better understanding of the molecular characteristics of SCLC and the development of biomarkers will lead to more rapid advances and better guide treatment decisions in the future.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006;24:4539–44.
Kalemkerian GP, Loo BW, Akerley W, et al. NCCN guidelines insights: small cell lung cancer, version 2.2018. J Natl Compr Cancer Netw. 2018;16:1171–82.
Oronsky B, Reid TR, Oronsky A, Carter CA. What’s new in SCLC? A review. Neoplasia. 2017;19:842–7.
Assi HA, Padda SK. Latest advances in management of small cell lung cancer and other neuroendocrine tumors of the lung. Cancer Treat Res Commun. 2020;23:100167.
National Comprehensive Cancer Network. Small cell lung cancer. Version 1.2021 – August 11, 2020. https://www.nccn.org/professionals/physician_gls/pdf/sclc.pdf. Accessed 21 May 2021.
Wang S, Zimmermann S, Parikh K, Mansfield AS, Adjei AA. Current diagnosis and management of small-cell lung cancer. Mayo Clin Proc. 2019;94:1599–622.
Yang S, Zhang Z, Wang Q. Emerging therapies for small cell lung cancer. J Hematol Oncol. 2019;12:47.
DiBonaventura MD, Shah-Manek B, Higginbottom K, Penrod JR, Yuan Y. Adherence to recommended clinical guidelines in extensive disease small-cell lung cancer across the US, Europe, and Japan. Ther Clin Risk Manag. 2019;15:355–66.
Janssen-Heijnen ML, Schipper RM, Razenberg PP, Crommelin MA, Coebergh JW. Prevalence of co-morbidity in lung cancer patients and its relationship with treatment: a population-based study. Lung Cancer. 1998;21:105–13.
Foster NR, Mandrekar SJ, Schild SE, et al. Prognostic factors differ by tumor stage for small cell lung cancer: a pooled analysis of North Central Cancer Treatment Group trials. Cancer. 2009;115:2721–31.
Ou SH, Ziogas A, Zell JA. Prognostic factors for survival in extensive stage small cell lung cancer (ED-SCLC): the importance of smoking history, socioeconomic and marital statuses, and ethnicity. J Thorac Oncol. 2009;4:37–43.
Guo H, Li L, Cui J. Advances and challenges in immunotherapy of small cell lung cancer. Chin J Cancer Res. 2020;32:115–28.
Demedts IK, Vermaelen KY, van Meerbeeck JP. Treatment of extensive-stage small cell lung carcinoma: current status and future prospects. Eur Respir J. 2010;35:202–15.
Zatloukal P, Cardenal F, Szczesna A, et al. A multicenter international randomized phase III study comparing cisplatin in combination with irinotecan or etoposide in previously untreated small-cell lung cancer patients with extensive disease. Ann Oncol. 2010;21:1810–6.
Schmittel A, Sebastian M, von Weikersthal LF, et al. A German multicenter, randomized phase III trial comparing irinotecan–carboplatin with etoposide–carboplatin as first-line therapy for extensive-disease small-cell lung cancer. Ann Oncol. 2011;22:1798–804.
Zhou T, Zhang Z, Luo F, et al. Comparison of first-line treatments for patients with extensive-stage small cell lung cancer: a systematic review and network meta-analysis. JAMA Netw Open. 2020;3: e2015748. https://doi.org/10.1001/jamanetworkopen.2020.15748.
Kim DW, Kim HG, Kim JH, et al. Randomized phase III trial of irinotecan plus cisplatin versus etoposide plus cisplatin in chemotherapy-naïve Korean patients with extensive-disease small cell lung cancer. Cancer Res Treat. 2019;52:119–27.
Horn L, Mansfield AS, Szczesna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–9.
Paz-Ares L, Dvorkin M, Chen Y, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–39.
Huang C, Gan GN, Zhang J. IMpower, CASPIAN, and more: exploring the optimal first-line immunotherapy for extensive-stage small cell lung cancer. J Hematol Oncol. 2020;13:69.
Serzan MT, Farid S, Liu SV. Drugs in development for small cell lung cancer. J Thorac Dis. 2020;12:6298–307.
Ragavan M, Das M. Systemic therapy of extensive stage small cell lung cancer in the era of immunotherapy. Curr Treat Options Oncol. 2020;21:64.
Goldman JW, Dvorkin M, Chen Y, et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide versus platinum-etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2021;22:51–65.
Reck M, Luft A, Szczesna A, et al. Phase III randomized trial of ipilimumab plus etoposide and platinum versus placebo plus etoposide and platinum in extensive-stage small-cell lung cancer. J Clin Oncol. 2016;34:3740–8.
Mansfield AS, Kazarnowicz A, Karaseva N, et al. Safety and patient-reported outcomes of atezolizumab, carboplatin, and etoposide in extensive-stage small-cell lung cancer (IMpower133): a randomized phase I/III trial. Ann Oncol. 2020;31:310–7.
Liu SV, Reck M, Mansfield AS, et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J Clin Oncol. 2021;39:619–30.
Wang Z, Duan J, Cai S, et al. Assessment of blood tumor mutational burden as a potential biomarker for immunotherapy in patients with non-small cell lung cancer with use of a next-generation sequencing cancer gene panel. JAMA Oncol. 2019;5:696–702.
Gandara DR, Paul SM, Kowanetz M, et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med. 2018;24:1441–8.
Facchinetti F, Di Maio M, Tiseo M. Adding PD-1/PD-L1 inhibitors to chemotherapy for the first-line treatment of extensive stage small cell lung cancer (SCLC): a meta-analysis of randomized trials. Cancers. 2020;12:2645.
Rudin CM, Awad MM, Navarro A, et al. Pembrolizumab or placebo plus etoposide and platinum as first-line therapy for extensive-stage small-cell lung cancer: randomized, double-blind, phase III KEYNOTE-604 study. J Clin Oncol. 2020;38:2369–79.
IMFINZI® (durvalumab) injection, for intravenous use [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2021.
TECENTRIQ® (atezolizumab) injection, for intravenous use [package insert]. South San Francisco, CA: Genentech, Inc.; 2021.
Esposito G, Palumbo G, Carillio G, et al. Immunotherapy in small cell lung cancer. Cancers. 2020;12:2522. https://doi.org/10.3390/cancers12092522.
Farid S, Liu SV. A narrative review of salvage therapy in small cell lung cancer. Precis Cancer Med. 2020;3:20.
Cheng S, Evans WK, Stys-Norman D, Shepherd FA, Lung Cancer Disease Site Group of Cancer Care Ontario’s Program in Evidence-based Care. Chemotherapy for relapsed small cell lung cancer: a systematic review and practice guideline. J Thorac Oncol. 2007;2:348–54.
Owonikoko TK, Behera M, Chen Z, et al. A systematic analysis of efficacy of second-line chemotherapy in sensitive and refractory small-cell lung cancer. J Thorac Oncol. 2012;7:866–72.
HYCAMTIN® (topotecan) for injection, for intravenous use [package insert]. East Hanover NJ: Novartis Pharmaceuticals Corporation; 2019.
TOPOTECAN injection for intravenous use [package insert]. Lake Forest, IL: Hospira, Inc.; 2020.
von Pawel J, Schiller JH, Shepherd FA, et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol. 1999;17:658–67.
von Pawel J, Gatzemeier U, Pujol JL, et al. Phase II comparator study of oral versus intravenous topotecan in patients with chemosensitive small-cell lung cancer. J Clin Oncol. 2001;19:1743–9.
O’Brien ME, Ciuleanu TE, Tsekov H, et al. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol. 2006;24:5441–7.
Shah C, Ready N, Perry M, et al. A multi-center phase II study of weekly topotecan as second-line therapy for small cell lung cancer. Lung Cancer. 2007;57:84–8.
Eckardt JR, von Pawel J, Pujol JL, et al. Phase III study of oral compared with intravenous topotecan as second-line therapy in small-cell lung cancer. J Clin Oncol. 2007;25:2086–92.
Spigel DR, Greco FA, Burris HA 3rd, et al. A phase II study of higher dose weekly topotecan in relapsed small-cell lung cancer. Clin Lung Cancer. 2011;12:187–91. https://doi.org/10.1016/j.cllc.2011.03.016.
von Pawel J, Jotte R, Spigel DR, et al. Randomized phase III trial of amrubicin versus topotecan as second-line treatment for patients with small-cell lung cancer. J Clin Oncol. 2014;32:4012–9.
Goto K, Ohe Y, Shibata T, et al. Combined chemotherapy with cisplatin, etoposide, and irinotecan versus topotecan alone as second-line treatment for patients with sensitive relapsed small-cell lung cancer (JCOG0605): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2016;17:1147–57.
Baize N, Monnet I, Greillier L, et al. Carboplatin plus etoposide versus topotecan as second-line treatment for patients with sensitive relapsed small-cell lung cancer: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2020;21:1224–33.
Lv C, Liu X, Zheng Q, et al. Analysis of topoisomerase I expression and identification of predictive markers for efficacy of topotecan chemotherapy in small cell lung cancer. Thorac Cancer. 2018;9:1166–73.
Kondo R, Watanabe S, Shoji S, et al. A phase II study of irinotecan for patients with previously treated small-cell lung cancer. Oncology. 2018;94:223–32.
Morgensztern D, Rose M, Waqar SN, et al. RRx-001 followed by platinum plus etoposide in patients with previously treated small-cell lung cancer. Br J Cancer. 2019;121:211–7.
ZEPZELCA™ (lurbinectedin) for injection, for intravenous use [package insert]. Palto Alto, CA: Jazz Pharmaceuticals, Inc.; 2020.
Belgiovine C, Bello E, Liguori M, et al. Lurbinectedin reduces tumour-associated macrophages and the inflammatory tumour microenvironment in preclinical models. Br J Cancer. 2017;117:628–38.
Santamaria Nunez G, Robles CM, Giraudon C, et al. Lurbinectedin specifically triggers the degradation of phosphorylated RNA polymerase II and the formation of DNA breaks in cancer cells. Mol Cancer Ther. 2016;15:2399–412.
Kauffmann-Guerrero D, Huber RM. Orphan drugs in development for the treatment of small-cell lung cancer: emerging data on lurbinectedin. Lung Cancer. 2020;11:27–31.
Jazz Pharmaceuticals (press release). Jazz pharmaceuticals announces US FDA accelerated approval of Zepzelca™ (lurbinectedin) for the treatment of metastatic small cell lung cancer. https://investor.jazzpharma.com/news-releases/news-release-details/jazz-pharmaceuticals-announces-us-fda-accelerated-approval. Published June 15, 2020. Accessed 24 May 2021.
Trigo J, Subbiah V, Besse B, et al. Lurbinectedin as second-line treatment for patients with small-cell lung cancer: a single-arm, open-label, phase 2 basket trial. Lancet Oncol. 2020;21:645–54.
Farago AF, Drapkin BJ, Lopez-Vilarino de Ramos JA, et al. ATLANTIS: a phase III study of lurbinectedin/doxorubicin versus topotecan or cyclophosphamide/doxorubicin/vincristine in patients with small-cell lung cancer who have failed one prior platinum-containing line. Future Oncol. 2019;15:231–9.
Jazz Pharmaceuticals (press release). Jazz pharmaceuticals and PharmaMar announce results of ATLANTIS phase 3 study evaluating Zepzelca™ in combination with doxorubicin for patients with small cell lung cancer following one prior platinum-containing line. https://investor.jazzpharma.com/news-releases/news-release-details/jazz-pharmaceuticals-and-pharmamar-announce-results-atlantis. Published December 3, 2020. Accessed 24 May 2021.
Teruel CF, Lubomirov R, Fudio S. Exposure-response analyses and clinical utility index to justify the dosage of lurbinectedin in small-cell lung cancer. J Thorac Oncol. 2021;16(Suppl 3):S509.
FDA grants accelerated approval to lurbinectedin for metastatic small cell lung cancer. US Food & Drug Administration website. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-grants-accelerated-approval-lurbinectedin-metastatic-small-cell-lung-cancer. Published June 16, 2020. Accessed 18 Aug 2021.
Ponce-Aix S, Cote GM, Gonzalez AF, et al. Lurbinectedin (LUR) in combination with irinotecan (IRI) in patients (pts) with advanced solid tumors: updated results from a phase Ib-II trial. J Clin Oncol. 2020;38(Suppl 15):3514–3514.
Ponce-Aix S. Lurbinectedin with irinotecan in relapsed small cell lung cancer: results from the expansion stage of a phase I-II trial. Oral presentation at: 2020 World Conference on Lung Cancer; Jan 28–31, 2021; Singapore.
Pleasance ED, Stephens PJ, O’Meara S, et al. A small-cell lung cancer genome with complex signatures of tobacco exposure. Nature. 2010;463:184–90.
Calles A, Aguado G, Sandoval C, Alvarez R. The role of immunotherapy in small cell lung cancer. Clin Transl Oncol. 2019;21:961–76.
Gelsomino F, Lamberti G, Parisi C, et al. The evolving landscape of immunotherapy in small-cell lung cancer: a focus on predictive biomarkers. Cancer Treat Rev. 2019;79:101887.
KEYTRUDA® (pembrolizumab) injection, for intravenous use [package insert]. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; 2021.
Chung HC, Piha-Paul SA, Lopez-Martin J, et al. Pembrolizumab after two or more lines of previous therapy in patients with recurrent or metastatic SCLC: results from the KEYNOTE-028 and KEYNOTE-158 studies. J Thorac Oncol. 2020;15:618–27.
Ternyila, D. Nivolumab indication in small cell lung cancer withdrawn from US market. Target Oncol (online). https://www.targetedonc.com/view/nivolumab-indication-in-small-cell-lung-cancer-withdrawn-from-us-market. Published January 4, 2021. Accessed 24 May 2021.
Ott PA, Elez E, Hiret S, et al. Pembrolizumab in patients with extensive-stage small-cell lung cancer: results from the phase Ib KEYNOTE-028 study. J Clin Oncol. 2017;35:3823–9.
Strosberg J, Mizuno N, Doi T, et al. Efficacy and safety of pembrolizumab in previously treated advanced neuroendocrine tumors: results from the phase II KEYNOTE-158 study. Clin Cancer Res. 2020;26:2124–30.
Parkins K. Merck withdraws Keytruda from SCLC indication amid FDA crackdown. Clinical Trials Arena website. https://www.clinicaltrialsarena.com/news/merck-withdraws-keytruda-for-lung-cancer-amid-fda-crackdown/. Updated March 3, 2021. Accessed 29 June 2021.
Ready NE, Ott PA, Hellmann MD, et al. Nivolumab monotherapy and nivolumab plus ipilimumab in recurrent small cell lung cancer: results from the CheckMate 032 randomized cohort. J Thorac Oncol. 2020;15:426–35.
Owonikoko TK, Park K, Govindan R, et al. Nivolumab and ipilimumab as maintenance therapy in extensive-disease small-cell lung cancer: CheckMate 451. J Clin Oncol. 2021;39:1349–59.
Reck M, Vicente D, Ciuleanu T, et al. Efficacy and safety of nivolumab (nivo) monotherapy versus chemotherapy (chemo) in recurrent small cell lung cancer (SCLC): results from CheckMate 331. Ann Oncol. 2018;29(Suppl 10):x43.
Fruh M, Panje CM, Reck M, et al. Choice of second-line systemic therapy in stage IV small cell lung cancer (SCLC) – a decision-making analysis amongst European lung cancer experts. Lung Cancer. 2020;146:6–11.
Aida Y, Nakazawa K, Shiozawa T, et al. Small-cell lung cancer treatment of newly diagnosed patients with poor performance status. Case Rep Oncol. 2019;12:613–20.
Pentz RD, Hendershot KA, Wall L, et al. Development and testing of a tool to assess patient preferences for phase I clinical trial participation. Psychooncology. 2015;24:835–8.
Hianik RS, Owonikoko T, Switchenko J, Dixon MD, Shaib WL, Pentz RD. Evaluating the impact of the patient preference assessment tool on clinicians’ recommendations for phase I oncology clinical trials. Psychooncology. 2021. https://doi.org/10.1002/pon.5739.
Domine M, Moran T, Isla D, et al. SEOM clinical guidelines for the treatment of small-cell lung cancer (SCLC) (2019). Clin Transl Oncol. 2020;22:245–55.
Fruh M, De Ruysscher D, Popat S, et al. Small-cell lung cancer (SCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi99-105.
Jett JR, Schild SE, Kesler KA, Kalemkerian GP. Treatment of small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e400S – e419.
Samson DJ, Seidenfeld J, Simon GR, et al. Evidence for management of small cell lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132:314S-S323.
Zhao H, Ren D, Liu H, Chen J. Comparison and discussion of the treatment guidelines for small cell lung cancer. Thorac Cancer. 2018;9:769–74.
Cramer-van der Welle CM, Schramel F, van Leeuwen AS, Groen HJM, van de Garde EMW, Santeon SSG. Real-world treatment patterns and outcomes of patients with extensive disease small cell lung cancer. Eur J Cancer Care. 2020;29:e13250.
Einhorn LH, Pennington K, McClean J. Phase II trial of daily oral VP-16 in refractory small cell lung cancer: a Hoosier Oncology Group study. Semin Oncol. 1990;17:32–5.
Steffens CC, Elender C, Hutzschenreuter U, et al. Treatment and outcome of 432 patients with extensive-stage small cell lung cancer in first, second and third line – results from the prospective German TLK cohort study. Lung Cancer. 2019;130:216–25.
Baine MK, Hsieh MS, Lai WV, et al. SCLC subtypes defined by ASCL1, NEUROD1, POU2F3, and YAP1: a comprehensive immunohistochemical and histopathologic characterization. J Thorac Oncol. 2020;15:1823–35.
Gadgeel SM. Targeted therapy and immune therapy for small cell lung cancer. Curr Treat Options Oncol. 2018;19:53.
Saito M, Shiraishi K, Goto A, Suzuki H, Kohno T, Kono K. Development of targeted therapy and immunotherapy for treatment of small cell lung cancer. Jpn J Clin Oncol. 2018;48:603–8.
Stewart CA, Gay CM, Xi Y, et al. Single-cell analyses reveal increased intratumoral heterogeneity after the onset of therapy resistance in small-cell lung cancer. Nat Cancer. 2020;1:423–36.
Owen DH, Giffin MJ, Bailis JM, Smit MA, Carbone DP, He K. DLL3: an emerging target in small cell lung cancer. J Hematol Oncol. 2019;12:61.
Rudin CM, Pietanza MC, Bauer TM, et al. Rovalpituzumab tesirine, a DLL3-targeted antibody-drug conjugate, in recurrent small-cell lung cancer: a first-in-human, first-in-class, open-label, phase 1 study. Lancet Oncol. 2017;18:42–51.
Tendler S, Kanter L, Lewensohn R, Ortiz-Villalon C, Viktorsson K, De Petris L. The prognostic implications of Notch1, Hes1, Ascl1, and DLL3 protein expression in SCLC patients receiving platinum-based chemotherapy. PLoS One. 2020;15:e0240973.
Rojo F, Corassa M, Mavroudis D, et al. International real-world study of DLL3 expression in patients with small cell lung cancer. Lung Cancer. 2020;147:237–43.
Chen B, Li H, Liu C, et al. Potential prognostic value of delta-like protein 3 in small cell lung cancer: a meta-analysis. World J Surg Oncol. 2020;18:226.
Leonetti A, Facchinetti F, Minari R, et al. Notch pathway in small-cell lung cancer: from preclinical evidence to therapeutic challenges. Cell Oncol. 2019;42:261–73.
Blackhall F, Jao K, Greillier L, et al. Efficacy and safety of rovalpituzumab tesirine compared with topotecan as second-line therapy in DLL3-high SCLC: results from the phase 3 TAHOE study. J Thorac Oncol. 2021;S1556–0864(2):01709–13. https://doi.org/10.1016/j.jtho.2021.02.009.
Chen X, Amar N, Zhu Y, et al. Combined DLL3-targeted bispecific antibody with PD-1 inhibition is efficient to suppress small cell lung cancer growth. J Immunother Cancer. 2020;8: e000785. https://doi.org/10.1136/jitc-2020-000785.
Pietanza MC, Waqar SN, Krug LM, et al. Randomized, double-blind, phase II study of temozolomide in combination with either veliparib or placebo in patients with relapsed-sensitive or refractory small-cell lung cancer. J Clin Oncol. 2018;36:2386–94.
Coleman N, Zhang B, Byers LA, Yap TA. The role of Schlafen 11 (SLFN11) as a predictive biomarker for targeting the DNA damage response. Br J Cancer. 2021;124:857–9.
Lok BH, Gardner EE, Schneeberger VE, et al. PARP inhibitor activity correlates with SLFN11 Expression and demonstrates synergy with temozolomide in small cell lung cancer. Clin Cancer Res. 2017;23:523–35.
G1 Therapeutics (press release). FDA approves G1 therapeutics’ COSELA™ (trilaciclib): the first and only myeloprotection therapy to decrease the incidence of chemotherapy-induced myelosuppression; Intrado GlobalNewswire website. https://www.globenewswire.com/news-release/2021/02/13/2175184/0/en/FDA-Approves-G1-Therapeutics-COSELA-trilaciclib-The-First-and-Only-Myeloprotection-Therapy-to-Decrease-the-Incidence-of-Chemotherapy-Induced-Myelosuppression.html. Published February 12, 2021. Accessed 24 May 2021.
COSELA™ (trilaciclib) for injection, for intravenous use [package insert]. Durham, NC: G1 Therapeutics, Inc.; 2021.
Weiss JM, Csoszi T, Maglakelidze M, et al. Myelopreservation with the CDK4/6 inhibitor trilaciclib in patients with small-cell lung cancer receiving first-line chemotherapy: a phase Ib/randomized phase II trial. Ann Oncol. 2019;30:1613–21.
Hart LL, Ferrarotto R, Andric ZG, et al. Myelopreservation with trilaciclib in patients receiving topotecan for small cell lung cancer: results from a randomized, double-blind, placebo-controlled phase II study. Adv Ther. 2021;38:350–65.
Daniel D, Kuchava V, Bondarenko I, et al. Trilaciclib prior to chemotherapy and atezolizumab in patients with newly diagnosed extensive-stage small cell lung cancer: a multicentre, randomised, double-blind, placebo-controlled phase II trial. Int J Cancer. 2020;148:2557–70.
Weiss J, Goldschmidt J, Andric Z, et al. Effects of trilaciclib on chemotherapy-induced myelosuppression and patient-reported outcomes in patients with extensive-stage small cell lung cancer: pooled results from three phase II randomized, double-blind, placebo-controlled studies. Clin Lung Cancer. 2021. https://doi.org/10.1016/j.cllc.2021.03.010.
Lai AY, Sorrentino JA, Dragnev KH, et al. CDK4/6 inhibition enhances antitumor efficacy of chemotherapy and immune checkpoint inhibitor combinations in preclinical models and enhances T-cell activation in patients with SCLC receiving chemotherapy. J Immunother Cancer. 2020;8:e000847.
Acknowledgements
Funding
Funding for this manuscript and the Rapid Service and Open Access Fees were provided by Jazz Pharmaceuticals through an unrestricted educational grant. Jazz Pharmaceuticals had no control over the content and development of this manuscript.
Medical Writing and Editorial Assistance
Michael Coco, PhD, of Coco Communications Inc. (Atlanta, GA) and Meri Pozo, PhD, CMPP of inScience Communications, Springer Healthcare (New York, NY, USA) and Elizabeth Samander, PhD of Springer Healthcare (New York, NY, USA) provided medical writing support. Brad Zerlanko, PhD of Springer Healthcare (Jersey City, NJ, USA) provided editorial support. This assistance was funded by Jazz Pharmaceuticals (Palo Alto, CA, USA).
Authorship
The named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript and take responsibility for the integrity of the work as a whole.
Authorship Contributions
The authors (Millie Das, Sukhmani K. Padda, Jared Weiss, Taofeek F. Owonikoko) equally participated in the development of the manuscript, had full editorial control, reviewed and edited various drafts, and provided their final approval of all content and submission for publication.
Disclosures
The authors report the following potential conflicts of interest: Millie Das discloses research funding from CellSight, Novartis, Abbvie, Celgene, United Therapeutics, and Varian; advisory board fees from AstraZeneca, Bristol Myers Squibb, and Beigene; consulting fees from Jazz Pharmaceuticals. Sukhmani K. Padda discloses research funding from Bayer, Boehringer Ingelheim and Epicentrx; and advisory board fees from Abbvie, AstraZeneca CA, Blueprint, Clovis, G1 Therapeutics, Janssen Pharmaceuticals, and Pfizer. Jared Weiss discloses consulting fees from Abbvie, AstraZeneca, Azitra, Blueprint MedicinesCelgene, EMD Serono, Genentech, G1 Therapeutics, Inivata, Jounce Therapeutics, Rakuten, Lilly, Nanobiotix, Pfizer, Saatchi Welness; and research funding from Celgene, Pfizer, Merck, AstraZeneca/Medimmune, Amgen, Carefusion, G1 Therapeutics, Immunicum, and Lilly. Taofeek K. Owonikoko discloses consulting fees from Novartis, Celgene, Lilly, Sandoz, Abbvie, Eisai, G1 Therapeutics, Takeda, Seattle Genetics, Bristol-Myers Squibb, MedImmune, BerGenBio, Lilly, Amgen, AstraZeneca, PharmaMar, Boehringer Ingelheim, EMD Serono, XCovery, Bayer, Heron Pharmaceutical, ARMO BioSciences, Merck, Bayer, Jazz Pharmaceuticals; and research funding from Novartis, Astellas Pharma, Bayer, StemCentRx, Regeneron, AstraZeneca/MedImmune, Abbvie, G1 Therapeutics, Bristol-Myers, Corvus Pharmaceuticals, United Therapeutics, Amgen, Loxo/Lilly, Fujifilm, Pfizer, Aeglea Biotherapeutics, Incyte, Merck, Mersana, Turning Point, and Oncorus. Dr Owonikoko is now chief of the Division of Hematology and Oncology, Department of Medicine, at the University of Pittsburgh, Pittsburgh, PA.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Das, M., Padda, S.K., Weiss, J. et al. Advances in Treatment of Recurrent Small Cell Lung Cancer (SCLC): Insights for Optimizing Patient Outcomes from an Expert Roundtable Discussion. Adv Ther 38, 5431–5451 (2021). https://doi.org/10.1007/s12325-021-01909-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01909-1