Abstract
Purpose of Review
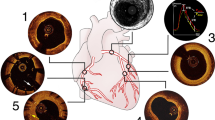
Our objective is to review the current status of OCT-guided treatment of calcified coronary artery disease.
Recent Findings
New treatment modalities provide multiple options for approaching interventions involving calcified lesions.
Summary
Coronary artery calcification is associated with stent underexpansion and worse procedural outcomes. Optimizing stent expansion is essential to reduce restenosis and the need for revascularization. Optical coherence tomography (OCT) allows for accurate diagnosis and detailed characterization of calcified lesions. The features of coronary artery calcification are determinant of the optimal lesion preparation and treatment strategy. We recommend an OCT-guided treatment approach for calcified coronary lesions.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Barbato E, Shlofmitz E, Milkas A, Shlofmitz R, Azzalini L, Colombo A. State of the art: evolving concepts in the treatment of heavily calcified and undilatable coronary stenoses - from debulking to plaque modification, a 40-year-long journey. EuroIntervention. 2017;13(6):696–705 A review of severe coronary calcification and contemporary treatment approaches.
Genereux P, Madhavan MV, Mintz GS, Maehara A, Palmerini T, Lasalle L, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) and ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trials. J Am Coll Cardiol. 2014;63(18):1845–54.
Mintz GS. Intravascular imaging of coronary calcification and its clinical implications. JACC Cardiovasc Imaging. 2015;8(4):461–71.
Madhavan MV, Tarigopula M, Mintz GS, Maehara A, Stone GW, Genereux P. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol. 2014;63(17):1703–14.
Maehara A, Ben-Yehuda O, Ali Z, Wijns W, Bezerra HG, Shite J, et al. Comparison of stent expansion guided by optical coherence tomography versus intravascular ultrasound: the ILUMIEN II study (observational study of optical coherence tomography [OCT] in patients undergoing fractional flow reserve [FFR] and percutaneous coronary intervention). JACC Cardiovasc Interv. 2015;8(13):1704–14.
Stack RS. New interventional technologies in cardiology. Mayo Clin Proc. 1989;64(7):867–70.
Yock PG, Linker DT, White NW, Rowe MH, Selmon MR, Robertson GC, et al. Clinical applications of intravascular ultrasound imaging in atherectomy. Int J Card Imaging. 1989;4(2–4):117–25.
Shlofmitz E, Kuku KO, Waksman R, Garcia-Garcia HM. Intravascular ultrasound-guided drug-eluting stent implantation. Minerva Cardioangiol. 2019.
Maehara A, Matsumura M, Ali ZA, Mintz GS, Stone GW. IVUS-guided versus OCT-guided coronary stent implantation: a critical appraisal. JACC Cardiovasc Imaging. 2017;10(12):1487–503.
Parviz Y, Shlofmitz E, Fall KN, Konigstein M, Maehara A, Jeremias A, et al. Utility of intracoronary imaging in the cardiac catheterization laboratory: comprehensive evaluation with intravascular ultrasound and optical coherence tomography. Br Med Bull. 2018;125(1):79–90.
Mintz GS, Douek P, Pichard AD, Kent KM, Satler LF, Popma JJ, et al. Target lesion calcification in coronary artery disease: an intravascular ultrasound study. J Am Coll Cardiol. 1992;20(5):1149–55.
Wang X, Matsumura M, Mintz GS, Lee T, Zhang W, Cao Y, et al. In vivo calcium detection by comparing optical coherence tomography, intravascular ultrasound, and angiography. JACC Cardiovasc Imaging. 2017;10(8):869–79.
Mintz GS, Popma JJ, Pichard AD, Kent KM, Satler LF, Chuang YC, et al. Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation. 1995;91(7):1959–65.
Hong MK, Mintz GS, Lee CW, Park DW, Choi BR, Park KH, et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006;27(11):1305–10.
• Shlofmitz E, Shlofmitz RA, Galougahi KK, Rahim HM, Virmani R, Hill JM, et al. Algorithmic Approach for optical coherence tomography-guided stent implantation during percutaneous coronary intervention. Interv Cardiol Clin. 2018;7(3):329–44 Review of an algorithmic approach to incorporating optical coherence tomography for routine use with percutaneous coronary interventions.
Shlofmitz E, Garcia-Garcia HM, Rogers T, Khalid N, Chen Y, Kajita AH, et al. Techniques to optimize the use of optical coherence tomography: insights from the Manufacturer and User Facility Device Experience (MAUDE) database. Cardiovasc Revasc Med. 2019;20:507–12.
Prati F, Cera M, Ramazzotti V, Imola F, Giudice R, Albertucci M. Safety and feasibility of a new non-occlusive technique for facilitated intracoronary optical coherence tomography (OCT) acquisition in various clinical and anatomical scenarios. EuroIntervention. 2007;3(3):365–70.
• Yamamoto MH, Maehara A, Song L, Matsumura M, Chin CY, Losquadro M, et al. Optical coherence tomography assessment of morphological characteristics in suspected coronary artery disease, but angiographically nonobstructive lesions. Cardiovasc Revasc Med. 2018; The authors highlight the importance of intravascular imaging when coronary disease is suspected but not appreciated by angiography alone.
Lee T, Mintz GS, Matsumura M, Zhang W, Cao Y, Usui E, et al. Prevalence, predictors, and clinical presentation of a calcified nodule as assessed by optical coherence tomography. JACC Cardiovasc Imaging. 2017;10(8):883–91.
•• Fujino A, Mintz GS, Matsumura M, Lee T, Kim SY, Hoshino M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018;13(18):e2182–e9 The authors introduce a new classification system to predict the risk of stent underexpansion based on the severity of calcification on optical coherence tomography.
Tomey MI, Kini AS, Sharma SK. Current status of rotational atherectomy. JACC Cardiovasc Interv. 2014;7(4):345–53.
Lee MS, Gordin JS, Stone GW, Sharma SK, Saito S, Mahmud E, et al. Orbital and rotational atherectomy during percutaneous coronary intervention for coronary artery calcification. Catheter Cardiovasc Interv. 2018;92(1):61–7.
Abdel-Wahab M, Richardt G, Joachim Buttner H, Toelg R, Geist V, Meinertz T, et al. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: the randomized ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. JACC Cardiovasc Interv. 2013;6(1):10–9.
Reifart N, Vandormael M, Krajcar M, Gohring S, Preusler W, Schwarz F, et al. Randomized comparison of angioplasty of complex coronary lesions at a single center. Excimer Laser, Rotational Atherectomy, and Balloon Angioplasty Comparison (ERBAC) study. Circulation. 1997;96(1):91–8.
Dill T, Dietz U, Hamm CW, Kuchler R, Rupprecht HJ, Haude M, et al. A randomized comparison of balloon angioplasty versus rotational atherectomy in complex coronary lesions (COBRA study). Eur Heart J. 2000;21(21):1759–66.
Abdel-Wahab M, Toelg R, Byrne RA, Geist V, El-Mawardy M, Allali A, et al. High-speed rotational atherectomy versus modified balloons prior to drug-eluting stent implantation in severely calcified coronary lesions. Circ Cardiovasc Interv. 2018;11(10):e007415.
Amemiya K, Yamamoto MH, Maehara A, Oyama Y, Igawa W, Ono M, et al. Effect of cutting balloon after rotational atherectomy in severely calcified coronary artery lesions as assessed by optical coherence tomography. Catheter Cardiovasc Interv. 2019.
Shlofmitz E, Martinsen BJ, Lee M, Rao SV, Genereux P, Higgins J, et al. Orbital atherectomy for the treatment of severely calcified coronary lesions: evidence, technique, and best practices. Expert Rev Med Devices. 2017;14(11):867–79.
Chambers JW, Feldman RL, Himmelstein SI, Bhatheja R, Villa AE, Strickman NE, et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). JACC Cardiovasc Interv. 2014;7(5):510–8.
Lee M, Genereux P, Shlofmitz R, Phillipson D, Anose BM, Martinsen BJ, et al. Orbital atherectomy for treating de novo, severely calcified coronary lesions: 3-year results of the pivotal ORBIT II trial. Cardiovasc Revasc Med. 2017;18(4):261–4.
Lee MS, Shlofmitz E, Goldberg A, Shlofmitz R. Multicenter registry of real-world patients with severely calcified coronary lesions undergoing orbital atherectomy: 1-year outcomes. J Invasive Cardiol. 2018;30(4):121–4.
Lee MS, Shlofmitz E, Kaplan B, Alexandru D, Meraj P, Shlofmitz R. Real-world multicenter registry of patients with severe coronary artery calcification undergoing orbital atherectomy. J Interv Cardiol. 2016;29(4):357–62.
Shlofmitz E, Shlofmitz R, Lee MS. Orbital atherectomy: a comprehensive review. Interv Cardiol Clin. 2019;8(2):161–71.
Yamamoto MH, Maehara A, Kim SS, Koyama K, Kim SY, Ishida M, et al. Effect of orbital atherectomy in calcified coronary artery lesions as assessed by optical coherence tomography. Catheter Cardiovasc Interv. 2018.
•• Yamamoto MH, Maehara A, Karimi Galougahi K, Mintz GS, Parviz Y, Kim SS, et al. Mechanisms of orbital versus rotational atherectomy plaque modification in severely calcified lesions assessed by optical coherence tomography. JACC Cardiovasc Interv. 2017;10(24):2584–6 A comparative assessment of the impact and mechanism of orbital atherectomy vs. rotational atherectomy.
Dini CS, Tomberli B, Mattesini A, Ristalli F, Valente S, Stolcova M, et al. Intravascular lithotripsy for calcific coronary and peripheral stenoses. EuroIntervention. 2019.
Brinton TJ, Ali ZA, Hill JM, Meredith IT, Maehara A, Illindala U, et al. Feasibility of shockwave coronary intravascular lithotripsy for the treatment of calcified coronary stenoses. Circulation. 2019;139(6):834–6.
Ali ZA, McEntegart M, Hill JM, Spratt JC. Intravascular lithotripsy for treatment of stent underexpansion secondary to severe coronary calcification. Eur Heart J. 2018.
Watkins S, Good R, Hill J, Brinton TJ, Oldroyd KG. Intravascular lithotripsy to treat a severely under-expanded coronary stent. EuroIntervention. 2018.
Alfonso F, Bastante T, Antuna P, de la Cuerda F, Cuesta J, Garcia-Guimaraes M, et al. Coronary lithoplasty for the treatment of undilatable calcified de novo and in-stent restenosis lesions. JACC Cardiovasc Interv. 2019;12(5):497–9.
Fujino A, Mintz GS, Lee T, Hoshino M, Usui E, Kanaji Y, et al. Predictors of calcium fracture derived from balloon angioplasty and its effect on stent expansion assessed by optical coherence tomography. JACC Cardiovasc Interv. 2018;11(10):1015–7.
Meraj PM, Shlofmitz E, Kaplan B, Jauhar R, Doshi R. Clinical outcomes of atherectomy prior to percutaneous coronary intervention: a comparison of outcomes following rotational versus orbital atherectomy (COAP-PCI study). J Interv Cardiol. 2018;31(4):478–85.
Koifman E, Garcia-Garcia HM, Kuku KO, Kajita AH, Buchanan KD, Steinvil A, et al. Comparison of the efficacy and safety of orbital and rotational atherectomy in calcified narrowings in patients who underwent percutaneous coronary intervention. Am J Cardiol. 2018;121(8):934–9.
Lee MS, Park KW, Shlofmitz E, Shlofmitz RA. Comparison of rotational atherectomy versus orbital atherectomy for the treatment of heavily calcified coronary plaques. Am J Cardiol. 2017;119(9):1320–3.
Kubo T, Shinke T, Okamura T, Hibi K, Nakazawa G, Morino Y, et al. Comparison between Optical COherence tomography guidance and Angiography guidance in percutaneous coronary intervention (COCOA): study protocol for a randomized controlled trial. J Cardiol. 2018;72(2):170–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
F. Sosa is an employee of Abbott Vascular.
Z. Ali has served as a consultant to Abbott Vascular, Boston Scientific, Opsens Medical, Cardinal Health, and Canon; has equity/options in Shockwave Medical; and has received research grants from Abbott Vascular, the National Heart, Lung, and Blood Institute, and Cardiovascular Systems Inc.
R. Waksman has served on the advisory boards of Abbott Vascular, Amgen, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, and Pi-Cardia Ltd.; as a consultant for Abbott Vascular, Amgen, Biosensors, Biotronik, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, and Pi-Cardia Ltd.; has received grant support from Abbott Vascular, AstraZeneca, Biosensors, Biotronik, Boston Scientific, and Chiesi; has served on the speakers bureaus of AstraZeneca and Chiesi; and has invested in MedAlliance.
A. Jeremias has received educational grants from and served as a consultant for Abbott Vascular and Philips; and has served as a consultant for Opsens.
All other authors have no conflict of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Intravascular Imaging
Rights and permissions
About this article
Cite this article
Shlofmitz, E., Sosa, F.A., Ali, Z.A. et al. OCT-Guided Treatment of Calcified Coronary Artery Disease: Breaking the Barrier to Stent Expansion. Curr Cardiovasc Imaging Rep 12, 32 (2019). https://doi.org/10.1007/s12410-019-9509-1
Published:
DOI: https://doi.org/10.1007/s12410-019-9509-1