Abstract
Purpose
Thoracic endovascular aortic aneurysm repair (TEVAR) has become a mainstay of therapy for aneurysms and other disorders of the thoracic aorta. The purpose of this narrative review article is to summarize the current literature on the risk factors for and pathophysiology of spinal cord injury (SCI) following TEVAR, and to discuss various intraoperative monitoring and treatment strategies.
Source
The articles considered in this review were identified through PubMed using the following search terms: thoracic aortic aneurysm, TEVAR, paralysis+TEVAR, risk factors+TEVAR, spinal cord ischemia+TEVAR, neuromonitoring+thoracic aortic aneurysm, spinal drain, cerebrospinal fluid drainage, treatment of spinal cord ischemia.
Principal findings
Spinal cord injury continues to be a challenging complication after TEVAR. Its incidence after TEVAR is not significantly reduced when compared with open thoracoabdominal aortic aneurysm repair. Nevertheless, compared with open procedures, delayed paralysis/paresis is the predominant presentation of SCI after TEVAR. The pathophysiology of SCI is complex and not fully understood, though the evolving concept of the importance of the spinal cord’s collateral blood supply network and its imbalance after TEVAR is emerging as a leading factor in the development of SCI. Cerebrospinal fluid drainage, optimal blood pressure management, and newer surgical techniques are important components of the most up-to-date strategies for spinal cord protection.
Conclusion
Further experimental and clinical research is needed to aid in the discovery of novel neuroprotective strategies for the protection and treatment of SCI following TEVAR.
Résumé
Objectif
La réparation endovasculaire d’un anévrisme de l’aorte thoracique (TEVAR) est devenue une modalité importante du traitement des anévrismes et autres pathologies de l’aorte thoracique. L’objectif de cet article narratif de synthèse est de résumer les publications actuelles sur les facteurs de risque et la pathophysiologie des lésions de la moelle épinière après TEVAR, et de discuter des différents monitorings peropératoires et options thérapeutiques pour les lésions de la moelle épinière après TEVAR.
Source
Les articles retenus dans cette synthèse ont été identifiés dans PubMed au moyen des termes de recherche suivants : Anévrisme de l’aorte thoracique, TEVAR, paralysie +TEVAR, facteurs de risque +TEVAR, ischémie de la moelle épinière +TEVAR, monitorage neurologique + anévrisme de l’aorte thoracique, drain spinal, drainage de liquide céphalo-rachidien, traitement de l’ischémie de la moelle épinière ischémie.
Constatations principales
Les lésions de la moelle épinière après TEVAR restent une complication problématique. Leur incidence après TEVAR n’est pas significativement réduite par rapport à la réparation thoraco-abdominale ouverte des anévrismes de l’aorte. Néanmoins, comparativement aux interventions ouvertes, la paralysie/parésie tardive est le tableau prédominant des lésions de la moelle après TEVAR. La pathophysiologie des lésions de la moelle épinière est complexe et encore mal comprise, bien que le concept actuel de l’importance de l’apport sanguin du réseau vasculaire collatéral de la moelle et de son déséquilibre après TEVAR apparaisse comme un facteur majeur de la survenue de ces lésions médullaires. Le drainage du liquide céphalo-rachidien, une gestion optimale de la pression sanguine et de nouvelles techniques chirurgicales sont les éléments importants des plus récentes stratégies de protection de la moelle épinière.
Conclusion
Il est nécessaire de poursuivre la recherche expérimentale et la recherche clinique pour contribuer à la découverte de nouvelles stratégies de protection et de traitement des lésions de la moelle épinière après TEVAR.
Similar content being viewed by others
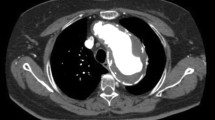
Over the last decade, thoracic endovascular aortic repair (TEVAR) has increasingly become a mainstay of therapy for thoracic aortic diseases such as aneurysm and acute aortic syndromes. Despite being less invasive than open surgical repair, TEVAR procedures are still associated with a significant risk of spinal cord injury (SCI). Crawford was the first to describe a thoracoabdominal aortic aneurysm (TAAA) classification system in 1986. The classification system, developed when only open repair was being performed, was based on the extent of the aorta involved, but it also showed an association with the relative incidence of SCI. Subsequently, the incidence of SCI after TEVAR has been largely comparable with that after open TAAA repair when compared with a similar Crawford classification (Fig. 1).1 The overall incidence of SCI (i.e., paresis or paralysis) after TEVAR ranges from 2-10%.2,3 For example, in 2011, Ullery et al. 4 reported a 2.8% incidence of SCI in a study of 424 TEVAR procedures. In 2013, DeSart et al. 5 reported a 9.4% of SCI in 607 TEVAR procedures, and in 2014, Scali et al. 6 showed a 9.2% incidence of SCI in 741 TEVAR procedures.
Thoracoabdominal aortic aneurysm repair according to Crawford’s Classification and the risk of ischemic spinal cord injury as reported by centres of excellence for aortic repair. (Reprinted by permission of Edizioni Minerva Medica from: Etz DC, Luehr M, Aspern KV, et al. Spinal cord ischemia in open and endovascular thoracoabdominal aortic aneurysm repair: new concepts. J Cardiovasc Surg (Torino) 2014; 55(2 Suppl 1): 159-68).3 TAAA = thoracoabdominal aortic aneurysm
The pathogenesis of SCI after TEVAR is multifactorial and not fully understood. There are two suggested theories behind the mechanism of SCI. The first relates to inadequate remodelling of the collateral blood supply network to maintain spinal cord viability. The second implicates atheroembolism of aortic plaque material into the segmental arteries supplying the spinal cord. Although considerable debate is circulating in the literature on the optimal preventive and definitive treatment measures for SCI after TEVAR, the main strategies are aimed at increasing mean arterial blood pressure and draining cerebrospinal fluid (CSF) in order to optimize spinal cord perfusion pressure (and blood flow). The American College of Cardiology Foundation/American Heart Association guidelines (though not updated since 2010) recommend CSF drainage for spinal cord protection in open TAAA repair and TEVAR for patients at high risk of SCI—determined by the presence of specific risk factors (e.g., prior abdominal aortic surgery).7 In 2015, the European Association for Cardio-Thoracic Surgery similarly recommended CSF drainage for TAAA repair in patients at high risk of SCI.8 Although randomized-controlled studies showed benefit for CSF drainage in open TAAA repair,9 its routine use in TEVAR procedures remains uncertain and a topic of considerable debate.8,10,11
The aim of this narrative review is to provide an overview of the risk factors for and the pathophysiology and clinical presentation of SCI following TEVAR, as well as to highlight the relevant anesthetic practices and recent surgical techniques for its prevention and treatment.
Risk of SCI in TEVAR
The advantages of the relatively less-invasive TEVAR compared with TAAA open repair are consistent with what one might expect by avoiding the extensive surgical trauma following open TAAA repair. These benefits include reductions in intensive care unit (ICU) length of stay, hospital length of stay, organ dysfunction, postoperative pain, and overall costs.12,13 Nevertheless, a similar reduction has not been seen in the incidence of SCI. To estimate the risk of SCI in TEVAR, Uchida reviewed 59 studies involving 7,309 TEVAR patients.14 Study results showed a 0-10.3% incidence of SCI, with an average of 4.5%. Recently, Etz et al.3 analyzed the risk of paralysis reported by “aortic centres of excellence” from six clinical trials of TEVAR that included 1,050 patients (from 2001 to 2008) and ten clinical trials with open TAAA repair in 6,034 patients (from 2005 to 2011). The trial results showed that the open TAAA repair and TEVAR procedures had similar rates of paralysis, especially for type II aortic aneurysm (0-22% in open TAAA repair vs 19% in TEVAR) (Fig. 1). Nevertheless, only one study mentioned the risk of SCI in TEVAR in relation to the Crawford classification. In this retrospective study, the authors reviewed 724 thoracic or TAAA repair procedures (352 TEVAR patients and 372 open TAAA repair patients). Study results did not show a significant difference in the incidence of SCI between both procedures (4.3% for TEVAR vs 7.5% for open TAAA repair; P = 0.08).15 Indeed, when compared with open TAAA repair, the reduction in SCI and paralysis was less than expected with TEVAR; moreover, delayed paralysis (i.e., > 24 hr following the procedure) occurred more frequently than acute paralysis.4,10,16
The limitation of the current literature in estimating the risk of SCI after TEVAR vs that after open TAAA repair is due to the lack of direct comparative prospective studies. In addition, the indications for TEVAR are expanding to include patients at lower risk of developing perioperative complications, which may bias recent results when compared with previous studies. Furthermore, potentially important patient demographic and surgical details are inconsistently reported in the clinical trials. Finally, the continued refinement of surgical techniques and the development of newer techniques (e.g., minimally invasive segmental artery coil embolization [MISACE] and temporary aneurysm sac perfusion [TASP]) may have an impact on the risk of SCI, which makes direct comparisons even more difficult. In future, comprehensive systematic reviews and meta-analysis that account for the previously mentioned limitations may provide a more accurate estimate of the relative risk of SCI in TEVAR patients.
Pathophysiology of SCI after TEVAR
The blood supply to the spinal cord is arguably more complex than the blood supply to any other vital organ.17 Its main blood supply comes from one anterior spinal artery and two posterior spinal arteries that run longitudinally along the cord. These anterior and posterior spinal vessels, originating from the vertebral arteries, are fed by additional collaterals from paired segmental arteries arising directly from the aorta, with two or three in the cervical region, two or three in the thoracic region, and none or one in the lumbosacral region.18 In the thoracic region, these segmental arteries arise from the aorta or the subclavian artery as intercostal arteries. The segmental arteries divide into muscular and spinal branches. The spinal branches give rise to anterior and posterior radicular arteries that join the anterior and posterior spinal arteries. The most dominant anterior radiculomedullary artery in the thoracolumbar area is known as the artery of Adamkiewicz (Fig. 2). Although historically it was considered the most important vessel supplying the spinal cord, this has largely been discounted in recent years.19
Evolution of the dynamic nature of spinal cord ischemia and paralysis after TEVAR. A: Blood flows in the paraspinous and intraspinous network under normal conditions. The arterial system is divided into a central centrifugal system supplied by the sulcal arteries and a peripheral centripetal system supplied by the pial network surrounding the spinal cord. B: Occlusion of the segmental arteries following aortic stent placement is accompanied by several compensatory mechanisms to maintain integrity of the spinal cord: (1) rerouting of blood flow from the paraspinous to the intraspinous network through the dorsal branch of the dorsal spinal artery to the ventral branch of the dorsal spinal artery supplying the radiculomedullary artery (red arrows); (2) intramedullary intraspinous collateral network between the anterior and posterior spinal arteries (green arrows); (3) extramedullary collaterals from the pial plexus; and (4) reversal of blood flow within the anterior spinal artery from nearby non-occluded segmental arteries (blue arrow). C: Failure of one or more of these compensatory mechanisms (black crosses) may lead to spinal cord ischemia: (1) No blood flow from the paraspinous to the intraspinous network (the blue color represents a thrombus in the segmental artery); (2) Absent intramedullary and extramedullary collaterals; (3) No reversal of blood flow within the anterior spinal artery from nearby non-occluded segmental arteries. (Used with permission from: Martirosyan NL, Feuerstein JS, Theodore N, Cavalcanti DD, Spetzler RF, Preul MC. Blood supply and vascular reactivity of the spinal cord under normal and pathological conditions. J Neurosurg Spine 2011; 15: 238-51)48 and modified by our group to explain compensatory mechanisms within the spinal cord collateral vascular network and pathophysiology of spinal cord injury in TEVAR). TEVAR = thoracic endovascular aortic repair; ASA = anterior spinal artery; PSA = posterior spinal artery; a = artery
The concept of what constitutes the main blood supply to the spinal cord has evolved in recent years and has a direct impact on understanding the relationship between the blood supply of the spinal cord and SCI. In the past, there was widespread opinion that the single artery of Adamkiewicz was the most important contributor to the development of SCI after aortic aneurysm repair.20 Currently, however, there is growing experimental and clinical evidence to suggest that impairment in the collateral network of blood vessels in the spinal cord is more important to SCI than any single artery.3,21 This collateral network is an interconnected network of blood vessels between the anterior spinal artery (i.e., the intraspinous network) and the blood supply of the adjacent muscles of the back (i.e., the paraspinous network). There are also multilevel connections to the adjacent muscles within the intraspinous network— i.e., above and below any particular spinal cord segment. The arterial system of the spinal cord itself is divided into a central centrifugal system supplied by the sulcal arteries and a peripheral centripetal system supplied by the pial network surrounding the spinal cord.18 This interconnected network acts as an important alternate source of blood supply when a principal input is excluded, such as with segmental artery exclusion after thoracic stent deployment.3,21
Aortic cross-clamping during open TAAA repair results in proximal (to the clamp) hypertension, increased central venous pressure (CVP), increased intracranial pressure, and distal hypotension.22,23 The latter causes renal and/or intestinal ischemia as well as lower limb ischemia. The distal hypotension also directly impacts the blood supply to the spinal cord and reduces the spinal cord perfusion pressure, leading to ischemia.23,24,25 Additionally, after aortic unclamping, reperfusion can contribute to injury of the spinal cord through an associated inflammatory response.26 Reimplantation of the segmental arteries arising from the excised aortic aneurysmal sac has been suggested to reduce SCI. Nevertheless, there is considerable disagreement among vascular surgeons regarding the management of the segmental arteries in open TAAA repair. For example, many opt to reimplant all intercostal arteries into the aortic graft, while others choose either to reimplant only critical segmental arteries or not to reimplant at all.27
Because TEVAR does not involve the physiologic perturbations associated with aortic cross-clamping or the associated reperfusion injury to the spinal cord, this led to the expectation of significantly lower rates of paralysis. Nevertheless, TEVAR does permanently exclude many of the segmental arteries occluded by a covered thoracic stent, which may have longer-lasting effects on compromising spinal cord blood flow28 than relatively brief periods of aortic cross-clamping during open repair.
Immediate paralysis presents following open TAAA repair, whereas delayed paralysis is a more common presentation of SCI after TEVAR. A possible explanation for these differing clinical presentations is that the aortic cross-clamp-mediated spinal cord ischemia (and direct ligation of intercostal vessels) and reperfusion injury may further contribute to immediate ischemia. The fact that the aneurysm sac (with its intercostal tributaries) is left intact during TEVAR may contribute to the development of delayed SCI following the eventual cessation of stent endoleak. Nevertheless, there is a lack of evidence on the exact pathophysiologic differences.
With deployment of a covered stent during TEVAR, collateral network remodelling is thought to play an important role in maintaining spinal cord blood flow by changing the distribution of blood flow in the intraspinous and paraspinous collateral network after segmental artery exclusion.29 Rerouting of blood flow from the paraspinous to the intraspinous network helps to maintain spinal cord viability and function (Fig. 2). This is achieved by an enlargement in the diameter of the intraspinous network and a change in the orientation of the vessels of the paraspinous network from a relatively perpendicular orientation to an alignment parallel to the spinal cord. This results in a greater percentage of the mean aortic pressure being transmitted to the spinal cord. Etz et al. 29 described these changes in an experimental porcine model and showed that this remodelling occurs over the two to five days after surgery. In addition, Colman et al. 19 suggested that perfused non-occluded segmental arteries (either proximal or distal to the covering stent) can maintain blood flow to the ischemic spinal cord segment. This is achieved by reversing the direction of blood flow within the anterior spinal artery through either an antegrade direction from the proximal arteries or a retrograde direction from the distal segmental arteries. If all these compensatory mechanisms are insufficient or fail secondary to thrombus formation in the intraspinous or paraspinous network, embolism, or cessation of stent endoleak, spinal cord ischemia (i.e., frequently delayed) can occur (Fig. 2).30 The onset and severity of injury after TEVAR depends on the ability of the collateral network to supply the marginally vascularized area in the critical zone of the spinal cord known as the watershed area in the grey matter.21,28,31,32
Another emerging factor involved in the pathogenesis of SCI after TEVAR is atheroembolism from dislodgement of aortic plaque (due to manipulation of guidewires and stent deployment during the surgical procedure) occluding segmental vessels.33 Indeed, Zipfel et al. 34 described 11 patients with SCI in their cohort of 406 TEVAR patients and attributed the cause of paralysis in three of these patients to atheroembolism. This was established in one of these patients after analysis of the computed tomographic scan of the aorta revealed presence of a mobile atheroma. The other two patients had a circular thrombus at the distal landing site, in addition to the unilateral clinical presentation of their paralysis, which further supported atheroembolism as the cause of paralysis. Tanaka et al. 35 further examined the role of embolization in causing paralysis in 266 TEVAR patients, and they classified spinal cord magnetic resonance imaging (MRI) findings into three types: focal (asymmetrical focal high intensity on axial T2-weighted images involving two or fewer segments of the spinal cord), sporadic (asymmetrical multiple high intensity on axial T2-weighted images involving more than three segments of the spinal cord, shown on Fig. 3), and diffuse (symmetrical high intensity on axial T2-weighted images). In their series, based on microscopic examination of the anterior spinal artery and its branches from autopsy of four patients with SCI, they attributed sporadic and focal MRI findings to atheroembolism, while diffuse findings were attributed to hemodynamic instability.
Pattern of spinal cord damage in thoracic endovascular aortic repair on magnetic resonance imaging (sporadic-type findings): asymmetrical multiple high intensity on axial T2-weighted images involving more than three segments of vertebra. Infarction is shaded on the illustration. (Used with permission from: Tanaka H, Minatoya K, Matsuda H, et al. Embolism is emerging as a major cause of spinal cord injury after descending and thoracoabdominal aortic repair with a contemporary approach: magnetic resonance findings of spinal cord injury. Interact Cardiovasc Thorac Surg 2014; 19: 205-10).35
Risk factors for SCI after TEVAR
Multiple risk factors for the development of SCI after TEVAR have been identified and can be divided into patient and surgical procedure risk factors (Table 1). Patient risk factors include advanced age (> 70 years old),6 perioperative hypotension (e.g., mean arterial blood pressure < 70 mmHg),36,37,38 renal insufficiency (creatinine > 132 µMol·L−1),4,6,39 chronic obstructive pulmonary disease (COPD),6 hypertension,6 and degenerative aneurysms compared with non-aneurysm pathologies.40 Renal insufficiency has been postulated as a marker of widespread peripheral atherosclerotic disease, which suggests that such patients may preoperatively have a compromised collateral network of blood supply to the spinal cord. On the other hand, the exact underlying mechanism of COPD as a risk factor for SCI is not fully understood.
Surgical risk factors include increased urgency of the procedure,41 large extent of aortic coverage,6,38,42,43,44 left subclavian artery coverage,39 coverage of hypogastric arteries,36,40 the use of three or more stents,39 extended duration of the procedure,36 and increased blood loss.40 The extent of aortic coverage is a particularly important surgical risk factor.6,38,42,43,44 Indeed, after reviewing 326 TEVAR patients, Feezor et al.44 concluded that the risk of SCI is increased by 30% for every 2 cm of additional thoracic aortic coverage. Amabile et al. 43 showed that aortic coverage > 205 mm is associated with an increased risk of SCI, and that the length of the thoracic coverage distal to the celiac artery is also an important risk factor.
The vascular territories providing blood supply to the spinal cord are the left subclavian, intercostal, lumbar, and hypogastric territories. In a prospective observational single-centre study of 63 TEVAR patients, Czerny et al. 45 showed a direct correlation between coverage of two or more of these vascular territories (positive predictive value, 0.67; 95% confidence interval [CI], 0.24 to 0.91; P = 0.005) and development of symptomatic SCI, especially when combined with prolonged intraoperative hypotension. They also showed strong agreement between the derived results when they applied them to the data from the multicentre European Registry on Endovascular Aortic Repair Complications cohort.45 In addition, Martin et al. 46 retrospectively reviewed 261 TEVAR patients and reported that 18 of the 27 (67%) SCI patients in their cohort had a history of either repaired or unrepaired abdominal aortic aneurysm (AAA) (odds ratio [OR], 3.57; 95% CI, 1.56 to 8.33; P = 0.003). This finding has also been shown in other studies.38,39,47 The reason for the increased risk with prior repaired AAA is likely due to the compromise of the pelvic and hypogastric collateral blood supply to the spinal cord.
Role of the left subclavian artery in SCI
The left subclavian artery provides blood supply to the brain and spinal cord via the left vertebral artery. In doing so, it contributes to the blood supplying the posterior aspect of the circle of Willis via the basilar artery (formed by the union of the left and right vertebral arteries). The left vertebral artery also provides one of the two branches that feed the anterior spinal artery (Fig. 4).48 In addition, the thyrocervical trunk arising from the left subclavian artery supplies the cervical spinal cord through anterior and posterior radiculomedullary arteries (Fig. 4).49 More than 40% of patients undergoing TEVAR require intentional coverage of the left subclavian artery due to the close proximity of thoracic aortic pathology.50 Results of a meta-analysis by Rizvi et al. have shown that coverage of the left subclavian artery increases the risk of vertebrobasilar stroke and arm ischemia51 (OR, 10.8; CI, 3.2 to 36.7; I2 = 0% for stroke) and (OR, 47.7; CI, 9.9 to 229.3; I2 = 72% for arm ischemia). A more recent meta-analysis by Waterford et al. has shown similar results.52 They showed that the overall stroke rate after left subclavian coverage was higher when compared with TEVAR procedures performed distal to the subclavian origin (7.4% vs 4.0%, respectively; P < 0.0001).
Network of vascular collaterals to the spinal cord: subclavian, hypogastric, intercostal and lumbar arteries. (Used with permission from: Amato AC, Stolf NA. Anatomy of spinal blood supply. J Vasc Bras 2015; 14: 248-52)109
There are multiple surgical options to maintain flow within the left subclavian artery when its coverage is planned during TEVAR (Fig. 5). Revascularization procedures include either transposition of the subclavian to the left common carotid artery or inserting a short bypass graft between the left subclavian and the left common carotid artery. Nevertheless, these revascularization procedures themselves carry a 10-12% risk of complications, including brachial plexus, vagus nerve, left recurrent laryngeal nerve and thoracic duct injuries, neck hematoma, subclavian dissection, and stroke.53,54 Newer endovascular techniques for preserving subclavian blood flow include the use of fenestrated/branched stent grafts, chimney and periscope grafts, sandwich techniques, or in situ fenestration techniques.55 Fenestrated or branched stents are custom pre-made stents designed to allow perfusion of the left subclavian artery. Chimney grafts are inserted into the subclavian artery parallel to the proximal wall of the aortic stent (Fig. 6). The use of a periscope graft is another technical variation of the chimney graft, but it is inserted through the distal part of the aorta resembling an inverted chimney (Fig. 7). Sandwich grafts are inserted between two aortic stents to avoid problems associated with gutters of the chimney grafts (Fig. 8). This technique is used with visceral and iliac vessels, but it was recently introduced to the aortic arch revascularization. In situ fenestration involves intraoperative creation of a fenestration (using a laser)56 to perfuse the left subclavian artery after aortic stent deployment. Nevertheless, the main concern about this technique is the interruption of the nitinol ring by the laser and the resulting lack of support at the edge of the fenestration; it would also affect the quality and durability of the stent.55
Surgical options for left subclavian artery management during TEVAR. When the operative plan requires covering the origin of the left subclavian artery (LSA), the LSA can be left without revascularization or can be perfused through extra-anatomical surgical procedures or, more recently, by endovascular techniques. Surgical revascularization is done either routinely or only for selected patients. TEVAR = thoracic endovascular aortic repair
Chimney graft technique for left subclavian artery revascularization. A thoracic aortic endograft is excluding a descending thoracic aneurysm and covering the origin of the left subclavian artery (LSA); a chimney graft is inserted in the LSA parallel to the proximal wall of the aortic stent. The top left diagram shows a cross section of the aortic arch with the proximal end of the thoracic aortic stent and the LSA chimney graft in place. The middle left diagram shows a cross section of the aortic aneurysm with the thoracic stent excluding the aneurysaml sac. The bottom left diagram shows a cross section of the distal portion of the aortic stent sealing the descending thoracic aorta
Periscope graft for left subclavian artery revascularization. A thoracic aortic endograft is excluding a descending thoracic aneurysm and covering the origin of the left subclavian artery (LSA); a periscope graft is inserted in the LSA through the distal part of the aorta. The top left diagram shows a cross section of the aortic arch sealed with the proximal end of the aortic stent. The bottom left diagram shows a cross section of the descending thoracic aorta with the thoracic stent and LSA periscope graft in place
Periscope Sandwich technique for left subclavian artery revascularization. Two thoracic aortic endografts are excluding a descending thoracic aneurysm with the proximal stent covering the origin of the left subclavian artery (LSA); a sandwich graft is inserted between two aortic stents. The top left diagram shows a cross section of the aortic arch sealed with the proximal end of the aortic stent. The bottom left diagram shows a cross section of the overlapping thoracic stents with the distal end of the sandwich graft between them
The importance of routine preoperative subclavian revascularization has been debated, and some advocate performing such techniques only in selected high-risk patients. In the 2009 practice guidelines from the American Society of Vascular Surgery, routine preoperative left subclavian artery revascularization was suggested in elective TEVAR patients where subclavian coverage is anticipated to achieve a proximal seal. The guidelines also strongly recommended routine preoperative revascularization in selected patients with an anatomy that compromises perfusion to critical organs such as the brain and spinal cord.57 Rizvi et al. 51 performed a meta-analysis on 3,365 patients from 51 observational studies on the TEVAR procedure with or without left subclavian coverage. Results from eight of the studies showed a non-significant increase in the risk of SCI with left subclavian artery coverage (OR 2.69; 95% CI, 0.75 to 9.68; I2 = 40%). Recently, Patterson et al. 58 conducted a meta-analysis on 1,002 TEVAR patients from the Medtronic Thoracic Endovascular Registry (MOTHER) data derived from five clinical trials and one institutional series. The authors reported that subclavian coverage did not increase the risk of SCI (5%) compared with no such coverage (3%) (P = 0.16). They also showed a non-significant reduction in the incidence of SCI in patients who underwent left subclavian revascularization vs those who did not (4% vs 1.4%, respectively; P = 0.186). A more recent meta-analysis by Hajibandeh et al. 59 showed similar results on 1,161 patients from five observational studies. They did not show a significant difference in the rate of SCI between the subclavian revascularization and non-revascularization groups (2.7% vs 4.3%, respectively; P = 0.09). No updated guidelines regarding subclavian coverage have since been published.
Although debate continues on whether to perform routine preoperative subclavian revascularization, there are certain situations where selective revascularization is recommended.39,51,53,60,61,62,63,64,65 Indeed, most authors agree on certain absolute indications for preoperative revascularization, including prior left internal mammary artery coronary bypass, presence of a left-sided arteriovenous fistula for renal dialysis, and left-hand dominant patients. Relative indications include situations of dominant left vertebral artery, extensive aortic coverage, prior AAA repair, and occluded hypogastric artery. Postoperative indications include upper limb ischemia or vertebrobasilar insufficiency.51,53,66
Role of hypogastric arteries in SCI
The internal iliac artery (also known as the hypogastric artery) provides blood supply to the spinal cord via radicular lumbosacral arteries.48 Its sacrifice during open AAA repair or during endovascular aneurysm repair (EVAR) is a risk factor for SCI in TEVAR. During EVAR, for example, unilateral coil embolization of the hypogastric artery is done to allow the endograft to anchor in the healthy external iliac artery, preventing hypogastric artery endoleak into the aortoiliac aneurysm. This unilateral embolization does not usually lead to complications due to a rich pelvic arterial network. Nevertheless, bilateral occlusion is associated with an increased risk of pelvic ischemia. Manifestations of pelvic ischemia include buttock claudication, erectile dysfunction, and to a lesser extent, SCI.67
Further compromise of hypogastric blood flow can occur during TEVAR when an iliac artery graft is used to serve as a vascular access conduit in patients with severe atherosclerosis of the iliofemoral arteries. This has been associated with a higher risk of SCI. For instance, Khoynezhad et al. 40 reported eight of 153 (4.3%) TEVAR patients with SCI, and five of the eight SCI patients required an iliac conduit for the procedure.
Clinical presentation of SCI after TEVAR
The clinical manifestations of SCI after TEVAR vary between immediate (at emergence from anesthesia) and delayed onset (> 24 hr after surgery), with the majority of cases (66%) being delayed onset.10 Spinal cord injury is a dynamic process, and the clinical presentation varies between paresis of one limb to full paraplegia, with or without autonomic dysfunction. These manifestations may be either transient (with partial or full recovery) or permanent (with no regression).5,68 Mehmedagic et al. 69 conducted mid-term follow-up on 29 patients with inhospital transient neurological deficits and documented full recovery of these deficits before discharge. They reported a permanent, though less-severe form of SCI in a subset of these patients, which was overlooked, reflecting the importance of transient paresis on patient long-term quality of life.
Autonomic dysfunction
Three spinal cord elements are involved in cardiovascular function: the descending vasomotor pathways, sympathetic preganglionic neurons, and spinal afferents.70 Cardiovascular dysfunction is common after SCI. Once SCI occurs, it is understood that there is damage to the motor and sensory neurons as well as to the descending pathways that are involved in the autonomic control of the cardiovascular system. This can lead to hypotension and bradycardia (i.e., spinal shock).70,71 In a subset of their delayed paralysis patients, Cheung et al.72 showed that the recovery of neurological function was associated with a decrease in the required dose of vasopressors. This might be attributed to the recovery of the autonomic dysfunction associated with the resolution of the SCI. This explains that hypotension can not only exacerbate SCI but can also serve as a potential indicator of the early onset of SCI when the autonomic system is affected. The relationship between hypotension secondary to ischemic spinal cord autonomic dysfunction and paralysis in TEVAR affords a potential opportunity for further investigation.
Spinal cord monitoring during TEVAR
Monitoring spinal cord function during TEVAR can assist in detecting pathologically relevant changes in the functional integrity of neuronal pathways. Furthermore, it has the potential to direct clinicians to the need for intraoperative intervention. That said, few centres report performing intraoperative spinal cord neuromonitoring during TEVAR. In addition to the costs associated with the necessary equipment, its relatively low rate of use compared with open procedures can be attributed to the lack of aortic cross-clamping, the relatively short duration of the procedure, the requirement for expert interpretation, and the often delayed nature of paralysis. Despite evidence-based guidelines suggesting a benefit to intraoperative spinal cord monitoring in spine surgery,73 the role of neuromonitoring in TEVAR is still evolving. The latest American Heart Association guidelines suggest considering neurophysiological monitoring of the spinal cord during both open TAAA repair and TEVAR for prevention and/or treatment of SCI. Nevertheless, the level of evidence is only class IIb—i.e., usefulness or efficacy is less well established by evidence/opinion.7 Additional studies are needed to examine the full potential of neuromonitoring in the diagnosis and prevention of SCI and paralysis in TEVAR.
Motor- and sensory-evoked potentials
Motor-evoked potential (MEP) monitoring is used to evaluate the descending spinal pathways, while somatosensory-evoked potential (SSEP) monitoring evaluates the ascending pathways. Hence, they can be considered useful tools in the diagnosis and management of SCI during TEVAR.74 Weigang et al.74 reported loss or changes in the SSEP and MEP in 11/31 (35%) patients undergoing TEVAR. They described recovery of these changes in ten of the 11 (91%) patients after they intervened by increasing the blood pressure and draining CSF. Nevertheless, the remaining patient did not respond to these intraoperative interventions and, interestingly, did not have any postoperative neurological deficits (i.e., false positive). It is worth mentioning that they also reported that one patient with delayed paresis had intraoperative MEPs and SSEPs that were unchanged (i.e., false negative). Similarly, Schurink et al. 75 reported a > 50% reduction in MEPs in two of ten (20%) patients undergoing TEVAR. In those two patients with MEP reductions, the procedure was carried out in stages to minimize the risk of SCI by allowing sufficient time for the collateral blood supply network to adapt. One of the other eight patients without MEP changes had temporary right lower leg paresis. Recently, Banga et al.76 observed MEP and/or SSEP changes in 31/49 (63%) TEVAR patients. The changes were restored to baseline in 12 patients after intervention—i.e., CSF drainage and blood pressure elevation. After intervention and restoration of lower limb blood flow in 18 of their other patients, the overall rate of SCI was 6% (three patients). The intraoperative changes in evoked potentials could not be restored in the remaining patient who presented with immediate paralysis. The other two patients presented with delayed SCI.
Thus, the use of monitoring evoked potentials during TEVAR is useful in the detection of SCI. Nevertheless, if no interventions were performed, it is not clear if patients with observed evoked potentials would actually manifest with postoperative SCI. One limitation of monitoring evoked potentials is the inability to differentiate mild from severe SCI. In addition, the vascular access needed for the introduction of the stent during TEVAR may result in leg ischemia, limiting the use of SSEP and MEP monitoring from the ipsilateral leg.77 For these reasons, the current available literature does not appear to support its routine use.
Effect of anesthesia on evoked potentials
During general anesthesia, volatile anesthetics affect the cortical waveforms by increasing cortical latency and decreasing SSEP amplitude. Therefore, for practical purpose, volatile anesthetics should be kept at no more than half the minimum anesthetic concentration (MAC).78,79 Isoflurane at concentrations of 0.75 and 1.0 MAC produces good MEP responses in only 61% and 8% of the patients, respectively, after multipulse transcranial electrical stimulation.80,81,82 Similarly, sevoflurane at 0.5 and 0.75 MAC produces adequate responses in only 55% and 10% of the patients, respectively, when using dual-pulse electrical stimuli. Although propofol suppresses the alpha motor neuron in the grey matter of the spinal cord, serum concentrations at ≤ 1 μg·mL−1 generally allow a MEP response in most patients. In addition, opioids used at low dose in continuous infusions do not generally affect MEP responses. The use of neuromuscular blocking agents should be closely monitored to provide muscle relaxation and an adequate MEP response. Single twitch height (T1) of 20-50% of baseline can achieve this result. Thus, the preferable anesthetic protocol during evoked potential neuromonitoring should lean heavily towards total intravenous anesthesia (e.g., with propofol and remifentanil) with only low concentrations of volatile agents, if any.83
Near-infrared spectroscopy (NIRS)
The use of NIRS in TEVAR in an attempt to detect SCI was first reported in 2011.84 In this report, NIRS optodes were placed over the surface of the thoracic and lumbar paraspinous muscles of two patients. This procedure provided real-time measurement of blood oxygen saturation in the paraspinous collateral network, which shows a strong direct association with spinal cord microcirculation. After deployment of a thoracic aortic stent, the first patient showed a decrease in the spinal cord NIRS signal, which improved after augmenting MAP and draining CSF. The second patient developed SCI, which was consistent with the reduction in the NIRS signal that did not recover after any intervention. von Aspern et al. 85 used NIRS in seven juvenile pigs to compare measurements of paravertebral muscle oxygenation with direct measurements of the spinal cord oxygenation and microcirculatory flow by laser Doppler flowmetry. There was a significant positive correlation (r = 0.51 to 0.52; P < 0.001) between the measurements of both devices, and there was no significant difference between lumbar paraspinous muscle oxygenation and direct spinal cord oxygenation (P = 0.30). Thus, at least in theory, NIRS monitoring of the paraspinous muscles may indirectly reflect oxygenation in the spinal cord. Nevertheless, this technique has yet to be validated clinically.3,85,86
Spinal cord neuroprotective strategies in TEVAR
Spinal cord protection during TEVAR requires a team approach during the perioperative period, including input from the anesthesiologists, surgeons, and ICU team members. Anesthesiologists are responsible for optimizing spinal cord perfusion throughout the procedure. Surgeons have to make perioperative decisions regarding staging of the procedure and management of the left subclavian and hypogastric arteries. Other new surgical techniques of minimally invasive segmental artery coil embolization and TASP have also been introduced to minimize the risk of SCI (Table 2).
Perioperative anesthetic management
General measures
Important measures for spinal cord protection during TEVAR include ensuring adequate oxygenation and perfusion by maintaining a normal cardiac index and adequate hemoglobin—though the precise limits are not well defined.10,87 Nevertheless, it is important to determine the best method for increasing the cardiac index. The detrimental effects of increasing cardiac index through expansion of blood volume include a higher CVP (potentially detrimental to spinal cord blood flow, as discussed below) and tissue edema (including spinal cord tissues), while augmentation of cardiac output with adrenergic drugs may have potential negative effects at the microcirculatory level of the spinal cord.
Blood pressure management and spinal cord perfusion pressure
Spinal cord perfusion pressure is the difference between mean arterial blood pressure (MAP) and either CSF pressure or CVP, whichever is greater.31 General guidelines for minimizing SCI include increasing MAP (i.e., > 90 mmHg) and draining CSF (≤ 10 mmHg) in order to maintain spinal cord perfusion pressure at levels > 80 mmHg.8,74 Recently, the European Association for Cardiothoracic Surgeons published a position paper about spinal cord protection in TEVAR in which they recommended increasing blood pressure in patients with SCI to higher than the individual’s preoperative MAP—i.e., and at least 80 mmHg.8 Nevertheless, the strength of the provided evidence regarding blood pressure management and CSF drainage in the treatment of SCI is generally limited to expert opinion (i.e., level IIaC evidence) (Table 3).8
Izumi et al.88 described the effect of maintaining high MAP on spinal cord protection in a rabbit model of aortic cross-clamping by comparing high and low blood pressure animal groups with a control group. Mean (standard deviation) arterial blood pressure during ischemia was controlled at 121.9 (2.8), 50.8 (4.3), and 82.3 (10.7) mmHg in high blood pressure, low blood pressure, and control groups, respectively. They observed higher spinal cord blood flow, lower markers of oxidative stress, faster recovery of transcranial MEPs, and less histological damage of the motor neurons in the animal group treated with higher MAPs. In addition, in an experimental rat model of spinal cord ischemia/reperfusion, Lu et al. 89 showed that hypovolemia-induced hypotension led to more neurological dysfunction, more extensive neuronal necrosis, but less apoptotic neuronal death when compared with the normotensive control group. Although there is no direct experimental evidence on the effect of blood pressure management in endovascular repair for spinal cord protection, the clinical experience in the literature shows that maintaining spinal cord perfusion pressures > 80 mmHg (by increasing the MAP and draining the CSF) after the deployment of the aortic stent is beneficial in the prevention and management of SCI and paralysis. In patients who go on to develop postoperative SCI, a MAP > 90 mmHg should be targeted in an attempt to reverse the weakness. Vasopressors used to attain increased MAP goals should be weaned slowly over the subsequent 24–48 hr after improvement of the weakness. Such high levels of blood pressure are generally tolerated by TEVAR patients.10,87
Hypothermia
Mild passive hypothermia (32-35 °C) may have a role in neuroprotection of the spinal cord, though it has not been studied in a rigorous fashion.87,90 Unlike open TAAA surgical repair, moderate hypothermia is not a current practice in TEVAR as it generally requires a more invasive approach (e.g., intravascular cooling systems) in order to be induced for a minimally invasive surgery.91 Furthermore, evidence suggests that deeper levels of hypothermia affect the performance of nitinol-based endovascular grafts in vitro by decreasing the radial expansive force and thus the deployed diameter. This could have an important clinical impact on graft deformation, migration, and endoleak.92
Cerebrospinal fluid drainage
Indications for CSF drainage
In 2010, the American Heart Association/American College of Cardiology Foundation guidelines recommended CSF drainage for TAAA open and endovascular repair. Nevertheless, the document provided references only for the open repair.7 In addition, in 2015, the European Association for Cardiothoracic Surgeons recommended that CSF drainage should be considered in patients undergoing TEVAR for prevention and treatment of SCI, though with only level IIaC evidence (i.e., mostly expert opinion).8 In a randomized-controlled trial by Coselli et al. for open TAAA repair,93 they showed that CSF drainage significantly reduced the incidence of paraplegia/paraparesis [nine of 69 patients (13%) in the control group without CSF drainage vs two of 76 patients (2.6%) receiving CSF drainage; P = 0.03]. Similar high-quality data are not available for TEVAR. Hence, the indications and protocols for use of CSF drainage during TEVAR vary widely between institutions across the USA and around the globe.
Wong et al.11 recently conducted a systematic review involving 4,936 patients to address the issue of SCI and CSF drainage after TEVAR; however, they were unable to clarify the role of prophylactic CSF drainage due to the lack of randomized-controlled trials. Uchida also analyzed the literature from 1999 to 2013 on paraplegia/paraparesis after endovascular repair of thoracic aortic pathology. Based on his review, Uchida developed indications for CSF drainage in TEVAR; however, these indications need to be validated in prospective randomized-controlled trials (Table 3).14 In the absence of any pharmacological intervention to protect against SCI, physicians’ options are generally limited to CSF drainage and blood pressure management.
There has been recent debate on the value of introducing postoperative CSF drainage in those patients presenting with delayed paralysis. In fact, Kakinohana questioned the role of the CSF drain in the prevention of delayed paralysis after TEVAR and suggested that its use in this setting cannot be fully justified as the mechanism of the delayed paraplegia is not completely understood.10
Timing of the CSF drain placement
The timing of CSF drain placement also differs among institutions. Some groups recommend placement of the CSF drain the day before surgery so that any complications from drain placement, should they arise, can be recognized early.94 Other groups recommend insertion on the day of the surgery, in part to reduce hospital bed utilization and cost.90 DeSart et al. reviewed a cohort of 607 TEVAR patients where 57 (9.4%) developed some degree of SCI. Fifty-four (95%) of these received a CSF drain at some point in their care, and 31 (54%) received it postoperatively. They concluded that the timing of CSF placement did not have a major impact on post-discharge functional impairment or long-term mortality.5 Thus, the optimal timing of CSF drain placement remains uncertain.
In patients who go on to develop some degree of SCI, the window for the benefits of adding CSF drain placement to their therapy is also important as the reversal of any deficits likely closes within one to two hours of onset. Bobadilla et al. 90 performed a retrospective study of 94 TEVAR patients in whom they routinely inserted a CSF drain (both elective and emergent). In their series, only one patient suffered from delayed paralysis. Their proactive protocol reduced the time needed for interventions by allowing for immediate CSF drainage and induced hypertension as soon as paralysis was detected. This routine placement avoids the delay of CSF drain placement in patients with sudden onset of postoperative paralysis. An additional benefit to routine CSF drain placement includes increasing the efficacy of induced hypertension for the treatment of postoperative paralysis (to off-load CSF volume and reduce CSF pressure efficiently). Induced hypertension without the aid of a CSF drain has been speculated to be harmful due to potential formation of edema in the spinal cord.95
Another concern for postoperative drain insertion is the development of post-stent coagulopathy. The aortic stent excludes the aneurysmal sac from the blood flow, causing the blood inside the sac to thrombose. This consumes platelets and coagulation factors through activation of coagulation cascades (with reduction in fibrinogen and plasminogen levels as well as prothrombin activity) and fibrinolysis (with increases in fibrin degradation products and D-dimer levels). In studies by Shimazaki et al. 96 and Monaco et al.,97 these changes were shown on patients with endovascular thoracic aortic aneurysm and aortic dissection repair. Although both studies concluded that these changes do not affect patients’ outcome, anesthesiologists need to be aware of these mechanisms that may impact the safety of postoperative CSF drain insertion.
Notwithstanding the above potential coagulation issues, an alternate approach for timing CSF drain insertion is the “wait and see” methodology, which is much easier to employ in TEVAR (compared with open TAAA repair), as fast-track anesthetic techniques usually allow for early neurologic examination. That said, institutions that implement this approach must have standardized ICU procedures that employ structured and regular neurologic exams, including increased vigilance by the nurse/intensivist along with the avoidance of unnecessary sedation. Institutions should also have clinical infrastructure available to place a CSF drain rapidly if delayed SCI should occur. Acher et al. 2 reviewed 22 studies in the literature representing the current practice of CSF drainage in TEVAR. They concluded that, despite the wide variation in CSF drainage management among different institutions, rates of SCI remain in the range of 1-10%, whether the surgeon made the decision to insert the drain or institutional criteria defined the management protocol. In addition, timing of CSF drainage insertion (intraoperatively vs postoperatively) did not show differences in clinical outcomes.
Cerebrospinal fluid drain complications
Inherent in all invasive procedures (including CSF drain placement) are their associated complications. A number of studies have outlined the various CSF drain-related complications. Hanna et al.98 reported the complications of CSF drain placement in 81 TEVAR patients. Nine patients (11.1%) experienced minor lumbar drain complications, including spinal headache, bleeding at the puncture site, persistent CSF leak, or clinically insignificant subdural hematoma. On the other hand, Arnaoutakis et al.94 reported no complications from spinal drain placement in 48 patients. The reduction of complications in the Arnaoutakis et al. 94 series may have been due to the timing of catheter placement (24 hr prior to the TEVAR) as well as strict anticoagulation management around insertion and removal time. That is, they discontinued clopidogrel seven to ten days before the procedure and subcutaneous heparin 12 hr before drain insertion. The most recent American Society of Regional Anesthesia and Pain Medicine guidelines on insertion of intrathecal catheters recommend stopping clopidogrel at least seven days before the procedure, stopping intravenous heparin for at least four hours, and stopping subcutaneous heparin for eight to ten hours before the procedure. In individuals using acetylsalicylic acid (for secondary prophylaxis), the guidelines recommend weighing the risk of bleeding against the cardiovascular risks of stopping acetylsalicylic acid.99 The platelet threshold for drain insertion is recommended to be ≥ 100·103·µL−1, international normalized ratio < 1.3, and a normal activated partial thromboplastin time.100 In addition to the role of suboptimal coagulation status, clinically significant subdural hematoma can also be attributed to excessive CSF drainage—i.e., at rates > 15-20 mL·hr−1.100
In addition to concerns about CSF drain complications, some physicians think that CSF drainage prevents early mobilization, requires trained staff, and increases ICU length of stay for at least 48 hr (i.e., the recommended period for postoperative drainage). Zipfel et al.34 reported that 66% of their TEVAR patients did not require ICU care or required ICU care for < 24 hr. They were able to achieve this result because they did not use a CSF drain in their patients.
Newer surgical techniques for prevention of SCI
Several newer surgical techniques are now undergoing evaluation as adjuncts for the prevention of SCI. These include performing the procedure in stages, the use of MISACE, and allowing TASP (Table 2).101,102,103
Staging
In cases with planned coverage of a long segment (i.e., > 30 cm) of the aorta in extended thoracic and thoracoabdominal aneurysm, a two-stage operation can be considered to decrease the risk of SCI.14 Performing the aortic coverage in stages can be intentional or unintentional. Unintentional staging occurs in patients with a history of prior open or endovascular aortic aneurysm repair and presenting with an extension of their aneurysmal disease that requires TEVAR. Intentional staging repair involves initial placement of a thoracic aortic endograft covering the aorta from the proximal seal zone to just above the level of the most proximal visceral branch vessels. This procedure can then be followed by distal stent placement for distal seal after an interval of two to three months.101
Minimally invasive segmental artery coil embolization
Luehr et al. 104 individually embolized the segmental arteries in a porcine model through an endovascular technique known as minimally invasive segmental artery coil embolization (MISACE). Their experimental work showed that this technique essentially “preconditions” the collateral vascular network to ischemia by inducing arteriogenesis and improving vascularity of the spinal cord before TEVAR. Etz et al. 102 conducted a novel trial for this technique on two patients with a large thoracic aortic aneurysm. One patient underwent TEVAR while the other patient underwent open surgical repair. The segmental arteries were occluded 4–8 weeks before the aneurysm repair in both patients; neither of them developed SCI. Nevertheless, in an editorial accompanying this publication, the author questioned the reproducibility of this complex technique of endovascular embolization of the segmental arteries on a larger scale of patients, especially in patients with tortuous anatomy or with the presence of thrombus in the aneurysm sac.105
In 2017, A randomized-controlled clinical open-label trial is starting in 20 centres in Europe and in two centres in the USA for Paraplegia Prevention in Aortic Aneurysm Repair with MISACE (PAPA-ARTIS) (Project ID: 733203, as registered in the Community Research and Development Information Service). This trial should shed new light on how many segmental arteries need to be coiled in order to precondition the collateral network as well as on the ideal time interval between the MISACE procedure and TEVAR. Nevertheless, there are concerns regarding MISACE itself causing SCI, in addition to the concerns arising from artificially augmenting the blood pressure in a patient with an unrepaired aortic aneurysm to reverse emergent paralysis. Finally, it is highly speculative to translate the concept of arteriogenesis concluded from studies on juvenile large animals to humans with comorbid disease and advanced pathologies.
Temporary aneurysm sac perfusion (TASP)
The TASP surgical technique for prevention of SCI is performed by establishing an endoleak into the covered aneurysm with a branched endograft that has a side branch that will ultimately be used to perfuse a major splanchnic vessel during the first part of a staged procedure. This is followed by a second procedure after a one- to three-month interval to complete the exclusion of the endobranch (with a stent that bridges the TEVAR stent to the intended visceral vessel) feeding the aneurysm sac.103,106 Use of this technique showed a reduction in the rate of permanent paralysis. Kasprzak et al. 103 tested the feasibility of this technique in a prospective study on 83 TEVAR patients (40 patients with TASP vs 43 patients without TASP). The incidence of SCI was significantly reduced in the TASP group (5% vs 21%, respectively; P = 0.03). Nevertheless, the incidence of subsequent endoleak, potential risk of aortic rupture (occurring in the time between the two stages), and higher rate of temporary paraparesis and paresthesia (30%) (as reported by Kasprzak et al.)103 necessitate further investigation of this technique.
Implantation sequence rearrangement for branched/fenestrated stents
The final step in the insertion of branched/fenestrated stents is implantation of the bifurcated body and iliac limbs through large sheaths connected to the femoral/iliac arteries. These sheaths block the blood flow to the pelvis and lower limbs and subsequently the collateral circulation to the spinal cord. Some groups have recently changed their implantation sequence by implanting the bifurcated body and iliac limbs and then withdrawing these large sheaths earlier in the procedure, after deployment of the central stent. This is done in order to restore the blood flow to the femoral and iliac arteries and, hence, to reduce the incidence of SCI.107,108
Conclusion
Spinal cord injury and paralysis continue to be challenging complications after TEVAR. The incidence of SCI after TEVAR remains relatively high despite recent advances in surgical techniques. Anesthesiologists have a major role in spinal cord protection by careful management of the hemodynamics and institution of protocols for CSF drainage. Newer surgical techniques (i.e., MISACE and TASP) are currently under investigation in an attempt to reduce this dreadful complication. Further preclinical and clinical research is needed to discover novel neuroprotective strategies for protection and treatment of SCI and paralysis following TEVAR.
References
Frederick JR, Woo YJ. Thoracoabdominal aortic aneurysm. Ann Cardiothorac Surg 2012; 1: 277-85.
Acher C, Acher CW, Marks E, Wynn M. Intraoperative neuroprotective interventions prevent spinal cord ischemia and injury in thoracic endovascular aortic repair. J Vasc Surg 2016; 63: 1458-65.
Etz DC, Luehr M, Aspern KV, et al. Spinal cord ischemia in open and endovascular thoracoabdominal aortic aneurysm repair: new concepts. J Cardiovasc Surg (Torino) 2014; 55(2 Suppl 1): 159-68.
Ullery BW, Cheung AT, Fairman RM, et al. Risk factors, outcomes, and clinical manifestations of spinal cord ischemia following thoracic endovascular aortic repair. J Vasc Surg 2011; 54: 677-84.
DeSart K, Scali ST, Feezor RJ, et al. Fate of patients with spinal cord ischemia complicating thoracic endovascular aortic repair. J Vasc Surg 2013; 58: 635-42.
Scali ST, Wang SK, Feezor RJ, et al. Preoperative prediction of spinal cord ischemia after thoracic endovascular aortic repair. J Vasc Surg 2014; 60: 1481-90.
Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010; 121: e266-369.
Etz CD, Weigang E, Hartert M, et al. Contemporary spinal cord protection during thoracic and thoracoabdominal aortic surgery and endovascular aortic repair: a position paper of the vascular domain of the European Association for Cardio-Thoracic Surgery. Eur Cardiothorac Surg 2015; 47: 943-57.
Khan NR, Smalley Z, Nesvick CL, Lee SL, Michael LM 2nd. The use of lumbar drains in preventing spinal cord injury following thoracoabdominal aortic aneurysm repair: an updated systematic review and meta-analysis. J Neurosurg Spine 2016; 25: 383-93.
Kakinohana M. What should we do against delayed onset paraplegia following TEVAR? J Anesth 2014; 28: 1-3.
Wong CS, Healy D, Canning C, Coffey JC, Boyle JR, Walsh SR. A systematic review of spinal cord injury and cerebrospinal fluid drainage after thoracic aortic endografting. J Vasc Surg 2012; 56: 1438-47.
Andrassy J, Weidenhagen R, Meimarakis G, Rentsch M, Jauch KW, Kopp R. Endovascular versus open treatment of degenerative aneurysms of the descending thoracic aorta: a single center experience. Vascular 2011; 19: 8-14.
Bicknell C, Powell JT. Aortic disease: thoracic endovascular aortic repair. Heart 2015; 101: 586-91.
Uchida N. How to prevent spinal cord injury during endovascular repair of thoracic aortic disease. Gen Thorac Cardiovasc Surg 2014; 62: 391-7.
Greenberg RK, Lu Q, Roselli EE, et al. Contemporary analysis of descending thoracic and thoracoabdominal aneurysm repair: a comparison of endovascular and open techniques. Circulation 2008; 118: 808-17.
Maeda T, Yoshitani K, Sato S, et al. Spinal cord ischemia after endovascular aortic repair versus open surgical repair for descending thoracic and thoracoabdominal aortic aneurism. J Anesth 2012; 26: 805-11.
Doppman JL. Paraplegia after surgery for thoracoabdominal aneurysms: Russian roulette for the vascular surgeon. Radiology 1993; 189: 27-8.
Melissano G, Bertoglio L, Rinaldi E, Leopardi M, Chiesa R. An anatomical review of spinal cord blood supply. J Cardiovasc Surg (Torino) 2015; 56: 699-706.
Colman MW, Hornicek FJ, Schwab JH. Spinal cord blood supply and its surgical implications. J Am Acad Orthop Surg 2015; 23: 581-91.
Mehrez IO, Nabseth DC, Hogan EL, Deterling RA Jr. Paraplegia following resection of abdominal aortic aneurysm. Ann Surg 1962; 156: 890-8.
Griepp RB, Griepp EB. Spinal cord protection in surgical and endovascular repair of thoracoabdominal aortic disease. J Thorac Cardiovasc Surg 2015; 149(2 Suppl): S86-90.
D’Ambra MN, Dewhirst W, Jacobs M, Bergus B, Borges L, Hilgenberg A. Cross-clamping the thoracic aorta. Effect on intracranial pressure. Circulation 1988; 78(5 Pt 2): III198-202.
Gelman S. The pathophysiology of aortic cross-clamping and unclamping. Anesthesiology 1995; 82: 1026-60.
Marini CP, Levison J, Caliendo F, Nathan IM, Cohen JR. Control of proximal hypertension during aortic cross-clamping: its effect on cerebrospinal fluid dynamics and spinal cord perfusion pressure. Semin Thorac Cardiovasc Surg 1998; 10: 51-6.
Wynn MM, Acher CW. A modern theory of spinal cord ischemia/injury in thoracoabdominal aortic surgery and its implications for prevention of paralysis. J Cardiothorac Vasc Anesth 2014; 28: 1088-99.
Zhu P, Li JX, Fujino M, Zhuang J, Li XK. Development and treatments of inflammatory cells and cytokines in spinal cord ischemia-reperfusion injury. Mediators Inflamm 2013; 2013: 701970.
David N, Roux N, Douvrin F, Clavier E, Bessou JP, Plissonnier D. Aortic aneurysm surgery: long-term patency of the reimplanted intercostal arteries. Ann Vasc Surg 2012; 26: 839-44.
Davidovic L, Ilic N. Spinal cord ischemia after aortic surgery. J Cardiovasc Surg (Torino) 2014; 55: 741-57.
Etz CD, Kari FA, Mueller CS, et al. The collateral network concept: a reassessment of the anatomy of spinal cord perfusion. J Thorac Cardiovasc Surg 2011; 141: 1020-8.
Stokum JA, Gerzanich V, Simard JM. Molecular pathophysiology of cerebral edema. J Cereb Blood Flow Metab 2016; 36: 513-38.
Carroccio A, Marin ML, Ellozy S, Hollier LH. Pathophysiology of paraplegia following endovascular thoracic aortic aneurysm repair. J Card Surg 2003; 18: 359-66.
Turnbull IM. Microvasculature of the human spinal cord. J Neurosurg 1971; 35: 141-7.
Griepp RB, Griepp EB. Spinal cord perfusion and protection during descending thoracic and thoracoabdominal aortic surgery: the collateral network concept. Ann Thorac Surg 2007; 83: S865-9 (discussion S890-2).
Zipfel B, Buz S, Redlin M, et al. Spinal cord ischemia after thoracic stent-grafting: causes apart from intercostal artery coverage. Ann Thorac Surg 2013; 96: 31-8.
Tanaka H, Minatoya K, Matsuda H, et al. Embolism is emerging as a major cause of spinal cord injury after descending and thoracoabdominal aortic repair with a contemporary approach: magnetic resonance findings of spinal cord injury. Interact Cardiovasc Thorac Surg 2014; 19: 205-10.
Chang CK, Chuter TA, Reilly LM, et al. Spinal arterial anatomy and risk factors for lower extremity weakness following endovascular thoracoabdominal aortic aneurysm repair with branched stent-grafts. J Endovasc Ther 2008; 15: 356-62.
Chiesa R, Melissano G, Marrocco-Trischitta MM, Civilini E, Setacci F. Spinal cord ischemia after elective stent-graft repair of the thoracic aorta. J Vasc Surg 2005; 42: 11-7.
Gravereaux EC, Faries PL, Burks JA, et al. Risk of spinal cord ischemia after endograft repair of thoracic aortic aneurysms. J Vasc Surg 2001; 34: 997-1003.
Buth J, Harris PL, Hobo R, et al. Neurologic complications associated with endovascular repair of thoracic aortic pathology: incidence and risk factors. a study from the European Collaborators on Stent/Graft Techniques for Aortic Aneurysm Repair (EUROSTAR) registry. J Vasc Surg 2007; 46: 1103-10 (discussion 1110-1).
Khoynezhad A, Donayre CE, Bui H, Kopchok GE, Walot I, White RA. Risk factors of neurologic deficit after thoracic aortic endografting. Ann Thorac Surg 2007; 83: S882-9 (discussion S890-2).
Knowles M, Murphy EH, Dimaio JM, et al. The effects of operative indication and urgency of intervention on patient outcomes after thoracic aortic endografting. J Vasc Surg 2011; 53: 926-34.
Bisdas T, Panuccio G, Sugimoto M, Torsello G, Austermann M. Risk factors for spinal cord ischemia after endovascular repair of thoracoabdominal aortic aneurysms. J Vasc Surg 2015; 61: 1408-16.
Amabile P, Grisoli D, Giorgi R, Bartoli JM, Piquet P. Incidence and determinants of spinal cord ischaemia in stent-graft repair of the thoracic aorta. Eur J Vasc Endovasc Surg 2008; 35: 455-61.
Feezor RJ, Martin TD, Hess PJ Jr, et al. Extent of aortic coverage and incidence of spinal cord ischemia after thoracic endovascular aneurysm repair. Ann Thorac Surg 2008; 86: 1809-14 (discussion 1814).
Czerny M, Eggebrecht H, Sodeck G, et al. Mechanisms of symptomatic spinal cord ischemia after TEVAR: insights from the European Registry of Endovascular Aortic Repair Complications (EuREC). J Endovasc Ther 2012; 19: 37-43.
Martin DJ, Martin TD, Hess PJ, Daniels MJ, Feezor RJ, Lee WA. Spinal cord ischemia after TEVAR in patients with abdominal aortic aneurysms. J Vasc Surg 2009; 49: 302-6 (discussion 306-7).
Schlosser FJ, Verhagen HJ, Lin PH, et al. TEVAR following prior abdominal aortic aneurysm surgery: increased risk of neurological deficit. J Vasc Surg 2009; 49: 308-14 (discussion 314).
Martirosyan NL, Feuerstein JS, Theodore N, Cavalcanti DD, Spetzler RF, Preul MC. Blood supply and vascular reactivity of the spinal cord under normal and pathological conditions. J Neurosurg Spine 2011; 15: 238-51.
Hoehmann CL, Hitscherich K, Cuoco JA. The artery of Adamkiewicz: vascular anatomy, clinical significance and surgical considerations. Int J Cardiovasc Res 2016; 5: 6.
Peterson BG, Eskandari MK, Gleason TG, Morasch MD. Utility of left subclavian artery revascularization in association with endoluminal repair of acute and chronic thoracic aortic pathology. J Vasc Surg 2006; 43: 433-9.
Rizvi AZ, Murad MH, Fairman RM, Erwin PJ, Montori VM. The effect of left subclavian artery coverage on morbidity and mortality in patients undergoing endovascular thoracic aortic interventions: a systematic review and meta-analysis. J Vasc Surg 2009; 50: 1159-69.
Waterford SD, Chou D, Bombien R, Uzun I, Shah A, Khoynezhad A. Left subclavian arterial coverage and stroke during thoracic aortic endografting: a systematic review. Ann Thorac Surg 2016; 101: 381-9.
Garg K, Maldonado TS. Further consideration for subclavian revascularization with TEVAR. Semin Vasc Surg 2012; 25: 232-7.
Saouti N, Hindori V, Morshuis WJ, Heijmen RH. Left subclavian artery revascularization as part of thoracic stent grafting. Eur J Cardiothorac Surg 2015; 47: 120-5 (discussion 125).
Dias N, Sonesson B. Revascularization options for left subclavian salvage during TEVAR. J Cardiovasc Surg (Torino) 2014; 55: 497-503.
Redlinger RE Jr, Ahanchi SS, Panneton JM. In situ laser fenestration during emergent thoracic endovascular aortic repair is an effective method for left subclavian artery revascularization. J Vasc Surg 2013; 58: 1171-7.
Matsumura JS, Lee WA, Mitchell RS, et al. The Society for Vascular Surgery Practice Guidelines: management of the left subclavian artery with thoracic endovascular aortic repair. J Vasc Surg 2009; 50: 1155-8.
Patterson BO, Holt PJ, Nienaber C, Fairman RM, Heijmen RH, Thompson MM. Management of the left subclavian artery and neurologic complications after thoracic endovascular aortic repair. J Vasc Surg 2014; 60: 1491-7.
Hajibandeh S, Hajibandeh S, Antoniou SA, Torella F, Antoniou GA. Meta-analysis of left subclavian artery coverage with and without revascularization in thoracic endovascular aortic repair. J Endovasc Ther 2016; 23: 634-41.
Cooper DG, Walsh SR, Sadat U, Noorani A, Hayes PD, Boyle JR. Neurological complications after left subclavian artery coverage during thoracic endovascular aortic repair: a systematic review and meta-analysis. J Vasc Surg 2009; 49: 1594-601.
Kotelis D, Geisbusch P, Hinz U, et al. Short and midterm results after left subclavian artery coverage during endovascular repair of the thoracic aorta. J Vasc Surg 2009; 50: 1285-92.
Maldonado TS, Dexter D, Rockman CB, et al. Left subclavian artery coverage during thoracic endovascular aortic aneurysm repair does not mandate revascularization. J Vasc Surg 2013; 57: 116-24.
Wilson JE, Galinanes EL, Hu P, Dombrovskiy VY, Vogel TR. Routine revascularization is unnecessary in the majority of patients requiring zone II coverage during thoracic endovascular aortic repair: a longitudinal outcomes study using United States Medicare population data. Vascular 2014; 22: 239-45.
Woo EY, Carpenter JP, Jackson BM, et al. Left subclavian artery coverage during thoracic endovascular aortic repair: a single-center experience. J Vasc Surg 2008; 48: 555-60.
Lee TC, Andersen ND, Williams JB, Bhattcharya SD, McCann RL, Hughes GC. Results with a selective revascularization strategy for left subclavian artery coverage during thoracic endovascular aortic repair. Ann Thorac Surg 2011; 92: 97-102 (discussion 102-3).
Riambau V, Capoccia L, Mestres G, Matute P. Spinal cord protection and related complications in endovascular management of B dissection: LSA revascularization and CSF drainage. Ann Cardiothorac Surg 2014; 3: 336-8.
Lin PH, Chen AY, Vij A. Hypogastric artery preservation during endovascular aortic aneurysm repair: is it important? Semin Vasc Surg 2009; 22: 193-200.
Mehmedagic I, Resch T, Acosta S. Complications to cerebrospinal fluid drainage and predictors of spinal cord ischemia in patients with aortic disease undergoing advanced endovascular therapy. Vasc Endovasc Surg 2013; 47: 415-22.
Mehmedagic I, Jorgensen S, Acosta S. Mid-term follow-up of patients with permanent sequel due to spinal cord ischemia after advanced endovascular therapy for extensive aortic disease. Spinal Cord 2014. DOI:10.1038/sc.2014.163.
Furlan JC, Fehlings MG, Shannon P, Norenberg MD, Krassioukov AV. Descending vasomotor pathways in humans: correlation between axonal preservation and cardiovascular dysfunction after spinal cord injury. J Neurotrauma 2003; 20: 1351-63.
Mathias CJ, Low DA, Frankel HL. Autonomic disturbances in spinal cord lesions. In: Mathias CJ, Bannister R (Eds). Autonomic Failure: A Textbook of Clinical Disorders of the Autonomic Nervous System. Oxford, UK: Oxford University Press; 2013.
Cheung AT, Weiss SJ, McGarvey ML, et al. Interventions for reversing delayed-onset postoperative paraplegia after thoracic aortic reconstruction. Ann Thorac Surg 2002; 74: 413-9 (discussion 420-1).
Nuwer MR, Emerson RG, Galloway G, et al. Evidence-based guideline update: intraoperative spinal monitoring with somatosensory and transcranial electrical motor evoked potentials. J Clin Neurophysiol 2012; 29: 101-8.
Weigang E, Hartert M, Siegenthaler MP, et al. Perioperative management to improve neurologic outcome in thoracic or thoracoabdominal aortic stent-grafting. Ann Thorac Surg 2006; 82: 1679-87.
Schurink GW, De Haan MW, Peppelenbosch AG, Mess W, Jacobs MJ. Spinal cord function monitoring during endovascular treatment of thoracoabdominal aneurysms: implications for staged procedures. J Cardiovasc Surg (Torino) 2013; 54: 117-24.
Banga PV, Oderich GS, Reis de Souza L, et al. Neuromonitoring, cerebrospinal fluid drainage, and selective use of iliofemoral conduits to minimize risk of spinal cord injury during complex endovascular aortic repair. J Endovasc Ther 2016; 23: 139-49.
Sloan TB, Edmonds HL Jr, Koht A. Intraoperative electrophysiologic monitoring in aortic surgery. J Cardiothorac Vasc Anesth 2013; 27: 1364-73.
Haghighi SS, Sirintrapun SJ, Johnson JC, Keller BP, Oro JJ. Suppression of spinal and cortical somatosensory evoked potentials by desflurane anesthesia. J Neurosurg Anesthesiol 1996; 8: 148-53.
Malcharek MJ, Loeffler S, Schiefer D, et al. Transcranial motor evoked potentials during anesthesia with desflurane versus propofol–a prospective randomized trial. Clin Neurophysiol 2015; 126: 1825-32.
Pelosi L, Stevenson M, Hobbs GJ, Jardine A, Webb JK. Intraoperative motor evoked potentials to transcranial electrical stimulation during two anaesthetic regimens. Clin Neurophysiol 2001; 112: 1076-87.
Pechstein U, Nadstawek J, Zentner J, Schramm J. Isoflurane plus nitrous oxide versus propofol for recording of motor evoked potentials after high frequency repetitive electrical stimulation. Electroencephalogr Clin Neurophysiol 1998; 108: 175-81.
Lotto ML, Banoub M, Schubert A. Effects of anesthetic agents and physiologic changes on intraoperative motor evoked potentials. J Neurosurg Anesthesiol 2004; 16: 32-42.
Husain AM, Swaminathan M, McCann RL, Hughes GC. Neurophysiologic intraoperative monitoring during endovascular stent graft repair of the descending thoracic aorta. J Clin Neurophysiol 2007; 24: 328-35.
Badner NH, Nicolaou G, Clarke CF, Forbes TL. Use of spinal near-infrared spectroscopy for monitoring spinal cord perfusion during endovascular thoracic aortic repairs. J Cardiothorac Vasc Anesth 2011; 25: 316-9.
von Aspern K, Haunschild J, Hoyer A, et al. Non-invasive spinal cord oxygenation monitoring: validating collateral network near-infrared spectroscopy for thoracoabdominal aortic aneurysm repair. Eur J Cardiothorac Surg 2016; 50: 675-83.
Kari FA, Czerny M. Spinal near-infrared spectroscopy monitoring in aortic surgery: the beginning of understanding it or already clinical routine? Eur J Cardiothorac Surg 2016; 50: 683-4.
Ullery BW, Wang GJ, Low D, Cheung AT. Neurological complications of thoracic endovascular aortic repair. Semin Cardiothorac Vasc Anesth 2011; 15: 123-40.
Izumi S, Okada K, Hasegawa T, et al. Augmentation of systemic blood pressure during spinal cord ischemia to prevent postoperative paraplegia after aortic surgery in a rabbit model. J Thorac Cardiovasc Surg 2010; 139: 1261-8.
Lu K, Liang CL, Chen HJ, et al. Injury severity and cell death mechanisms: effects of concomitant hypovolemic hypotension on spinal cord ischemia-reperfusion in rats. Exp Neurol 2004; 185: 120-32.
Bobadilla JL, Wynn M, Tefera G, Acher CW. Low incidence of paraplegia after thoracic endovascular aneurysm repair with proactive spinal cord protective protocols. J Vasc Surg 2013; 57: 1537-42.
Kulik A, Castner CF, Kouchoukos NT. Outcomes after thoracoabdominal aortic aneurysm repair with hypothermic circulatory arrest. J Thorac Cardiovasc Surg 2011; 141: 953-60.
Robich MP, Hagberg R, Schermerhorn ML, et al. Hypothermia severely effects performance of nitinol-based endovascular grafts in vitro. Ann Thorac Surg 2012; 93: 1223-7.
Coselli JS, LeMaire SA, Koksoy C, Schmittling ZC, Curling PE. Cerebrospinal fluid drainage reduces paraplegia after thoracoabdominal aortic aneurysm repair: results of a randomized clinical trial. J Vasc Surg 2002; 35: 631-9.
Arnaoutakis DJ, Arnaoutakis GJ, Beaulieu RJ, Abularrage CJ, Lum YW, Black JH 3rd. Results of adjunctive spinal drainage and/or left subclavian artery bypass in thoracic endovascular aortic repair. Ann Vasc Surg 2014; 28: 65-73.
Pokhrel B, Hasegawa T, Izumi S, et al. Excessively high systemic blood pressure in the early phase of reperfusion exacerbates early-onset paraplegia in rabbit aortic surgery. J Thorac Cardiovasc Surg 2010; 140: 400-7.
Shimazaki T, Ishimaru S, Kawaguchi S, Yokoi Y, Watanabe Y. Blood coagulation and fibrinolytic response after endovascular stent grafting of thoracic aorta. J Vasc Surg 2003; 37: 1213-8.
Monaco M, Di Tommaso L, Stassano P, et al. Impact of blood coagulation and fibrinolytic system changes on early and mid term clinical outcome in patients undergoing stent endografting surgery. Interact Cardiovasc Thorac Surg 2006; 5: 724-8.
Hanna JM, Andersen ND, Aziz H, Shah AA, McCann RL, Hughes GC. Results with selective preoperative lumbar drain placement for thoracic endovascular aortic repair. Ann Thorac Surg 2013; 95: 1968-74 (discussion 1974-5).
Narouze S, Benzon HT, Provenzano DA, et al. Interventional spine and pain procedures in patients on antiplatelet and anticoagulant medications: guidelines from the American Society of Regional Anesthesia and Pain Medicine, the European Society of Regional Anaesthesia and Pain Therapy, the American Academy of Pain Medicine, the International Neuromodulation Society, the North American Neuromodulation Society, and the World Institute of Pain. Reg Anesth Pain Med 2015; 40: 182-212.
Fedorow CA, Moon MC, Mutch WA, Grocott HP. Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: rationale and practical considerations for management. Anesth Analg 2010; 111: 46-58.
O’Callaghan A, Mastracci TM, Eagleton MJ. Staged endovascular repair of thoracoabdominal aortic aneurysms limits incidence and severity of spinal cord ischemia. J Vasc Surg 2015; 61: 347-54.
Etz CD, Debus ES, Mohr FW, Kolbel T. First-in-man endovascular preconditioning of the paraspinal collateral network by segmental artery coil embolization to prevent ischemic spinal cord injury. J Thorac Cardiovasc Surg 2015; 149: 1074-9.
Kasprzak PM, Gallis K, Cucuruz B, Pfister K, Janotta M, Kopp R. Editor’s choice–Temporary aneurysm sac perfusion as an adjunct for prevention of spinal cord ischemia after branched endovascular repair of thoracoabdominal aneurysms. Eur J Vasc Endovasc Surg 2014; 48: 258-65.
Luehr M, Salameh A, Haunschild J, et al. Minimally invasive segmental artery coil embolization for preconditioning of the spinal cord collateral network before one-stage descending and thoracoabdominal aneurysm repair. Innovations (Phila) 2014; 9: 60-5.
Wheatley GH 3rd. Setting the stage: thoracoabdominal aortic aneurysm repair in 2 acts. J Thorac Cardiovasc Surg 2015; 149: 1079-80.
Reilly LM, Chuter TA. Reversal of fortune: induced endoleak to resolve neurological deficit after endovascular repair of thoracoabdominal aortic aneurysm. J Endovasc Ther 2010; 17: 21-9.
Maurel B, Delclaux N, Sobocinski J, et al. The impact of early pelvic and lower limb reperfusion and attentive peri-operative management on the incidence of spinal cord ischemia during thoracoabdominal aortic aneurysm endovascular repair. Eur J Vasc Endovasc Surg 2015; 49: 248-54.
Verhoeven EL, Katsargyris A, Bekkema F, et al. Editor’s choice–Ten-year experience with endovascular repair of thoracoabdominal aortic aneurysms: results from 166 consecutive patients. Eur J Vasc Endovasc Surg 2015; 49: 524-31.
Amato AC, Stolf NA. Anatomy of spinal blood supply. J Vasc Bras 2015; 14: 248-52.
Acknowledgements
Esmerina Tili and Hamdy Awad are supported by the NIH R03 NS102861-01 grant.
Conflicts of interest
None declared.
Editorial responsibility
This submission is handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Hamdy Awad, Mohamed Ehab Ramadan, and Esmerina Tili conceived the idea and personally collected and interpreted the data in the literature. Mohamed Ehab Ramadan, Hosam F. El Sayed, and Esmerina Tili created the figures. Daniel A. Tolpin and Charles D. Collard reviewed, edited, and added the data in the manuscript. All authors helped in preparation of the manuscript and attest to the integrity of the original data and the analysis reported in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Awad, H., Ramadan, M.E., El Sayed, H.F. et al. Spinal cord injury after thoracic endovascular aortic aneurysm repair. Can J Anesth/J Can Anesth 64, 1218–1235 (2017). https://doi.org/10.1007/s12630-017-0974-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-017-0974-1