Abstract
Purpose
The purpose of the Canadian Anesthesia Research Priority Setting Partnership (CAR PSP) was to identify a top ten list of shared priorities for research in anesthesia and perioperative care in Canada.
Methods
We used the methods of the James Lind Alliance to involve patients, caregivers, healthcare professionals, and researchers in determining the research priorities in Canada. In a first survey, participants submitted questions that they want research to answer about anesthesia and perioperative care. We summarized those responses into a longlist of questions. We reviewed the literature to see if any of those questions were already answered. In a second survey, participants chose up to ten questions from the longlist that they thought were most important to be answered with research. From that list, the highest ranking questions were discussed and assigned a final rank at an in-person workshop.
Results
A total of 254 participants submitted 574 research suggestions that were then summarized into 49 questions. Those questions were checked against the literature to be sure they were not already adequately addressed, and in a second survey of those 49 questions, participants chose up to 10 that they thought were most important. A total of 233 participants submitted their priorities, which were then used to choose 24 questions for discussion at the final workshop. At the final workshop, 22 participants agreed on a top ten list of priorities.
Conclusion
The CAR PSP top ten priorities reflect a wide variety of priorities captured by a broad spectrum of Canadians who receive and provide anesthesia care. The priorities are a tool to initiate and guide patient-oriented research in anesthesia and perioperative care.
Résumé
Objectif
L’objectif du Partenariat canadien pour l’établissement des priorités de la recherche en anesthésie (CAR-PSP) était d’établir une liste des dix principales priorités pour la recherche sur les soins anesthésiques et périopératoires au Canada.
Méthodes
Nous avons utilisé la méthodologie de la James Lind Alliance pour impliquer des patients, des aidants, des professionnels de la santé et des chercheurs afin de déterminer quelles étaient les priorités en matière de recherche au Canada. Dans une première enquête, les participants ont envoyé des questions sur les soins anesthésiques et périopératoires auxquelles ils voulaient que la recherche réponde. Nous avons résumé ces envois par une liste exhaustive de questions. Nous avons passé en revue les publications pour voir s’il existait déjà des réponses à ces questions. Dans une deuxième étude, les participants ont choisi dans la liste jusqu’à dix questions qui leur semblaient les plus importantes et pour lesquelles la recherche devrait fournir des réponses. À partir de cette liste, les questions les mieux classées ont été discutées et un classement définitif leur a été attribué au cours d’un atelier où tous les participants étaient présents en personne.
Résultats
Au total, 254 participants ont envoyé 574 suggestions de recherche qui ont été résumées en 49 questions. La littérature a été examinée pour s’assurer que ces questions n’avaient pas déjà reçu des réponses adéquates, et dans une seconde étude, les participants ont choisi jusqu’à 10 questions qu’ils jugeaient les plus importantes parmi ces 49 questions. Au total, 233 participants ont communiqué leurs priorités qui ont alors servi à choisir 24 questions ouvertes pour la discussion dans un atelier final. Dans cet atelier, 22 participants se sont mis d’accord sur une liste des dix principales priorités.
Conclusion
Les dix principales priorités du CAR-PSP sont le reflet d’un grand éventail de priorités venant de Canadiens de tous horizons qui reçoivent ou fournissent des soins d’anesthésie. Ces priorités sont un outil permettant d’entamer et de guider une recherche axée sur le patient dans le domaine des soins anesthésiques et périopératoires.
Similar content being viewed by others
Current research in anesthesia and perioperative care has focused on studies to better understand physiology and applied pharmacology as well as to assess safety or postoperative pain relief. Such studies advance knowledge about anesthesia and perioperative practice but may not provide readily translatable meaningful answers to relevant patient-centred questions.1,2
Funding sources, vested researcher interests, publication pressure, and consumer interests are all potential contributors to influencing the research agenda, often moving it away from the needs of the patients it is meant to serve.3 For these reasons, although there is much in common between the research that researchers and patients wish to see done, there are often important mismatches.4,5
Canadian anesthesia research is generally delivered through “responsive funding” programs to which researchers propose topics to various funding bodies. In Canada (as is elsewhere), the funding pool for anesthesia-related research is increasingly competitive and the research community is looking for direction and funding priorities.6,7,8 There is now recognition for a “needs-led” program, driven by a systematic approach to identifying and setting research priorities. A Canadian anesthesia and perioperative care research priority-setting framework could assist decision-makers to balance competing demands particularly as research funders are increasingly held accountable for resource allocation.9,10,11,12
Most Canadians will experience at least one surgery in their lifetime.13 In 2015–2016, there were approximately 1.47 million inpatient surgical procedures conducted in Canadian hospitals.14 Patients receive anesthesia and perioperative care for a variety of surgeries (or for the birth of a baby), but the consistent factor for these patients is the provision of anesthesia care. The large body of knowledge and diverse experience that these patients have is rarely drawn upon.
While most researchers remain guided by the medical model, hoping to understand physiologic mechanisms or prevent adverse outcomes, the social model of research seeks to answer questions and measure outcomes that matter to patients. This approach can increase the relevance and quality of research and lead to better patient outcomes, improved patient experience, and a more sustainable healthcare system.15,16,17 Regardless of the indication for surgery or anesthesia care, we assume that Canadian patients want to know that anesthesia care (in combination with the procedure they are undergoing) will help “cure” their disease, improve their health, reduce pain, or lead to the safe delivery of their newborn. But their priorities can only be truly discovered through patient-oriented research and patient engagement.18
Patient-oriented research engages patients as partners, and focuses on patient-identified priorities and improving patient outcomes.19 Notably, engaging patients in research does not limit the focus of the research to clinically focused questions. Patients can be, and are, engaged in preclinical research.20 Patients’ perspectives are essential to supporting a patient-oriented approach to research, regardless of the specifics of the research question. Patients’ perspectives are also essential to understanding whether healthcare services and procedures make a difference to patients’ health status and quality of life.21 An extensive search revealed a dearth of patient-oriented research in the published anesthesia literature.5,22,23
Formal processes, like those established by the James Lind Alliance (JLA), are being advocated to identify shared patient-oriented priorities and to propose topics for new research.24 Formal research priority setting is a systematic way of making the case to stakeholders for funded research on relevant, clinically important questions.25,26 The JLA method focuses on joint patient, caregiver, and clinician input to develop a “top ten” list. The JLA is a non-profit initiative, supported by the National Institute for Health Research in the United Kingdom (UK). The JLA methods for identifying shared clinician and patient/informal caregiver priorities around unanswered clinical questions have been used for over a decade to prioritize research uncertainties in almost 100 healthcare conditions internationally, including anesthesia and perioperative care priorities for the British National Institute for Academic Anesthesia (NIAA).25 Additional information on the JLA methods is available at http://www.jla.nihr.ac.uk/.
We set out to conduct a Canadian anesthesia and perioperative care research priority setting exercise as a rare and valuable opportunity to bring together patients, informal caregivers, and clinicians to suggest priorities for the Canadian anesthesia research agenda.24
Methods
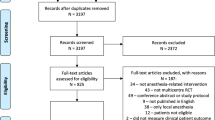
We used the JLA methodology to conduct a research priority setting partnership (PSP). See the Figure for the steps followed.
The Canadian Anesthesia Research Priority Setting Partnership (CAR PSP) was overseen by an independent senior JLA advisor (K.C.). We formed a steering committee (SC) with equal representation of anesthesia providers and patients/informal caregivers. The SC informed and directed all the research processes associated with the CAR PSP. This project received research ethics board approval (IWK Health Centre Research Ethics Board #1023459, June 7 2018).
Identifying and inviting partners
Where possible, Canadian partners with diverse anesthesia experiences were identified. Partners included patients and informal caregivers, clinicians, including anesthesiologists, nurses and allied healthcare professionals, all with experience of anesthesia and/or perioperative care. Medical specialty societies, professional and patient organizations and individuals were identified by the SC and invited to endorse the project and/or to nominate people for either the SC and/or attendance at the in-person final prioritization workshop. Eleven national organizations formally agreed to partner with the CAR PSP (Table 1).
Further partner recruitment through connections to Strategy for Patient-Oriented Research (SPOR) Units, to request aid in their respective jurisdictions, was facilitated by the Maritime SPOR Unit. The SPOR units are funded by the Canadian Institutes of Health Research to facilitate patient-oriented research. Voices and experiences from diverse and under-represented groups were specifically solicited through targeted recruitment, including contacting representative organizations.
Scope of the Canadian Anesthesia Research Priority Setting Partnership
The CAR PSP invited questions about all aspects of care during anesthesia and the perioperative period, and the management of longer-term problems that originated during this period. The management of chronic pain was not considered unless the pain originated around the time of anesthesia. The initial scope was discussed and further defined and clarified as part of the first SC meeting. This manuscript reflects the critical components of the CAR PSP protocol, and the full version is available at: http://www.jla.nihr.ac.uk/priority-setting-partnerships/anaesthesia-canada/. To facilitate future comparison with the one existing perioperative PSP, the scope of the CAR PSP closely mirrored the UK NIAA PSP.25
Inclusion criteria
The scope included all the work conducted by anesthesiologists, including obstetric and resuscitation care, as well as that conducted both by the wider perioperative team and the care pathway from initial intention to treat or operate onwards. “Onwards” was meant as an open-ended word signifying that long-term problems attributable to the surgery/intervention and management period must also be considered.
The perioperative period was defined to span the time from when a decision is made to have surgery or anesthesia care to the time that the patient returned to preoperative function, recovered to a stable functional level, or fully recovered from having surgery. There was no age limit and we actively encouraged involvement of people from diverse populations such as parents of newborns and young children, the elderly, Indigenous peoples, and those with disabilities.
Exclusion criteria
As the PSP focused on “perioperative care”, we excluded the surgery itself. We focused on the management of patients’ physical wellbeing within the hospital environment throughout all procedures and its impact on recovery thereafter. Many anesthesiologists provide critical care services, but this was felt to be beyond the scope of the current PSP.
Identifying unanswered questions (first survey)
We created and managed the CAR PSP online surveys using REDCap (Research Electronic Data Capture)27,28 hosted at the IWK Health Centre, Halifax, NS. Web links to the CAR PSP surveys were distributed by some of the 11 partner national perioperative organization email listservs and newsletters. In addition to patient networks (e.g., Patients for Patient Safety Canada, Patient Voices Network), the surveys were promoted through the project’s website (http://www.car-psp.ca), Twitter (@car_psp), and Facebook (fb.me/carpsp).
Respondents to the first survey were asked to submit three questions that they would like anesthesia researchers to address. Specifically, respondents were asked “Based on your experience, what questions do you have? No question is too big or too small! Please provide up to three questions about anesthesia or perioperative care that you want research to answer. You can provide details about your own experiences, if you would like to do so.” Prior to this question, participants saw a page with plain language explanations of the terms “anesthesia” and “perioperative care.”
Respondent demographics were assessed weekly and the survey closed once efforts to gain responses from all Canadian provinces and territories, across ages, sex, and types of healthcare providers within the main groups of respondents (clinicians, patients, and caregivers) were made. Targeted efforts to recruit respondents included contacting groups like Prostate Cancer Canada (for male patients), the Society of Rural Physicians of Canada (for rural and/or family physicians), and the Assembly of First Nations (for Indigenous respondents). At our request, some organizations shared the survey via their social media and/or newsletters.
Question management
Following the first survey, all submitted questions were aggregated into a longlist of summary questions with duplicate or highly-related questions aggregated into single questions. An independent information specialist, with previous priority-setting experience from an unrelated PSP, in consultation with members of the SC, then removed any out-of-scope questions. The SC reviewed this work, and a SC subgroup worked with the project manager (J.B.) to further refine wording and to develop a final list of summary questions.
Verifying uncertainties and reviewing evidence
With the help of an evidence synthesis specialist from the Maritime SPOR Unit, the longlist of summary questions was compared with the published literature to determine the extent to which any of the questions were already answered. This process followed JLA guidance of reviewing Cochrane systematic reviews (SR) published within the past three years. Specifically, the evidence synthesis specialist retrieved Cochrane SRs by the anesthesia group, and these were reviewed by the project manager, with consultation of SC members. These longlist summary questions were subsequently divided into those “with an answer” and those “without an answer” in the scientific literature. Questions were considered unanswered if the SR was not up to date (within the last three years); the SR did not have enough available evidence; the SR evidence was of insufficient quality; or the SR was inconclusive/unable to make conclusions.
Interim prioritization (second survey)
A refined longlist of “summary” questions unanswered by the literature from the first survey was put into a second national online survey. This survey gave respondents an opportunity to review the longlist and choose which questions ought to be discussed for final prioritization. Participants across Canada were asked to choose up to ten questions that they thought were top priorities from the longlist, according to their personal or professional experience. Participants in the second survey were recruited in much the same manner as for the first survey. For the second survey, however, we also directly emailed participants from the first survey who had provided their email addresses.
To support similar representation of key partnership categories, we pre-specified that responses to the second survey would be considered by respondent category (patients and caregivers; healthcare providers) so that their priorities could be considered independently. This strategy ensured that the top ten priorities from each group were included in the shortlist for the workshop.
Final prioritization workshop
The final prioritization to determine the CAR PSP top ten priorities was held as an in-person workshop. Individuals and members from partner organizations were invited to send expressions of interest to participate. The SC sought to involve a balance of patients and healthcare providers at the workshop. Participants were selected to represent geographical and experiential diversity.
The workshop followed the JLA’s standard method, an adapted nominal group technique, in which participants work in three small groups with balanced representation of patients, caregivers, and clinicians, to rank the short-listed questions. After each group ranked its priorities, prioritizations were averaged across the three groups. This allowed for a second round of prioritization in three newly formed but similarly balanced small groups. Again, an aggregate ranking was calculated. The final top ten priorities were then determined by consensus through a large group plenary discussion facilitated by the JLA advisor (K.C.).
Results
Identifying unanswered questions (first survey)
A total of 254 respondents submitted 574 initial questions. Nine responses were submitted in French. See Table 2 for demographic details. A total of 505 in-scope questions were aggregated into a longlist of 49 summary questions. The SC agreed that 69 questions were not in-scope, so they were not aggregated into the summary questions. Table 3 shows an example of how the initial questions were aggregated into summary questions. Following the evidence review, the SC agreed that no questions were fully answered, so the longlist of 49 questions was retained for the interim prioritization survey. Table 4 shows this longlist of questions.
Summary of interim prioritization results (second survey)
A total of 233 respondents submitted their priorities for the 49 anesthesia summary unanswered questions. Ten responses were submitted in French. Table 5 shows the demographic details. The results were computed within the groups of patients/caregivers and healthcare providers (Table 6). The ten highest-ranked priorities for both groups were considered independently. Given that there were some differences, and some commonalities, in the ten highest-ranked priorities for both groups, this resulted in 24 questions that were most highly ranked by both groups of respondents. These were considered at the final in-person prioritization workshop.
Final prioritization workshop and “top ten”
Three facilitators (one senior advisor from the JLA, and two with experience facilitating JLA PSP final workshops) supported 22 participants (14 (64%) patients/caregivers) in the final in-person prioritization workshop. Following two rounds of group-level prioritization, the full workshop agreed, by consensus, on the CAR PSP top ten priorities (Table 7).
The top ten list from this PSP contains many patient-oriented priorities, such as improving pain control after surgery. The list reflects shared priorities of patients and healthcare providers. For example, the priority around preventing errors and patient injuries was derived from initial questions submitted by both patients and healthcare providers and ranked highly after the second survey (patients: #3, healthcare providers: #4) and at the final workshop (#4).
Discussion
The Canadian anesthesia community is changing how it thinks about research in anesthesia and perioperative care, aligning the agenda to patient-oriented research. This opportunity to engage patients’ perspectives around anesthesia and perioperative care is timely and has the potential to improve research impact and patient outcomes.29,30,31 The CAR PSP top ten priorities reflect a wide variety of priorities that capture a broad spectrum of Canadians who receive and provide anesthesia care, and the scope of anesthesia practice. Using the CAR PSP top ten priorities to shape the Canadian anesthesia research agenda will reflect shared concerns around the impact of anesthesia and perioperative care on patient-reported outcomes and experience. These top ten priorities complement and can, in many cases, align with the typical curiosity-based research that has always been fundamental to anesthesia research.
The CAR PSP featured responses from hundreds of Canadian patients, healthcare providers, and others, and reached a consensus priority list from an initial submission of 574 questions. The CAR PSP top ten priorities included factors most important to improve patient outcomes and satisfaction, impacts of shared decision-making, error prevention, and the impact of reducing opioids at time of surgery.
The CAR PSP top ten priorities are general in-scope and should not be considered specific research question themselves, nor hypothesis generating. They should serve as starting points for researchers, funders, and decision-makers. They also identify questions around anesthesia care, where the answers can have immediate translatable impacts on our patients’ daily lives.
Strengths of our study include using an established methodology to elicit shared priorities on anesthesia and perioperative care, the number of participant submissions, and the balance of patient, caregiver and clinician participation. Even with effective promotion and publicity, a PSP may face limited stakeholder engagement. Anesthesia does not involve caring for patients with a chronic condition/disease, nor a well-defined patient group, so engagement can be challenged. The CAR PSP survey response numbers were similar to other PSPs in Canada and to the NIAA PSP.32,33 (Canadian population of 37 million, approximately 3,300 anesthesiologists; UK population 61 million, approximately 11,000 anesthesiologists, NIAA PSP reported 623 respondents and 1,420 suggestions.)13,25,34,35
The CAR PSP captured responses from individuals from all provinces, with a range of ages, and with a good balance of gender identity. PSPs are not designed to attract a representative sample, instead the JLA process relies on engagement, and the SC focused on getting responses from members of key stakeholder groups. Whenever the SC saw that responses from a particular group (e.g., northern communities) were lacking, we targeted outreach to those groups. Despite as many efforts as were practical within time constraints and budget, these were not always successful (e.g., no respondents from the territories) and this is a limitation.
Our focus on the entire anesthesia and perioperative care period, over a wide range of subspecialty anesthesia care for diverse surgical procedures and patient groups, could be considered too broad. This PSP, unlike some others, including the NIAA, did not group the initially submitted questions into subspecialty-related anesthesia themes or patient groups (e.g., cardiac anesthesia or pediatric patients). Subspecialty questions were grouped into more manageable broad-based summary questions. As such, there are few anesthesia subspecialty top ten priorities. Nevertheless, examples of submitted questions, the summary list of 49 questions, and the 24 highest-ranked questions are available to researchers to review on the JLA website. Researchers are encouraged to explore in more depth the original questions that contributed to the research questions in the prioritization survey. Furthermore, as a first PSP in the Canadian anesthesia community, our methods and experience could support future efforts for setting priorities within more specific aspects of perioperative care.
Limitations
Given that the surveys for this PSP were only available online, we acknowledge that they were not accessible to people who may not use, or have access to, the internet. We relied on word-of-mouth, social media, and partner organizations to advertise the surveys, so we likely missed potential respondents who are not engaged through these methods. Our surveys garnered more responses from healthcare providers than patients and caregivers, though our SC had equal representation and our final workshop had more patients and caregivers than healthcare providers.
The final workshop took place over a full day in Toronto. Although we covered expenses for travel, and provided an honorarium for patients to attend, this kind of workshop excludes potential participants who cannot take time off work or cannot travel for other reasons.
The methods used for establishing a top ten list of priorities were qualitative in nature. We followed a well-established methodology that invites a variety of perspectives to contribute in different ways (i.e., SC, participation in surveys, final workshop). All these opportunities to contribute are complementary and instrumental in arriving at a top ten list of priorities. A different top ten list of priorities may have resulted had different people joined the SC or participated in the surveys or final workshop.
Future initiatives
Only one other country, the UK, has incorporated shared patient/caregiver input regarding anesthesia research priorities.25 The CAR PSP adds to the breadth of what is currently known from the UK. Differences in demographics, varied geographic location and population density, as well as healthcare funding models and delivery between Canada and the UK exist. As such, there is not enough experience to know whether research priorities identified in one country can be adopted by another country. An in-depth comparison of the CAR PSP top ten and the NIAA top ten is warranted to assess similarities and generalizability across countries. It appears that the top ten lists for both countries share some similar questions. For example, both PSPs identified pain after surgery and long-term effects of anesthesia as priorities for research. Differences exist, however, such as with the priority around the impact of reducing opioids during surgery appearing in the Canadian list, but not the UK one.
Additionally, we will assess how the CAR PSP priorities ranking differed between the patient/caregiver and clinician groups and impacted the CAR PSP top ten priorities.
Using the CAR PSP top ten
Following the established methodology of the JLA, the Canadian anesthesia research community now has a made-in-Canada top ten list of shared priorities that can help situate and direct their projects. Funders may choose to focus their calls for applications around these priorities. Commitment to patient-oriented research can also be shown by funding proposals that align with the top ten priorities, funding projects with patient partners as co-investigators on the research team, or including patient reviewers in the grant review processes.
The top ten priorities are not prescriptive. If a topic did not rank in the final top ten, this does not mean it is unimportant research. Researchers are encouraged to consider how their current and future projects can align with the top ten. For example, the priority of “How can anesthesiologists improve pain control after surgery?” lends itself to a broad range of research questions, from preclinical research leading to development of new drugs, to psychological interventions that help patients manage pain.
Call to action
The CAR PSP top ten priorities represent the collective wisdom of the participants who contributed to the CAR PSP and they deserve the attention of the research community. The CAR PSP top ten priorities are a call to action and serve as a valuable tool to initiate and guide patient-oriented research in anesthesia and perioperative care. This initiative is particularly important in anesthesia research where the patient perspective has not frequently been incorporated. This PSP has forged important relationships among patients/caregivers, healthcare providers, and researchers, and is a springboard for a sustained culture of patient engagement within anesthesia research.
References
George RB, McKeen DM. We must ask relevant questions and answer with meaningful outcomes. Can J Anesth 2017; 64: 899-903.
Heneghan C, Goldacre B, Mahtani KR. Why clinical trial outcomes fail to translate into benefits for patients. Trials 2017. DOI: https://doi.org/10.1186/s13063-017-1870-2.
Government of Canada; Canadian Institutes of Health Research. Strategy for Patient-Oriented Research - Patient Engagement Framework. Available from URL: http://www.cihr-irsc.gc.ca/e/48413.html (accessed December 2019).
Thornton H. Patient and public involvement in clinical trials. BMJ 2008; 336: 903-4.
James Lind Alliance Priority Setting Partnerships. About Priority Setting Partnerships. Available from URL: http://www.jla.nihr.ac.uk/about-the-james-lind-alliance/about-psps.htm (accessed December 2019).
Orser BA, Miller DR. New opportunities for anesthesia research in Canada. Can J Anesth 2002; 49: 895-9.
Bevan DR. The future of academic anesthesia departments in Canada. Can J Anesth 2006; 53: 533-9.
Tsui BC, Li LX, Ma V, Wagner AM, Finucane BT. Declining randomized clinical trials from Canadian anesthesia departments? Can J Anesth 2006; 53: 226-35.
Bate A, Mitton C. Application of economic principles in healthcare priority setting. Expert Rev Pharmacoecon Outcomes Res 2006; 6: 275-84.
Mitton C, Donaldson C. Tools of the trade: a comparative analysis of approaches to priority setting in healthcare. Health Serv Manage Res 2003; 16: 96-105.
Harrison A, Mitton C. Physician involvement in setting priorities for health regions. Healthc Manage Forum 2004; 17: 21-7.
Robinson A. Patient and public involvement: in theory and in practice. J Laryngol Otol 2014. DOI: https://doi.org/10.1017/S0022215114000735.
Organisation for Economic Co-Operation and Development. Health Care Utilisation: Surgical procedures. Available from URL: https://stats.oecd.org/index.aspx?queryid=30167 (accessed December 2019).
Canadian Perioperative Anesthesia Clinical Trials Group. Available from URL: https://canadianpact.ca/ (accessed December 2019).
Brett J, Staniszewska S, Mockford C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect Int J Public Particip Health Care Health Policy 2012; 17: 637-50.
Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, et al. Patient and service user engagement in research: a systematic review and synthesized framework. Health Expect 2015; 18: 1151-66.
Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res 2014. DOI: https://doi.org/10.1186/1472-6963-14-89.
Myles PS. Perioperative outcomes: are we asking the right questions? Can J Anesth 2016; 63: 138-41.
Crowe S, Fenton M, Hall M, Cowan K, Chalmers I. Patients’, clinicians’ and the research communities’ priorities for treatment research: there is an important mismatch. Res Involv Engagem 2015. DOI: https://doi.org/10.1186/s40900-015-0003-x.
Cowan K. Can patients be involved in preclinical research? BMJ Open Science. Available from URL: https://blogs.bmj.com/openscience/2018/06/05/can-patients-be-involved-in-preclinical-research/ (accessed December 2019).
Canadian Institute for Health Information. Patient-reported outcome measures (PROMs). Available from URL: https://www.cihi.ca/en/patient-reported-outcome-measures-proms (accessed December 2019).
O’Leary JD, Crawford MW. Bibliographic characteristics of the research output of pediatric anesthesiologists in Canada. Can J Anesth 2010; 57: 573-7.
Government of Canada; Canadian Institutes of Health Research. ICRH Strategic Plan 2013-2016. Available from URL: http://www.cihr-irsc.gc.ca/e/47022.html (accessed December 2019).
Solomon MZ, Gusmano MK, Maschke KJ. The Ethical imperative and moral challenges of engaging patients and the public with evidence. Health Aff (Millwood) 2016; 35: 583-9.
Boney O, Bell M, Bell N, et al. Identifying research priorities in anaesthesia and perioperative care: final report of the joint National Institute of Academic Anaesthesia/James Lind Alliance Research Priority Setting Partnership. BMJ Open 2015. DOI: https://doi.org/10.1136/bmjopen-2015-010006.
Boney O, Nathanson MH, Grocott MP, Metcalf L; Steering Group for the National Institute of Academic Anaesthesia/James Lind Alliance Anaesthesia and Peri-operative Care Priority Setting Partnership. Differences between patients’ and clinicians’ research priorities from the Anaesthesia and Peri-operative Care Priority Setting Partnership. Anaesthesia 2017; 72: 1134-8.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377-81.
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019. DOI: https://doi.org/10.1016/j.jbi.2019.103208.
Aubin D, Hebert M, Eurich D. The importance of measuring the impact of patient-oriented research. CMAJ 2019; 191: E860-4.
Esmail L, Moore E, Rein A. Evaluating patient and stakeholder engagement in research: moving from theory to practice. J Comp Eff Res 2015; 4: 133-45.
Staley K. ‘Is it worth doing?’ Measuring the impact of patient and public involvement in research. Res Involv Engagem 2015. DOI: https://doi.org/10.1186/s40900-015-0008-5.
Manns B, Hemmelgarn B, Lillie E, et al. Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 2014; 9: 1813-21.
Rees SE, Chadha R, Donovan LE, et al. Engaging patients and clinicians in establishing research priorities for gestational diabetes mellitus. Can J Diabetes 2017; 41: 156-63.
Government of Canada SC. Population - Canada at a Glance, 2018. Available from URL: https://www150.statcan.gc.ca/n1/pub/12-581-x/2018000/pop-eng.htm (accessed December 2019).
Canadian Medical Association. Anesthesiology. Available from URL: https://www.cma.ca/anesthesiology (accessed December 2019).
Author contributions
Dolores M. McKeen, Jillian C. Banfield, Daniel I. McIsaac, Jason McVicar, Colleen McGavin, Katherine Cowan and Andreas Laupacis contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Mary Anne Earle, Claire Ward, Katharina Kovacs Burns, Donna Penner, Gilbert Blaise and Thierry De Greef contributed to acquisition, analysis, and interpretation of data. The Perioperative Anesthesia Clinical Trials Group (PACT) contributed to the conception and design of the project.
Acknowledgements
We thank the editorial board of the Canadian Journal of Anesthesia who provided French language translation of the two surveys. We thank the Maritime Strategy for Patient Oriented Research (SPOR) SUPPORT Unit (MSSU) for their support and connections to other Canadian SPOR Units to request support and recruitment aid in their respective jurisdictions. Specifically, we thank Leah Boulos, Brian Condran, Julia Kontak, and Michelle Fiander. We also thank Melissa Crane for her work to synthesize the initial questions into summary questions. We are especially grateful to Katherine Cowan for her expert guidance throughout this project.
Conflicts of interest
None.
Funding statement
The Canadian Anesthesia Research Priority Setting Partnership was funded through a Canadian Institutes of Health Research – Strategy for Patient Oriented Research (CIHR SPOR) Collaboration Grant. This Top 10 priorities are an initial output of a grant aimed to support patient-oriented Canadian anesthesia research. Collaborating funding organizations: Association of University Departments of Anesthesia (ACUDA). Canadian Anesthesiologists’ Society (CAS). Canadian Institutes of Health Research (CIHR). Dalhousie University Department of Anesthesia, Perioperative and Pain Medicine. Northern Ontario School of Medicine Department of Anesthesia. Perioperative Anesthesia Clinical Trials Group (PACT). University of Manitoba Department of Anesthesia
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an editorial. Please see Can J Anesth 2020; 67: this issue.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McKeen, D.M., Banfield, J.C., McIsaac, D.I. et al. Top ten priorities for anesthesia and perioperative research: a report from the Canadian Anesthesia Research Priority Setting Partnership. Can J Anesth/J Can Anesth 67, 641–654 (2020). https://doi.org/10.1007/s12630-020-01607-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-020-01607-6