Abstract
Purpose
Pupillometry is a technique for objective quantification of nociception that takes into account the central processing of noxious stimuli and its sympathetic response. This narrative review provides an overview of the physiology of the pupil, the principles of pupillometry, and its potential application in the perioperative environment, especially in nociception monitoring and quantifying responses to opioids.
Source
Relevant articles, including reports of original investigation, review articles, and meta-analyses were identified from searches of PubMed and Google Scholar databases. Articles that described pupillary physiology and pupillometry, along with original research reports of the application of pupillometry in perioperative and critical care environment were used to synthesize a narrative review.
Principal findings
Pupillometry is emerging as an objective measure of nociception, especially in patients under general anesthesia, children, non-verbal patients, and critically ill patients who cannot effectively communicate ongoing pain. Portable automated pupillometers have made accurate quantification of pupillary reflexes, including light reflex and dilatation reflex, possible. This technique has been successfully studied in the perioperative setting for a number of applications, including quantification of nociception, response to analgesia, and assessing efficacy of regional blocks. Pupillary oscillations have shown promise in assessing central opioid effects. Pupillometers can also accurately quantify light reflexes during the neurologic evaluation of critically ill patients.
Conclusions
Pupillometry is an easy to use non-invasive bedside technique to quantify nociception and monitor opioid effects. It has the potential to personalize pain management in perioperative and intensive care unit environments. Additional studies are needed to further understand the utility of pupillometry in this context.
Résumé
Objectif
La pupillométrie est une technique de quantification objective de la nociception qui tient compte de l’intégration centrale des stimuli douloureux et de la réponse sympathique de la pupille. Cette revue narrative donne un aperçu de la physiologie de la pupille, des principes de la pupillométrie et de son application potentielle dans le contexte périopératoire, en particulier dans le monitorage de la nociception et la quantification des réponses aux opioïdes.
Source
Les articles pertinents, comprenant les comptes rendus de recherche originale, les articles de synthèse et les méta-analyses, ont été identifiés à partir de recherches dans les bases de données PubMed et Google Scholar. Les articles décrivant la physiologie de la pupille et la pupillométrie, ainsi que des comptes rendus de recherche originale portant sur l’application de la pupillométrie dans le contexte périopératoire et des soins intensifs, ont été utilisés pour synthétiser un compte rendu narratif.
Constatations principales
La pupillométrie est une modalité émergente en tant que mesure objective de la nociception, en particulier chez les patients sous anesthésie générale, les patients pédiatriques, les patients qui ne parlent pas et les patients en état critique qui ne peuvent pas communiquer de façon efficace leur douleur. Les pupillomètres automatisés portatifs ont rendu possible la quantification précise des réflexes pupillaires, y compris du réflexe photomoteur et du réflexe de dilatation. Cette technique a été étudiée avec succès dans le cadre périopératoire pour plusieurs applications, y compris la quantification de la nociception, la réponse à l’analgésie et l’évaluation de l’efficacité des blocs régionaux. Les oscillations pupillaires se sont montrées prometteuses pour l’évaluation des effets centraux des opioïdes. Les pupillomètres peuvent également quantifier avec précision les réflexes photomoteurs lors de l’évaluation neurologique des patients en état critique.
Conclusion
La pupillométrie est une technique au chevet non invasive facile à utiliser pour quantifier la nociception et surveiller les effets des opioïdes. Cette technique pourrait permettre de personnaliser la prise en charge de la douleur dans les environnements périopératoires et de soins intensifs. D’autres études sont nécessaires pour mieux comprendre l’utilité de la pupillométrie dans ce contexte.
Similar content being viewed by others
Despite numerous advancements in perioperative medicine, pain management continues to be a challenging perioperative issue with approximately 20-80% of surgical patients reporting moderate to severe pain.1,2 It is especially difficult to assess nociception under anesthesia, and pain postoperatively in children or in patients who are non-verbal. Pain is a highly subjective sensation, so methods to quantify pain, such as the visual analogue scale (VAS) and numerical rating scale (NRS), are similarly subjective. These scales may be inaccurate and challenging to use in children, elderly patients with cognitive decline, unconscious critically ill patients, and in patients recovering from general anesthesia (GA). Nociception represents the neural correlate of pain, leading to autonomic responses such as tachycardia, hypertension, pupillary dilatation, sweating, and tearing. Therefore, these autonomic responses can potentially be used as surrogate measures to quantify nociception and response to analgesic therapy. Methods such as measuring heart rate variability, skin conductance, and pupillary dilatation and electroencephalograhy (EEG) have been tested to quantify intraoperative nociception.3 The analgesia nociception index (ANI) is based on heart rate variability.4 Multi-parameter indices have also been described for assessment of intraoperative nociception. These include surgical pleth index (based on heart beat interval and pulse wave amplitude)5 and the nociception level index (which is a composite based on heart rate, heart rate variability, photoplethysmograph wave amplitude, skin conductance, skin conductance fluctuations, and their time derivatives).6 A review by Ledowski describes the nociception monitoring technologies that are currently commercially available.3
This present review focuses on pupillary evaluation for assessment of nociception and its effects on analgesic therapy. The eyes have long been a subject of special interest in medicine. Some ancient sources have called the eyes “the window to the soul”. Nevertheless, the un-aided visual assessment of pupillary responses is often inaccurate and subject to inter-observer variability. The availability of quantitative pupillometers (see Fig. 1 and eVideo in the Electronic Supplementary Material) that can be used at the bedside has made accurate measurement of various pupillary parameters possible and increasingly more adaptable clinically. In an era of precision medicine, the ability to accurately quantify pupillary dynamics is a potentially powerful innovation. This narrative review provides an overview of pupillary physiology and summarizes the literature on the application of pupillometry in perioperative medicine and the intensive care unit (ICU), with special emphasis on nociception monitoring.
Search methods
Articles for this review were identified from a search of PubMed and Google Scholar using the keywords of “pupillometry”, “pupillary reflex”, “pupillary response”, “anesthesia”, “analgesia”, “opioid”, “pain”, “nociception”. All studies where pupillometry was used in the context of monitoring pain, nociception, antinociception, and opioid effect were chosen. Only references with at least an abstract in English were chosen. Additional articles were identified using hand searches of references from the retrieved articles.
Physiology
The pupil is the central aperture in the iris and its diameter is determined by the contraction of two antagonizing smooth muscle groups. The circular sphincteric muscle, which keeps the pupil constricted and forms the predominant iris musculature, receives parasympathetic innervation through the oculomotor nerve (cranial nerve [CN] III) and short ciliary nerves via the muscarinic receptors. The radial muscle dilates the pupil and is sympathetically innervated by long ciliary nerves from the cervical sympathetic ganglion via the α1 adrenergic receptors.7 This radial smooth muscle is comparatively weaker than the circular muscle, and as a result, the baseline natural tendency of the pupil is to remain constricted, unless sympathetic activity/blockade of pupilloconstrictor neurons cause dilatation. Ophthalmological significance is in determining the cause of anisocoria.8 Innervation of iris smooth muscles and neural pathways mediating pupillary reflexes are depicted in Fig. 2.7
Parasympathetic and sympathetic supply of iris muscles. The parasympathetic innervation of the pupil sphincter via the oculomotor nerve and short ciliary nerve is shown on the left. This is inhibited by central supranuclear inhibition of Edinger–Westphal (EW) nuclei via α2-adrenergic receptor activation, resulting in relaxation of the pupil sphincter muscle. Opioids inhibit the central inhibitory neurons of the EW nucleus, resulting in pupillary constriction. The sympathetic innervation of the pupillary dilator through the long ciliary nerve is shown on the right. This figure was modified from “Eyeing up the future of the pupillary light reflex in neurodiagnostics”; Diagnostics, by Hall et al.,7 licensed under CC BY (http://creativecommons.org/licenses/by/4.0/)
Pupillary light reflex (PLR)
The PLR consists of pupillary constriction in response to light—either directly or consenually from stimulation of the opposite pupil.7 The un-aided human eye can readily appreciate this pupillary constriction. Afferent input from the retina passes through the optic nerve (CN II) and is integrated in the Edinger–Westphal (EW) nucleus of the midbrain. The parasympathetic efferent signals travel through the oculomotor nerve (CN III). Post-ganglionic nerves reach the sphincter pupillae through the short ciliary nerves, causing pupillary constriction. There are two cholinergic nerve endings in the pupilloconstrictor pathway, with the first being the synapse at the ciliary ganglion. This contains Nn nicotinic receptors and can be blocked by ganglion blockers such as hexamethonium.8 The second neuromuscular junction at the pupillary sphincter smooth muscle contains muscarinic receptors that can be blocked by atropine.8 Since the constriction phase of PLR is completely under parasympathetic control, measures of constriction are considered robust parameters to detect parasympathetic dysfunction and evaluate the integrity of CNs II and III
Pupillary reflex dilatation (PRD)
Pupillary dilatation occurs during the recovery phase of PLR, dark adaptation, and in response to an alerting stimulus (which includes response to pain).8 Pupillary dilatation is predominantly driven by the sympathetic nervous system, as the pupillary dilators receive sympathetic innervation.7 The first-order neurons from the hypothalamus descend down the spinal cord to synapse with the second-order (pre-ganglionic) neurons at C8-T1. These second-order neurons relay signals to the post-ganglionic long ciliary nerves at the cervical sympathetic ganglion. The first- and second-order neurons are cholinergic. The long ciliary nerves release noradrenaline at the neuromuscular junction of pupillary dilator muscles, acting on α1 receptors to cause active pupillary dilatation.7
Passive dilatation is one of two mechanisms contributing to PRD, the other being sympathetic mediated active dilatation. Passive dilatation of the pupil results from supranuclear inhibition of the EW nucleus causing relaxation of the sphincter pupillae. The α2 adrenergic neurons from the brainstem reticular activating system inhibit pre-ganglionic neurons in the EW nucleus.7 Horner syndrome, seen after cervical sympathectomy, results from unopposed parasympathetic activation of iris and hence miosis.8 The contribution of the humoral sympathetic response in PRD has also been investigated, with blood catecholamine levels in response to surgical stress or pain and vasopressor infusions have shown to be inadequate in eliciting a measurable PRD.9 Nevertheless, pheochromocytoma—a condition that can produce very high blood catecholamine levels—was shown to cause pupillary dilatation.10 Quantitative measurement of PRD is of growing interest as it could be used as a tool to quantify pain. The PRD is evoked in response to a noxious stimulus and the reflex fades in patients with steady unrelenting pain. Therefore, a standardized noxious stimulus (usually a tetanic stimulus using a skin electrode) is applied to elicit and measure PRD.11
As PRD is a result of a complex interaction between spinal sympathetic and supraspinal pathways, it can be influenced by a number of intrinsic and environmental factors. This is elaborately reviewed by Loewenfeld.12 The EW neurons have a resting tone and fire continuously, activating the parasympathetic pupillo-constrictors.8 Inhibitory inputs to the EW nucleus come from neurons in the midbrain, posterior hypothalamus, and the reticular activating system, arising from stimuli such as arousal or pain.7,8 Pain concurrently increases the sympathetic activity; therefore, PRD is elicited through both sympathetic activation and central inhibition of the EW nucleus. The relative contribution of these two components varies depending on the state of awareness of the individual. In a normal awake individual, the spinal sympathetic pupillo-dilator pathway plays a major role, as indicated by the absence of PRD after topical α1 blockade.9 Nevertheless, in the anesthetized patient, a robust PRD is found even after sympathetic block,13 denoting the role played by the supraspinal pathways. An intact supraspinal component can bring about a PRD without active sympathetic pupillodilatation, but the reverse does not occur. In a study of brain dead organ donors, PRD could not be elicited in individuals with an intact sympathetic response to pain but no brain stem function.9
Other animal species show widely variable neurophysiology behind pupillary reflexes; therefore, results from animal studies may not translate to humans. There is a strong humoral component of the reflex in some animals that is not found in humans.8 Central α2 receptors play a prominent role in afferent and efferent pathways of PRD in animals.14 The role played by non-adrenergic, non-cholinergic neural pathways in PRD remain to be determined.15
Pupillary oscillations
The pupil undergoes sustained physiologic oscillation with a frequency of 0.2 Hz, varying in diameter by 1-2 mm.16 This phenomenon of pupillary unrest, also known as pupillary hippus, remains prominent during a mentally relaxed state and disappears with mental activity. While hippus might introduce potential errors into the pupillary readings, it could be easily prevented by repeated measurements over a period of time. Pupillary unrest happens both in darkness and ambient light. Patterns of change in pupillary unrest have been evaluated in assessing nociception and central opioid effects.
Pupillometry
PLR may be characterized as “normal, brisk, or sluggish”, which is subjective and inaccurate. Visual assessment of PRD is also problematic, as PRD has a longer latency and duration than PLR does.17 Objective quantification of these reflexes can be made with pupillometers—i.e., hand-held, non-invasive devices used to accurately quantify pupillary reflexes. The acquired images are plotted as a function of time, and the results processed to provide pupillary parameters and indices. These portable pupillometers use infrared rays to create an iris/pupil image and measure the pupillary size in millimetres down to the hundredth place.18,19 Using visible light would elicit a PLR; therefore, the PRD measurement uses infrared rays to avoid confounding.8
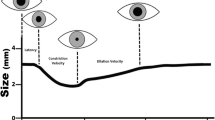
The pupillometer provides several PLR parameters including latency, maximum constriction amplitude (MCA), pupillary light reflex amplitude (PLRA), constriction velocity (CV), and dilatation velocity (DV).18 Latency is the duration between light exposure and the onset of pupillary constriction, measured in seconds and accurate to the hundredth. The MCA is the difference between the initial and final pupillary diameters. Dividing this value by the duration of constriction gives the CV (mm·sec−1). The DV is obtained in a similar way. Pupillary light reflex amplitude is expressed as a percentage of pupil size change from baseline in response to light. The neurologic pupillary index (NPi) is derived from latency, CV, and DV using proprietary algorithms.18 It is a dimensionless number between 0 and 5 to grade the robustness of PLR. Used in critically ill patients to evaluate brain function, values > 3 are considered normal and 0 indicates no PLR.18,20 Phases of PLR and the associated pupillometry measures are depicted in Fig. 3. Lussier et al. reported normal ranges of PLR parameters in more than 2,100 individuals admitted to the neuro-critical care unit.18 Individuals with normal/near normal levels of Glasgow coma scale (GCS) (13-15) had a NPi of 4.3, pupillary size of 3.2 mm, latency of 0.3 sec, CV of 2 mm·sec−1, and DV of 0.6 mm·sec−1. The PLR is being widely used in neurologic evaluation of critically ill patients with traumatic brain injury, stroke, post-cardiac arrest, and intoxication, and in diagnosis of brain death.21 The PLRA has been shown to significantly increase in response to noxious stimulus, although evidence is weak and application of PLR in this context is not as common as PRD.11
Phases of pupillary light reflex and the corresponding pupillometry measures. Latency is the time elapsed from the light stimulus to the beginning of constriction. This is followed by a phase of maximum constriction which is further followed by a slow dilatation phase called the pupil escape (during a continuous light stimulus). The maximal and average slopes of the constriction phase provide the maximal and average constriction velocities, respectively. Similarly the slope of the dilation phase provide dilation velocity. These denote the change in pupillary diameter per unit time. The baseline diameter is denoted as maximum aperture,and the trough provides the minimum aperture.
The PRD is measured by administration of a standardized cutaneous tetanic pain stimulus. Usually the stimulus is at 100 Hz with an amplitude of 40-60 mA, synchronized with pupillary measurement.22 The duration of the stimulus used is variable among studies, ranging from one to ten seconds.22,23,24 This technique is used to obtain amplitude, latency, and duration of PRD. A PRD amplitude > 30% has been associated with systemic manifestations of tachycardia and hypertension.25 In many studies, a PRD amplitude between 13% and 25% is usually chosen as a threshold large enough to signify pupillary response to noxious stimulus, without the associated systemic response.26,27 Instead of using a pre-defined stimulus of 40-60 mA, some researchers use a 100-Hz electrical stimulus, with stepwise increments of 10 mA every second, starting from 10 mA up to 60 mA.22 Once the PRD amplitude reaches ≥ 13%, the stimulus is stopped from increasing further. The amplitude and the electrical intensity are used to determine the pain pupillary index (PPi). The PPi is a dimensionless number between 1 and 9 used to quantify nociception—the greater the electrical intensity required to elicit a pupil dilatation ≥ 13%, the lower the PPi and nociception (Table 1).22,28 The latency of PRD is approximately 0.8 sec and the duration may last up to several minutes after a tetanic stimulus.17 Pupillary reflex dilatation amplitude and PPi are usually used as the surrogate autonomic markers to quantify nociception and the effect of analgesic interventions in anesthetized or unconscious patients.
Pupillary unrest under ambient light (PUAL) is measured using infrared pupillometry for a duration of 16 sec. The data are Fourier transformed and after artefacts are removed, the area under the curve gives the PUAL.29 It comprises the sum of oscillatory amplitudes between 0.3 and 3 Hz frequencies.30 The mean (standard deviation) PUAL from a total of 4,589 separate measurements from over 1,000 individuals has been reported by McKay et al. to be 0.246 (0.125).30 The variation coefficient of pupillary diameter (VCPD) is another method used to quantify pupillary oscillations. Oscillations are recorded for a duration of ten seconds and VCPD is calculated as the median deviation divided by the median.31
Factors influencing pupillary reflexes
Pupillary size
Many factors influence measurement of the PRD; the most important factor being the resting size of the pupil. Most other factors indirectly affect the pupillary reflexes by influencing the pupillary resting size. The iris muscles have a large dynamic range (corresponding to a pupillary diameter [PD] between 2 and 7 mm) during which their CV is maximal.32 A mid-position pupil is approximately 4 mm (range 3-5 mm), and anything < 2 mm is appreciated by the naked eye as a “pin-point” pupil.
Ambient light
The next most important factor influencing PRD is ambient light, as it causes pupillary constriction and alters retinal sensitivity.8 Therefore, infrared light is used for pupillary measurements in pupillometers. Portable pupillometers also come with an opaque cup used to cover the measured eye for a few seconds before a reading to exclude any influence of ambient light. The contralateral eye is manually covered from light to prevent the consensual light reflex. Though complete exclusion of ambient light may not be possible, it is best to ensure the same amount of ambient light during each pupillometric measurement.
Effect of drugs
Drugs play an important role in modifying pupillary reflexes. Opioids, the most widely studied group of drugs in this context, cause miosis through the central disinhibition of EW neurons.33 Opioids have different effects on PLR and PRD. With respect to PLR, opioids do not alter PLRA or CV when the values are normalized to the resting size of the constricted pupil.32,34 A measurable PLR has been shown with hypoxia and hypercarbia in the setting of opioid-induced respiratory depression; this is a result of the associated sympathetic stimulation.32 Conversely, opioids at analgesic doses reduce the PRD amplitude in response to standardized noxious stimuli.34 This has practical applications in assessing analgesia levels and titrating opioid doses, especially in non-communicative patients. Opioids reduce the PUAL via an unknown mechanism. Opioid-induced PUAL reduction was proportionately greater than opioid-induced miosis.35
Inhalational and intravenous anesthetics do not typically depress PRD.11,27,36 Propofol and inhalational anesthetics do decrease PLRA, independent of the baseline pupillary size.37,38 General anesthesia and propofol sedation have been shown to suppress pupillary unrest.39
Anti-emetics used intraoperatively—especially dopamine D2 receptor blockers such as droperidol and metoclopramide—have been shown to significantly depress PRD, signifying the role played by central dopaminergic pathways in the reflex. A similar decrease is not seen with ondansetron.15 Neuromuscular blockers do not affect PRD.40 Anticholinesterase drugs such as neostigmine used for reversal of neuromuscular blockade were found to have no significant effect on pupil size when administered with atropine.41 Nevertheless, another study found that neostigmine reduced the mydriatic effect of intravenous atropine or glycopyrrolate.42 The effects of reversal agents on pupillary reflexes remain unclear.
Other factors
Age-induced miosis alters pupillary reflexes secondary to a decrease in resting pupillary size.12 Factors such as skin tone, eye colour, and subject cooperation can also influence pupillary reflexes.18,43 A number of pathological conditions such as Horner syndrome, Argyll-Robertson pupil (absent light reflex, with normal accommodation reflex), Adie’s pupil (sluggish constriction to light and tonic constriction with slow re-dilation), midbrain/pontine lesions, and pupillary adhesions secondary to uveitis/endophthalmitis can potentially impair pupillary reflexes.8 Baseline pupillometry prior to anesthesia should be performed to exclude these conditions and avoid misinterpretation.
Pupillometry in anesthesia
Guedel historically described pupil size as a factor to define the stages of ether anesthesia, with the beginning of pupillary dilatation indicating an adequate depth for surgery.44 Modern anesthetic agents do not produce significant pupillary dilatation at usual doses.45 They generally produce the opposite, with this miosis associated with inhalational anesthetics likely being due to suppression of inhibitory influences over the EW nucleus.
Inhalational anesthetics do not depress PRD in response to pain.11 Similarly, a total intravenous anesthesia (TIVA) with propofol has no effect on PRD.36 It has been shown that patients with propofol TIVA had a brisk PRD, but still did not move in response to a surgical skin stimulus. Nevertheless, opioids have been shown to produce a dose-related depression of PRD in response to noxious stimuli.34 In a study using TIVA with propofol and remifentanil, suppression of PRD was found to correlate with absence of movement with skin incision.46 Another study in children anesthetized with sevoflurane showed a rapid increase in PD upon skin incision, with alfentanil injection promptly restoring the PD to baseline values.25 Pupillary diameter was a more sensitive measure of noxious stimulus in this study than heart rate, arterial blood pressure, or bispectral index (BIS) monitoring. Furthermore, hemodynamic monitoring, EEG, and BIS monitoring were found to have a longer latency compared with PRD.25 In a study that evaluated pain scores and PRD in response to an electrical pain stimulus with varying concentrations of nitrous oxide, PRD correlated well with the pain signal intensity and the corresponding VAS scores.47 It also decreased in response to increasing nitrous oxide concentration corresponding to decreased nociception. The authors concluded that PRD may be a useful indicator for the central processing of noxious stimuli and the effects of analgesic intervention.47 Table 2 summarizes the studies related to pupillometry use in the perioperative and ICU settings.
Role in combined regional GA
Pupillometry has also been used to assess the efficacy and extent of regional blocks. In a study of patients under GA, PRD was measured using tetanic stimulation at various dermatomes to evaluate the level of blockade by thoracic epidural anesthesia.24 That study showed the feasibility of using PRD to guide thoracic epidural infusion to optimize analgesia. In a study of children receiving sevoflurane combined with regional blocks, failure of regional anesthesia was found to be significantly associated with rapidly increasing PD after skin incision.48 Pupillary reflex dilatation has also been used to detect the level of sensory block in children receiving GA with caudal epidural block to assess effectiveness of epidural analgesia under GA.49 The sensory level was estimated in all subjects using the PRD criteria of 0.2 mm increase from baseline. The authors concluded that a PRD of 0.2 mm may be clinically useful in children over two years of age, and better than temperature differences measured using rapid response infrared thermometry between the dermatomes under GA. Another similar study used PRD to evaluate sciatic nerve blocks.26 Sensory block significantly reduced PRD compared with the non-blocked limb when a tetanic pain stimulus was applied to both limbs. Change in pupillometric parameters have also been shown to positively correlate with the intensity of labour pain measured by the NRS.50 In a study of pain assessment in labouring women, PRD and PLRA were measured along with concomitant recording of NRS. Increases in PD and PLRA were noticed with labour contractions, correlating well with self-reported pain in NRS. The pupillary changes disappeared with epidural analgesia. Measurement of PD without a noxious stimulus to quantify labour pain may be possible because of the intermittent nature of labour pain compared with constant post-surgical pain.51 Pupillary oscillation (i.e., VCPD) has also been shown to better correlate with patient-reported pain scores in labouring women than PD measurements alone are.31
Postoperative pain management
Pupillometry has the potential to quantify postoperative pain and guide opioid therapy, as the PPi (an index derived from the PRD) has been shown to correlate with immediate postoperative pain.28 One study of postoperative pain after general surgical procedures (cholecystectomy, colonic surgery, abdominal wall surgery, upper abdominal surgery, and thyroidectomy) assessed 100 patients using a five-point verbal rating scale, with morphine administered if necessary; concomitant measurement of PRD was performed before and after morphine administration. Pupillary reflex dilatation was correlated with self-reported pain scores and also reliably decreased after morphine administration.52 During the immediate postoperative period, PRD amplitude in response to a constant pressure applied for a ten-second period close to the edge of the skin incision correlated positively with pain quantified by a verbal rating scale. In the same study, morphine analgesia was associated with a decrease in PRD. Thus, PRD may be a potential tool for facilitating postoperative pain management, especially in non-communicative patients. One caveat is that tetanic stimulation to elicit PRD is painful if the patient is awake, so could be used only in anesthetized or sedated patients. Though trends in PRD could guide opioid therapy, the clinical utility of the absolute PRD values in quantifying nociception, especially in cases of constant pain of trauma or cancer, is unclear.
Other pupillary parameters such as PD without a standard noxious stimulus and PLRA have been studied in the context of pain management in the postanesthesia care unit (PACU) without promising results. In an observational study of 103 patients who had surgery under GA, PD was measured at baseline before GA and also after PACU admission.53 Though PD at PACU increased to about 40-80% greater than the baseline value, the only factors that were significantly associated with this increase were time from extubation and intraoperative opioid administration. The authors were not able to show any association of PD with early postoperative pain or pain relief.53 They postulated the residual effect of intraoperative opioids and the lower level of nociceptive stimulation in the PACU as the reasons for their findings. Another cross-sectional study of 145 individuals reported no correlation between PACU pain scores and PD or PLRA.54 The authors concluded that the lower intensity and continuous nature of postoperative pain (unlike the transient pain stimulus used to measure PRD), residual effects of anesthetic agents and concurrent use of medications including anticholinergics and anesthetics could have contributed to their results, insisting on the need for further research.54 In an observational study of 345 patients who received GA, the authors recorded postoperative VAS along with pupillary parameters PD, PLR, and VCPD.31 The ANI was also recorded, which is derived from heart rate variability. The values range from 0 (maximal nociception) to 100 (maximal analgesia), to reflect the balance between analgesia and nociception during GA. The VCPD correlated more strongly with VAS than with ANI, PD, or PLR. The authors concluded that VCPD is a reliable tool to monitor pain in conscious patients. As objective nociception monitors are most useful in patients under anesthesia or sedation, and because anesthetic agents impact pupillary oscillations, its intraoperative application is questionable and requires further study.
Intensive care unit applications of pupillometry
Another important application of pupillometry is assessment of pain in critically ill, mechanically ventilated patients who are often sedated or unconscious. In 37 critically ill patients, the PLRA was found to positively correlate with the behavioural pain scale score following surgical dressing changes.55 A percentage variation in pupil size > 19% in response to light predicted a behavioural pain score (BPS) > 3 with a 100% sensitivity and 77% specificity. The authors concluded that pupillometry might be used to guide pain assessment and adjust analgesia before painful procedures. In another study of deeply sedated and mechanically ventilated patients (n = 34), PRD in response to cutaneous tetanic stimulation was found to be predictive of insufficient analgesia for endotracheal suction.56 Thus, pupillometry may be a non-invasive, rapid technique to assess nociception in critically ill patients for opioid titration. It also helps to ensure adequate analgesia before performing painful procedures. In a proof of concept study of 40 intubated and sedated ICU patients (20 brain injured with either traumatic brain injury /stroke/ subarachnoid hemorrhage [GCS between 7 and 13], and 20 non-brain injured), the authors were able to accurately predict the nociceptive response to endotracheal suctioning using pupillometry performed prior to the suctioning.22 The authors used a stepwise increase in 100 Hz tetanic skin response to elicit a PRD. The PPi was determined by the electrical intensity to increase the pupil size by ≥ 13%. A PPi less than 4 predicted no nociceptive response to suctioning with an 88% sensitivity and 79% specificity. In a similar study in 170 intubated critically ill patients, the PPi was measured prior to nursing interventions. The nursing interventions were classified as painful (BPS > 5) or non-painful (BPS ≤ 5) and correlation with PPi was studied. The PPi was not able to discriminate between painful and non-painful nursing interventions.57
In the ICU, PLR can also be valuable in monitoring brainstem function (especially midbrain function) after cardiac resuscitation, neurotrauma, stroke etc.8,21 Importantly, the pupillary reflex is a brainstem function test that is unaffected by neuromuscular blockers.40
Pupillometer and non-nociceptive central opioid effects
Opioids cause miosis by blocking the neurons that inhibit EW neurons.33 In ten healthy volunteers, pupillary effects of morphine, codeine, and tramadol were studied.58 Morphine and codeine administration resulted in 26% decrease in pupil diameter. Miosis after tramadol administration was delayed up to 150 min after administration. The authors concluded that measurement of pupil diameter may have a place in monitoring the central effects of opioids.33
Patients vary greatly in their response to opioid therapy, so vary in their susceptibility to opioid-induced adverse effects such as respiratory depression. Accordingly, the typical opioid dosing used in clinical practice (based on factors such as body weight, age, and surgery type) is more of a trial-and-error approach. This variability is in part due to genetic factors that affect both pharmacokinetics and pharmacodynamics, although other factors such as previous opioid treatment or abuse may also play a role.
This variable response to opioids has been correlated with quantitative pupillometry readings and has been widely studied (especially with tramadol). Tramadol is a synthetic opioid, and its active metabolite has a higher affinity for μ opioid receptors than the parent drug. In addition, it has norepinephrine and serotonin reuptake inhibiting properties. Accordingly, miosis following tramadol administration occurs late—indicating the action of the active metabolite. This is the predominant response in extensive metabolizers (individuals with normal tramadol metabolism). Poor metabolizers show a lower magnitude of pupillary response attributed to the non-opioid effects of tramadol.59 Pupillary dilatation was even observed in a few poor metabolizers.60
Measurments of PUAL prior to opioid therapy have been correlated to opioid responsiveness. It has been shown that the greater the baseline PUAL, the greater the opioid responsiveness is. The magnitude of PUAL decrease with opioid therapy has also been shown to correlate with the degree of opioid pain relief.29 A case report described a patient receiving perioperative opioid therapy with inadequate pain relief but with significant opioid adverse effects.30 The PUAL was significantly depressed predicting decreased opioid response. Eventually, the patient responded to other analgesic modalities.30 This signifies that patients can experience major opioid adverse effects with inadequate analgesia, and a decrease in PUAL in response to opioids may not always correlate with opioid analgesia. The PUAL is also depressed during GA, which might confound its use intraoperatively.
Limitations of pupillometry
Despite the many potential clinical applications, pupillometry does have some limitations. Conditions such as cataracts, prosthetic eye, periorbital edema, as well as facial or ocular injuries could limit the usefulness of pupillometry.61 Drugs such as anticholinesterases and dopamine receptor blockers can potentially influence pupillary measurements. Even though pupillometry is relatively simple, it is associated with practical difficulties that could hinder application in everyday practice. Ambient light has a significant influence on pupillary measures. Accordingly, the eyes must be shielded from external light before performing pupillometry. This could be difficult to achieve in the operating room setting. Pupillometry cannot be used for continuous monitoring of nociception/analgesia. Intermittent, repeated access to the eyes under the surgical drapes might be challenging and cumbersome in some cases and impossible in others, such as posterior spinal fusion (where the patient is prone). Because of this, it is be hard to use pupillometry to proactively identify and treat pain during painful surgical events. Measurement of PRD requires a standardized noxious stimulus, which is usually a tetanic stimulation. This could be very painful in awake patients, so can only be used in anesthetized, sedated patients and unconscious ICU patients.
Summary and conclusions
A number of pupillometric parameters have been studied in the context of quantifying nociception as well as anti-nociception (e.g., from opioid administration). Most of them measure the balance between sympathetic and parasympathetic influences on pupillary dynamics. The parameters include pupillary diameter, PLR, PRD, PUAL, and VCPD. The pupil dilates in response to acute pain stimulus, but this response eventually fades with constant unrelenting pain. Moreover, PD per se does not correlate well with patient-reported pain scores.31 Opioids and ambient light can significantly influence PD. As PRD it is not influenced by anesthetic agents, it is especially useful intraoperatively to monitor the central nervous system opioid effect. It could also be used to assess the level of regional block using a tetanic skin stimulus. The PPi, a PRD derivative, has similar pros and cons; it needs a light stimulus and is strongly influenced by ambient light and baseline pupil diameter. Opioids do not influence PLRA normalized to pupil size; however, correlation of PLRA to nociception is weak. Inhaled and intravenous anesthetics depress PLRA, rendering its intraoperative use less feasible. Measures of pupillary oscillation such as PUAL and VCPD do not require a tetanic skin stimulus or a light stimulus. They correlate with opioid effects and patient-reported pain scores, but are also suppressed by anesthesia and thus their intraoperative use may be questionable.
The accurate interpretation of each of the pupillometric indices is somewhat controversial, principally because the mechanism behind each index is not fully understood. A common underlying denominator in all pupil dynamics, and thus the pupillometric indices, is the alteration in sympathetic-parasympathetic balance in response to nociception as well as the interventions to mitigate it. The central nervous system effects of opioids can directly impact some of the pupillary parameters (PRD, oscillations; but not PLR) through its action on the EW nucleus. Nevertheless, this may not always be the case (as seen in studies where PRD is used in conjunction with regional blocks). In summary, the jury is still out on what the best pupillary parameter is to pursue in context of nociception and its appropriate interpretation. There is a need for further adequately powered prospective studies. With sufficient robust evidence, pupillometry could potentially be used to personalize perioperative pain management and thus tailor opioid therapy at the bedside.
References
Buvanendran A, Fiala J, Patel KA, Golden AD, Moric M, Kroin JS. The incidence and severity of postoperative pain following inpatient surgery. Pain Med 2015; 16: 2277-83.
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003; 97: 534-40.
Ledowski T. Objective monitoring of nociception: a review of current commercial solutions. Br J Anaesth 2019; 123: e312-21.
Boselli E, Bouvet L, Bégou G, et al. Prediction of immediate postoperative pain using the analgesia/nociception index: a prospective observational study. Br J Anaesth 2014; 112: 715-21.
Won YJ, Lim BG, Kim YS, Lee M, Kim H. Usefulness of surgical pleth index-guided analgesia during general anesthesia: a systematic review and meta-analysis of randomized controlled trials. J Int Med Res 2018; 46: 4386-98.
Edry R, Recea V, Dikust Y, Sessler DI. Preliminary intraoperative validation of the nociception level index: a noninvasive nociception monitor. Anesthesiology 2016; 125: 193-203.
Hall CA, Chilcott RP. Eyeing up the future of the pupillary light reflex in neurodiagnostics. Diagnostics (Basel) 2018; DOI: https://doi.org/10.3390/diagnostics8010019.
Larson MD, Behrends M. Portable infrared pupillometry: a review. Anesth Analg 2015; 120: 1242-53.
Yang LL, Niemann CU, Larson MD. Mechanism of pupillary reflex dilation in awake volunteers and in organ donors. Anesthesiology 2003; 99: 1281-6.
Tauzin-Fin P, Hilbert G, Krol-Houdek M, Gosse P, Maurette P. Mydriasis and acute pulmonary oedema complicating laparoscopic removal of phaechromocytoma. Anaesth Intensive Care 1999; 27: 646-9.
Larson MD, Sessler DI, Washington DE, Merrifield BR, Hynson JA, McGuire J. Pupillary response to noxious stimulation during isoflurane and propofol anesthesia. Anesth Analg 1993; 76: 1072-8.
Loewenfeld IE. Mechanisms of reflex dilatation of the pupil; historical review and experimental analysis. Doc Ophthalmol 1958; 12: 185-448.
Larson MD, Tayefeh F, Sessler DI, Daniel M, Noorani M. Sympathetic nervous system does not mediate reflex pupillary dilation during desflurane anesthesia. Anesthesiology 1996; 85: 748-54.
Larson MD, Talke PO. Effect of dexmedetomidine, an alpha2-adrenoceptor agonist, on human pupillary reflexes during general anaesthesia. Br J Clin Pharmacol 2001; 51: 27-33.
Larson MD. The effect of antiemetics on pupillary reflex dilation during epidural/general anesthesia. Anesth Analg 2003; 97: 1652-6.
Bouma H, Baghuis LC. Hippus of the pupil: periods of slow oscillations of unknown origin. Vision Res 1971; 11: 1345-51.
Larson MD, Berry PD, May J, Bjorksten A, Sessler DI. Latency of pupillary reflex dilation during general anesthesia. J Appl Physiol 1985; 2004(97): 725-30.
Lussier BL, Stutzman SE, Atem F, et al. Distributions and reference ranges for automated pupillometer values in neurocritical care patients. J Neurosci Nurs 2019; 51: 335-40.
Taylor WR, Chen JW, Meltzer H, et al. Quantitative pupillometry, a new technology: normative data and preliminary observations in patients with acute head injury. Technical note. J Neurosurg 2003; 98: 205-13.
Chen JW, Gombart ZJ, Rogers S, Gardiner SK, Cecil S, Bullock RM. Pupillary reactivity as an early indicator of increased intracranial pressure: the introduction of the neurological pupil index. Surg Neurol Int 2011; DOI: https://doi.org/10.4103/2152-7806.82248.
Lussier BL, Olson DM, Aiyagari V. Automated pupillometry in neurocritical care: research and practice. Curr Neurol Neurosci Rep 2019; DOI: https://doi.org/10.1007/s11910-019-0994-z.
Vinclair M, Schilte C, Roudaud F, et al. Using pupillary pain index to assess nociception in sedated critically ill patients. Anesth Analg 2019; 129: 1540-6.
Larson MD, Sessler DI, Ozaki M, McGuire J, Schroeder M. Pupillary assessment of sensory block level during combined epidural/general anesthesia. Anesthesiology 1993; 79: 42-8.
Huybrechts I, Barvais L, Ducart A, Engelman E, Schmartz D, Koch M. Assessment of thoracic epidural analgesia during general anesthesia using pupillary reflex dilation: a preliminary study. J Cardiothorac Vasc Anesth 2006; 20: 664-7.
Constant I, Nghe MC, Boudet L, et al. Reflex pupillary dilatation in response to skin incision and alfentanil in children anaesthetized with sevoflurane: a more sensitive measure of noxious stimulation than the commonly used variables. B J Anaesth 2006; 96: 614-9.
Isnardon S, Vinclair M, Genty C, Hebrard A, Albaladejo P, Payen JF. Pupillometry to detect pain response during general anaesthesia following unilateral popliteal sciatic nerve block: a prospective, observational study. Eur J Anaesthesiol 2013; 30: 429-34.
Guglielminotti J, Grillot N, Paule M, et al. Prediction of movement to surgical stimulation by the pupillary dilatation reflex amplitude evoked by a standardized noxious test. Anesthesiology 2015; 122: 985-93.
Ly-Liu D, Reinoso-Barbero F. Immediate postoperative pain can also be predicted by pupillary pain index in children. Br J Anaesth 2015; 114: 345-6.
Neice AE, Behrends M, Bokoch MP, Seligman KM, Conrad NM, Larson MD. Prediction of opioid analgesic efficacy by measurement of pupillary unrest. Anesth Analg 2017; 124: 915-21.
McKay RE, Neice AE, Larson MD. Pupillary unrest in ambient light and prediction of opioid responsiveness: case report on its utility in the management of 2 patients with challenging acute pain conditions. A A Pract 2018; 10: 279-82.
Charier DJ, Zantour D, Pichot V, et al. Assessing pain using the variation coefficient of pupillary diameter. J Pain 2017; 18: 1346-53.
Rollins MD, Feiner JR, Lee JM, Shah S, Larson M. Pupillary effects of high-dose opioid quantified with infrared pupillometry. Anesthesiology 2014; 121: 1037-44.
Larson MD. Mechanism of opioid-induced pupillary effects. Clin Neurophysiol 2008; 119: 1358-64.
Larson MD, Kurz A, Sessler DI, Dechert M, Bjorksten AR, Tayefeh F. Alfentanil blocks reflex pupillary dilation in response to noxious stimulation but does not diminish the light reflex. Anesthesiology 1997; 87: 849-55.
Bokoch MP, Behrends M, Neice A, Larson MD. Fentanyl, an agonist at the mu opioid receptor, depresses pupillary unrest. Auton Neurosci 2015; 189: 68-74.
Leslie K, Sessler DI, Smith WD, et al. Prediction of movement during propofol/nitrous oxide anesthesia. Performance of concentration, electroencephalographic, pupillary, and hemodynamic indicators. Anesthesiology 1996; 84: 52-63.
Belani KG, Sessler DI, Larson MD, et al. The pupillary light reflex. Effects of anesthetics and hyperthermia. Anesthesiology 1993; 79: 23-7.
Larson MD, Sessler DI, McGuire J, Hynson JM. Isoflurane, but not mild hypothermia, depresses the human pupillary light reflex. Anesthesiology 1991; 75: 62-7.
Behrends M, Larson MD, Neice AE, Bokoch MP. Suppression of pupillary unrest by general anesthesia and propofol sedation. J Clin Monit Comput 2019; 33: 317-23.
Gray AT, Krejci ST, Larson MD. Neuromuscular blocking drugs do not alter the pupillary light reflex of anesthetized humans. Arch Neurol 1997; 54: 579-84.
Balamoutsos NG, Drossou F, Alevizou F, Tjovairi E, Papastephanou C, Marios A. Pupil size during reversal of muscle relaxants. Anesth Analg 1980; 59: 615-6.
Schwartz H, Apt L. Mydriatic effect of anticholinergic drugs used during reversal of nondepolarizing muscle relaxants. Am J Ophthalmol 1979; 88(3 Pt 2): 609-12.
Olson DM, Stutzman S, Saju C, Wilson M, Zhao W, Aiyagari V. Interrater reliability of pupillary assessments. Neurocrit Care 2016; 24: 251-7.
Guedel AE. Inhalation Anesthesia—a Fundamental Guide. The MacMillan Company; 1937: 974-5.
Cullen DJ, Eger EI 2nd, Stevens WC, et al. Clinical signs of anesthesia. Anesthesiology 1972; 36: 21-36.
Barvais L, Engelman E, Eba JM, Coussaert E, Cantraine F, Kenny GN. Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br J Anaesth 2003; 91: 347-52.
Oka S, Chapman CR, Kim B, Nakajima I, Shimizu O, Oi Y. Pupil dilation response to noxious stimulation: effect of varying nitrous oxide concentration. Clin Neurophysiol 2007; 118: 2016-24.
Migeon A, Desgranges FP, Chassard D, et al. Pupillary reflex dilatation and analgesia nociception index monitoring to assess the effectiveness of regional anesthesia in children anesthetised with sevoflurane. Paediatr Anaesth 2013; 23: 1160-5.
Emery J, Ho D, MacKeen L, Heon E, Bissonnette B. Pupillary reflex dilation and skin temperature to assess sensory level during combined general and caudal anesthesia in children. Paediatr Anaesth 2004; 14: 768-73.
Guglielminotti J, Mentre F, Gaillard J, Ghalayini M, Montravers P, Longrois D. Assessment of pain during labor with pupillometry: a prospective observational study. Anesth Analg 2013; 116: 1057-62.
Charier D, Vogler MC, Zantour D, et al. Assessing pain in the postoperative period: Analgesia Nociception Index ™ versus pupillometry. Br J Anaesth 2019; 123: e322-7.
Aissou M, Snauwaert A, Dupuis C, Atchabahian A, Aubrun F, Beaussier M. Objective assessment of the immediate postoperative analgesia using pupillary reflex measurement: a prospective and observational study. Anesthesiology 2012; 116: 1006-12.
Duale C, Julien H, Pereira B, Abbal B, Baud C, Schoeffler P. Pupil diameter during postanesthetic recovery is not influenced by postoperative pain, but by the intraoperative opioid treatment. J Clin Anesth 2015; 27: 23-32.
Kantor E, Montravers P, Longrois D, Guglielminotti J. Pain assessment in the postanaesthesia care unit using pupillometry: a cross-sectional study after standard anaesthetic care. Eur J Anaesthesiol 2014; 31: 91-7.
Lukaszewicz AC, Dereu D, Gayat E, Payen D. The relevance of pupillometry for evaluation of analgesia before noxious procedures in the intensive care unit. Anesth Analg 2015; 120: 1297-300.
Paulus J, Roquilly A, Beloeil H, Théraud J, Asehnoune K, Lejus C. Pupillary reflex measurement predicts insufficient analgesia before endotracheal suctioning in critically ill patients. Crit Care 2013; DOI: https://doi.org/10.1186/cc12840.
Gaillard T, Gergaud S, Grayot CM, François C, Hamel JF, Lasocki S. Can pupillometry diagnose a lack of analgesia prior to nursing in critically ill patients? Intensive Care Med Exp 2015; DOI: https://doi.org/10.1186/2197-425X-3-S1-A326.
Knaggs RD, Crighton IM, Cobby TF, Fletcher AJ, Hobbs GJ. The pupillary effects of intravenous morphine, codeine, and tramadol in volunteers. Anesth Analg 2004; 99: 108-12.
Fliegert F, Kurth B, Göhler K. The effects of tramadol on static and dynamic pupillometry in healthy subjects—the relationship between pharmacodynamics, pharmacokinetics and CYP2D6 metaboliser status. Eur J Clin Pharmacol 2005; 61: 257-66.
Matouskova O, Slanar O, Chytil L, Perlik F. Pupillometry in healthy volunteers as a biomarker of tramadol efficacy. J Clin Pharm Ther 2011; 36: 513-7.
McNett M, Moran C, Janki C, Gianakis A. Correlations between hourly pupillometer readings and intracranial pressure values. J Neurosci Nurs 2017; 49: 229-34.
Rouche O, Wolak-Thierry A, Destoop Q, et al. Evaluation of the depth of sedation in an intensive care unit based on the photo motor reflex variations measured by video pupillometry. Ann Intensive Care 2013; DOI: https://doi.org/10.1186/2110-5820-3-5.
Li D, Miaskowski C, Burkhardt D, Puntillo K. Evaluations of physiologic reactivity and reflexive behaviors during noxious procedures in sedated critically ill patients. J Crit Care 2009; 24(472): e9-13.
Wildemeersch D, Gios J, Jorens PG, Hans GH. Objective nociceptive assessment in ventilated ICU patients: a feasibility study using pupillometry and the nociceptive flexion reflex. J Vis Exp 2018; DOI: https://doi.org/10.3791/57972.
Sabourdin N, Peretout JB, Khalil E, Guye ML, Louvet N, Constant I. Influence of depth of hypnosis on pupillary reactivity to a standardized tetanic stimulus in patients under propofol-remifentanil target-controlled infusion: a crossover randomized pilot study. Anesth Analg 2018; 126: 70-7.
Sabourdin N, Barrois J, Louvet N, et al. Pupillometry-guided intraoperative remifentanil administration versus standard practice influences opioid use: a randomized study. Anesthesiology 2017; 127: 284-92.
Duceau B, Baubillier M, Bouroche G, Albi-Feldzer A, Jayr C. Pupillary reflex for evaluation of thoracic paravertebral block: a prospective observational feasibility study. Anesth Analg 2017; 125: 1342-7.
Author contributions
Senthil Packiasabapathy and Senthilkumar Sadhasivam contributed to all aspects of this manuscript, including study conception and design; acquisition of data; and drafting, editing and revision of the article. Valluvan Rangasamy contributed to acquisition of data and drafting, editing, and revision of the article.
Disclosures
None.
Funding statement
Funding support was provided by the Department of Anesthesia, Indiana University School of Medicine, Indianapolis, Indiana, USA and NIH R01 HD089458 (Principal Investigator: Sadhasivam) and R21 HD094311 (Principal Investigator: Sadhasivam).
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Supplementary material 1 eVideo Hand-held pupillometer is used on an individual to obtain multiple objective pupillometer measures in response to light reflex in real-time. The pupillometer is applied closely over the left eye of the individual (while right eye is closed) to avoid environmental light influence. The pupillometer screen displays different values including maximum, minimum diameters, maximum constriction, and dilation velocity after a light stimulus. (MOV 589 kb)
Rights and permissions
About this article
Cite this article
Packiasabapathy, S., Rangasamy, V. & Sadhasivam, S. Pupillometry in perioperative medicine: a narrative review. Can J Anesth/J Can Anesth 68, 566–578 (2021). https://doi.org/10.1007/s12630-020-01905-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-020-01905-z