Abstract
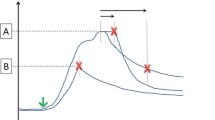
Early brain injury (EBI) during the first 72 h after subarachnoid hemorrhage (SAH) is an important determinant of clinical outcome. A hallmark of EBI, global cerebral ischemia, occurs within seconds of SAH and is thought to be related to increased intracranial pressure (ICP). We tested the hypothesis that ICP elevation and cortical hypoperfusion are the result of physical blockade of cerebrospinal fluid (CSF) flow pathways by cisternal microthrombi. In mice subjected to SAH, we measured cortical blood volume (CBV) using optical imaging, ICP using pressure transducers, and patency of CSF flow pathways using intracisternally injected tracer dye. We then assessed the effects of intracisternal injection of recombinant tissue plasminogen activator (tPA). ICP rose immediately after SAH and remained elevated for 24 h. This was accompanied by a decrease in CBV and impaired dye movement. Intracisternal administration of tPA immediately after SAH lowered ICP, increased CBV, and partially restored CSF flow at 24 h after SAH. Lowering ICP without tPA, by draining CSF, improved CBV at 1 h, but not 24 h after SAH. These findings suggest that blockade of CSF flow by microthrombi contributes to the early decline in cortical perfusion in an ICP-dependent and ICP-independent manner and that intracisternal tPA may reduce EBI and improve outcome after SAH.







Similar content being viewed by others
References
Johanson C, Duncan J, Klinge P, Brinker T, Stopa E, Silverberg G. Multiplicity of cerebrospinal fluid functions: new challenges in health and disease. Cerebrospinal Fluid Res. 2008;5(1):10.
van Gijn J, Kerr RS, Rinkel GJE. Subarachnoid haemorrhage. Lancet. 2007;369(9558):306–18. doi:10.1016/S0140-6736(07)60153-6.
Caner B, Hou J, Altay O, Fuj 2nd M, Zhang JH. Transition of research focus from vasospasm to early brain injury after subarachnoid hemorrhage. J Neurochem. 2012;123 Suppl 2:12–21. doi:10.1111/j.1471-4159.2012.07939.x.
de Rooij NK, Greving JP, Rinkel GJE, Frijns CJM. Early prediction of delayed cerebral ischemia after subarachnoid hemorrhage: development and validation of a practical risk chart. Stroke. 2013; 44(5):1288-94. doi:10.1161/strokeaha.113.001125.
Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, Claassen J, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke. 2002;33(1):200–9. doi:10.1161/hs0102.101080.
Yan J, Li L, Khatibi NH, Yang L, Wang K, Zhang W, et al. Blood–brain barrier disruption following subarchnoid hemorrhage may be faciliated through PUMA induction of endothelial cell apoptosis from the endoplasmic reticulum. Exp Neurol. 2011;230(2):240–7. doi:10.1016/j.expneurol.2011.04.022.
Sarrafzadeh A, Haux D, Sakowitz O, Benndorf G, Herzog H, Kuechler I, et al. Acute focal neurological deficits in aneurysmal subarachnoid hemorrhage: relation of clinical course, CT findings, and metabolite abnormalities monitored with bedside microdialysis. Stroke. 2003;34(6):1382–8. doi:10.1161/01.str.0000074036.97859.02.
Sakowitz OW, Santos E, Nagel A, Krajewski KL, Hertle DN, Vajkoczy P, et al. Clusters of spreading depolarizations are associated with disturbed cerebral metabolism in patients wwith aneurysmal subarachnoid hemorrhage. Stroke. 2013;44(1):220–3. doi:10.1161/strokeaha.112.672352.
Lee J-Y, He Y, Sagher O, Keep R, Hua Y, Xi G. Activated autophagy pathway in experimental subarachnoid hemorrhage. Brain Res. 2009;1287:126–35. doi:10.1016/j.brainres.2009.06.028.
Endo H, Nito C, Kamada H, Yu F, Chan PH. Reduction in oxidative stress by superoxide dismutase overexpression attenuates acute brain injury after subarachnoid hemorrhage via activation of Akt/glycogen synthase kinase-3beta survival signaling. J Cereb Blood Flow Metab. 2007;27(5):975–82. doi:10.1038/sj.jcbfm.9600399.
Westermaier T, Jauss A, Eriskat J, Kunze E, Roosen K. Acute vasoconstriction: decrease and recovery of cerebral blood flow after various intensities of experimental subarachnoid hemorrhage in rats. J Neurosurg. 2009;110(5):996–1002. doi:10.3171/2008.8.JNS08591.
Woernle CM, Winkler KML, Burkhardt J-K, Haile SR, Bellut D, Neidert MC, et al. Hydrocephalus in 389 patients with aneurysm-associated subarachnoid hemorrhage. J Clin Neurosci. 2013;20(6):824–6. doi:10.1016/j.jocn.2012.07.015.
Schubert G, Seiz M, Hegewald A, Manville J, Thomé C. Hypoperfusion in the acute phase of subarachnoid hemorrhage. In: Feng H, Mao Y, Zhang J, editors. Early brain injury or cerebral vasospasm. Acta neurochirurgica supplements. Vienna: Springer; 2011. p. 35–8.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra11. doi:10.1126/scitranslmed.3003748.
Jackowski A, Crockard A, Burnstock G, Russell RR, Kristek F. The time course of intracranial pathophysiological changes following experimental subarachnoid haemorrhage in the rat. J Cereb Blood Flow Metab. 1990;10(6):835–49. doi:10.1038/jcbfm.1990.140.
Wang RK, Jacques SL, Ma Z, Hurst S, Hanson SR, Gruber A. Three dimensional optical angiography. Opt Express. 2007;15(7):4083–97.
Zhang W, Iliff JJ, Campbell CJ, Wang RK, Hurn PD, Alkayed NJ. Role of soluble epoxide hydrolase in the sex-specific vascular response to cerebral ischemia. J Cereb Blood Flow Metab. 2009;29(8):1475–81. doi:10.1038/jcbfm.2009.65.
Jia Y, Alkayed N, Wang RK. Potential of optical microangiography to monitor cerebral blood perfusion and vascular plasticity following traumatic brain injury in mice in vivo. J Biomed Opt. 2009;14(4):040505. doi:10.1117/1.3207121.
Sozen T, Tsuchiyama R, Hasegawa Y, Suzuki H, Jadhav V, Nishizawa S, et al. Role of interleukin-1beta in early brain injury after subarachnoid hemorrhage in mice. Stroke. 2009;40(7):2519–25. doi:10.1161/STROKEAHA.109.549592.
Schubert GA, Seiz M, Hegewald AA, Manville J, Thome C. Acute hypoperfusion immediately after subarachnoid hemorrhage: a xenon contrast-enhanced CT study. J Neurotrauma. 2009;26(12):2225–31. doi:10.1089/neu.2009.0924.
Abbott NJ. Evidence for bulk flow of brain interstitial fluid: significance for physiology and pathology. Neurochem Int. 2004;45(4):545–52. doi:10.1016/j.neuint.2003.11.006.
Preston SD, Steart PV, Wilkinson A, Nicoll JAR, Weller RO. Capillary and arterial cerebral amyloid angiopathy in Alzheimer’s disease: defining the perivascular route for the elimination of amyloid β from the human brain. Neuropathol Appl Neurobiol. 2003;29(2):106–17. doi:10.1046/j.1365-2990.2003.00424.x.
Schubert GA, Poli S, Mendelowitsch A, Schilling L, Thome C. Hypothermia reduces early hypoperfusion and metabolic alterations during the acute phase of massive subarachnoid hemorrhage: a laser-Doppler-flowmetry and microdialysis study in rats. J Neurotrauma. 2008;25(5):539–48. doi:10.1089/neu.2007.0500.
Chung WY, Lee LS. The effect of tissue plasminogen activator (t-PA) on cerebral vasospasm in canine subarachnoid hemorrhage. Zhonghua Yi Xue Za Zhi (Taipei). 1993;52(5):298–306.
Findlay JM, Weir BKA, Kanamaru K, Grace M, Baughman R. The effect of timing of intrathecal fibrinolytic therapy on cerebral vasospasm in a primate model of subarachnoid hemorrhage. Neurosurgery. 1990;26(2):201–6.
Findlay JM, Weir BKA, Steinke D, Tanabe T, Gordon P, Grace M. Effect of intrathecal thrombolytic therapy on subarachnoid clot and chronic vasospasm in a primate model of SAH. J Neurosurg. 1988;69(5):723–35. doi:10.3171/jns.1988.69.5.0723.
Suzuki H, Kanamaru K, Kuroki M, Sun H, Waga S, Miyazawa T. Effects of unilateral intrathecal administrations of low dose tissue-type plasminogen activator on clot lysis, vasospasm and brain phospholipid hydroperoxidation in a primate model of bilateral subarachnoid hemorrhage. Neurol Res. 1998;20(7):625–31.
Asada M, Kong J, Nakamura M, Tamaki N. Thrombolytic therapy with tissue plasminogen activator for prevention of vasospasm in experimental subarachnoid hemorrhage: its efficacy and problems. Neurol Res. 1996;18(4):342–4.
Kawada S, Kinugasa K, Meguro T, Hirotsune N, Tokunaga K, Kamata I, et al. Experimental study of intracisternal administration of tissue-type plasminogen activator followed by cerebrospinal fluid drainage in the ultra-early stage of subarachnoid haemorrhage. Acta Neurochir (Wien). 1999;141(12):1331–8. doi:10.1007/s007010050438.
Brinker T, Seifert V, Dietz H. Subacute hydrocephalus after experimental subarachnoid hemorrhage: its prevention by intrathecal fibrinolysis with recombinant tissue plasminogen activator. Neurosurgery. 1992;31(2):306–11. discussion 11–2.
Brinker T, Seifert V, Stolke D. Effect of intrathecal fibrinolysis on cerebrospinal fluid absorption after experimental subarachnoid hemorrhage. J Neurosurg. 1991;74(5):789–93. doi:10.3171/jns.1991.74.5.0789.
Litrico S, Almairac F, Gaberel T, Ramakrishna R, Fontaine D, Sedat J et al. Intraventricular fibrinolysis for severe aneurysmal intraventricular hemorrhage: a randomized controlled trial and meta-analysis. Neurosurg Rev. 2013;36(4):523–30. doi:10.1007/s10143-013-0469-7.
Kinouchi H, Ogasawara K, Shimizu H, Mizoi K, Yoshimoto T. Prevention of symptomatic vasospasm after aneurysmal subarachnoid hemorrhage by intraoperative cisternal fibrinolysis using tissue-type plasminogen activator combined with continuous cisternal drainage. Neurol Med Chir. 2004;44(11):569–77.
Ramakrishna R, Sekhar LN, Ramanathan D, Temkin N, Hallam D, Ghodke BV, et al. Intraventricular tissue plasminogen activator for the prevention of vasospasm and hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2010;67(1):110–7. doi:10.1227/01.NEU.0000370920.44359.91. discussion 7.
Varelas PN, Rickert KL, Cusick J, Hacein-Bey L, Sinson G, Torbey M, et al. Intraventricular hemorrhage after aneurysmal subarachnoid hemorrhage: pilot study of treatment with intraventricular tissue plasminogen activator. Neurosurgery. 2005;56(2):205–13. discussion −13.
Findlay JM, Jacka MJ. Cohort study of intraventricular thrombolysis with recombinant tissue plasminogen activator for aneurysmal intraventricular hemorrhage. Neurosurgery. 2004;55(3):532–7. discussion 7–8.
Amin-Hanjani S, Ogilvy CS, Barker 2nd FG. Does intracisternal thrombolysis prevent vasospasm after aneurysmal subarachnoid hemorrhage? A meta-analysis. Neurosurgery. 2004;54(2):326–34. discussion 34–5.
Roos YB, Rinkel GJ, Vermeulen M, Algra A, van Gijn J. Antifibrinolytic therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2003;2, CD001245. doi:10.1002/14651858.CD001245.
Hillman J, Fridriksson S, Nilsson O, Yu Z, Säveland H, Jakobsson K-E. Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. J Neurosurg. 2002;97(4):771–8. doi:10.3171/jns.2002.97.4.0771.
Iplikcioglu AC, Berkman MZ. The effect of short-term antifibrinolytic therapy on experimental vasospasm. Surg Neurol. 2003;59(1):10–6. doi:10.1016/S0090-3019(02)00867-4.
Diamond SL, Anand S. Inner clot diffusion and permeation during fibrinolysis. Biophys J. 1993;65(6):2622–43. doi:10.1016/S0006-3495(93)81314-6.
Diamond SL. Engineering design of optimal strategies for blood clot dissolution. Annu Rev Biomed Eng. 1999;1(1):427–61. doi:10.1146/annurev.bioeng.1.1.427.
Conflict of Interest
Dominic A. Siler declares that he has no conflict of interest.
Jorge A. Gonzalez declares that he has no conflict of interest.
Ruikang K. Wang declares that he has no conflict of interest.
Justin S. Cetas declares that he has no conflict of interest.
Nabil J. Alkayed declares that he has no conflict of interest.
All institutional and national guidelines for the care and use of laboratory animals were followed.
Funding Sources
Dominic A. Siler—NHLBI F30 HL108624, Oregon Brain Institute.
Nabil J. Alkayed—NINDS R01 NS044313 and NS070837
Ruikang K. Wang—NHLBI R01 HL093140 and NIBIB R01 EB009682
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siler, D.A., Gonzalez, J.A., Wang, R.K. et al. Intracisternal Administration of Tissue Plasminogen Activator Improves Cerebrospinal Fluid Flow and Cortical Perfusion After Subarachnoid Hemorrhage in Mice. Transl. Stroke Res. 5, 227–237 (2014). https://doi.org/10.1007/s12975-014-0329-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-014-0329-y