Abstract
Purpose of Review
Nanoparticles are crucial for developing patient-/target-specific drug delivery systems. In recent days, mathematical modeling and simulation plays an important role in optimization of various parameters like nanoparticle-based drug dose, dissolution of drug particles, and adverse reaction from the nanoparticles. With the help of modeling and simulation, we can determine or optimize the type, shape, and size of the nanoparticles to be utilized as potential drug delivery system and its influence on the targeted cells/tissues. The main purpose of this review article is to discuss the latest modeling and simulation tools available for developing patient-specific nanoparticle-based drug delivery systems.
Recent Findings
In our current study, we are reporting different mathematical models used for cancer drug delivery systems. It also reports several numerical methods, and simulations models are available for representing nano-drug-bio interactions within the biological systems.
Summary
This review highlights the applications of mathematical modeling and simulation software for developing a rational nano-carrier design and selecting accurate biomaterials for in vivo model.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MP, Acosta-Torres LS, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnology. 2018;16:71. https://doi.org/10.1186/s12951-018-0392-8.
Sahai N, Ahmad N, Gogoi M. Nanoparticles based drug delivery for tissue regeneration using biodegradable scaffolds: a review. Curr Pathobiol Rep. 2018;6:219–24.
Lammers T, Aime S, Hennink WE, Storm G, Kiessling F. Theranostic nanomedicine. Acc Chem Res. 2011;44:1029–38. https://doi.org/10.1021/ar200019c.
Chauhan VP, Jain RK. Strategies for advancing cancer nanomedicine. Nat Mater. 2013;12:958–62.
Psimadas D, Georgoulias P, Valotassiou V, Loudos G. Molecular Nanomedicine Towards Cancer : J Pharm Sci. 2012;101:2271–80. https://doi.org/10.1002/jps.
Pelaz B, Alexiou C, Alvarez-Puebla RA, Alves F, Andrews AM, Ashraf S, et al. Diverse applications of nanomedicine. ACS Nano. 2017;11:2313–81. https://doi.org/10.1021/acsnano.6b06040.
van der Meel R, Sulheim E, Shi Y, Kiessling F, Mulder WJM, Lammers T. Smart cancer nanomedicine. Nat Nanotechnol. 2019;14:1007–17. https://doi.org/10.1038/s41565-019-0567-y.
Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17:20–37.
Tang L, Cheng J. Nonporous silica nanoparticles for nanomedicine application. Nano Today. 2013;8:290–312.
Lee SH, Jun BH. Silver nanoparticles: synthesis and application for nanomedicine. Int J Mol Sci. 2019;20.
Dellinger A, Zhou Z, Connor J, Madhankumar AB, Pamujula S, Sayes CM, et al. Application of fullerenes in nanomedicine: an update. Nanomedicine. 2013;8:1191–208.
Mirza AZ, Siddiqui FA. Nanomedicine and drug delivery: a mini review. Int Nano Lett. 2014;4:94. https://doi.org/10.1007/s40089-014-0094-7.
Clemente-Casares X, Santamaria P. Nanomedicine in autoimmunity. Immunol Lett. 2014;158:167–74.
Moss DM, Siccardi M. Optimizing nanomedicine pharmacokinetics using physiologically based pharmacokinetics modelling. Br J Pharmacol. 2014;171:3963–79.
Moss DM, Siccardi M (2014) Optimising nanomedicine pharmacokinetics using PBPK modelling. Br J Pharmacol 44:n/a-n/a.
Sindhwani S, Syed AM, Ngai J, Kingston BR, Maiorino L, Rothschild J, et al. The entry of nanoparticles into solid tumours. Nat Mater. 2020;19:566–75. https://doi.org/10.1038/s41563-019-0566-2.
• Dogra P, Butner JD, Chuang Y li, et al (2019) Mathematical modeling in cancer nanomedicine: a review Biomed Microdev 21: . doi: https://doi.org/10.1007/s10544-019-0380-2
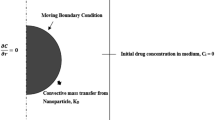
•• Shamsi M, Mohammadi A, Manshadi MKD, Sanati-Nezhad A. Mathematical and computational modeling of nano-engineered drug delivery systems. J Control Release. 2019;307:150–65.
Siepmann J, Siepmann F. Mathematical modeling of drug delivery. Int J Pharm. 2008;364:328–43.
Clancy CE, An G, Cannon WR, Liu Y, May EE, Ortoleva P, et al. Multiscale modeling in the clinic: drug design and development. Ann Biomed Eng. 2016;44:2591–610. https://doi.org/10.1007/s10439-016-1563-0.
Gilad Y, Noy E, Senderowitz H, Albeck A, Firer MA, Gellerman G. Synthesis, biological studies and molecular dynamics of new anticancer RGD-based peptide conjugates for targeted drug delivery. Bioorg Med Chem. 2016;24:294–303. https://doi.org/10.1016/j.bmc.2015.12.020.
Mansoorinasab A, Morsali A, Heravi MM, Beyramabadi SA (2015) Quantum mechanical study on the adsorption of drug gentamicin onto aγ-Fe2 O3 nanoparticles. Orient J Chem 31:1509–1513 . doi: https://doi.org/10.13005/ojc/310329
Xu Z, Wu GM, Li Q, et al. Predictive value of combined LIPS and ANG-2 level in critically ill patients with ARDS risk factors. Mediators Inflamm 2018. 2018. https://doi.org/10.1155/2018/1739615.
Forouzandehmehr M, Shamloo A. Margination and adhesion of micro- and nanoparticles in the coronary circulation: a step towards optimised drug carrier design. Biomech Model Mechanobiol. 2018;17:205–21. https://doi.org/10.1007/s10237-017-0955-x.
Bozsak F, Chomaz JM, Barakat AI. Modeling the transport of drugs eluted from stents: physical phenomena driving drug distribution in the arterial wall. Biomech Model Mechanobiol. 2014;13:327–47. https://doi.org/10.1007/s10237-013-0546-4.
Liu Y, Shah S, Tan J. Computational modeling of nanoparticle targeted drug delivery. Rev Nanosci Nanotechnol. 2012;1:66–83. https://doi.org/10.1166/rnn.2012.1014.
Hossain SS, Hossainy SFA, Bazilevs Y, Calo VM, Hughes TJR. Mathematical modeling of coupled drug and drug-encapsulated nanoparticle transport in patient-specific coronary artery walls. Comput Mech. 2012;49:213–42. https://doi.org/10.1007/s00466-011-0633-2.
Priyadharshini S, Ponalagusamy R. An unsteady flow of magnetic nanoparticles as drug carrier suspended in micropolar fluid through a porous tapered arterial stenosis under non-uniform magnetic field and periodic body acceleration. Comput Appl Math. 2018;37:4259–80. https://doi.org/10.1007/s40314-018-0572-z.
Arifin DY, Lee LY, Wang CH. Mathematical modeling and simulation of drug release from microspheres: implications to drug delivery systems. Adv Drug Deliv Rev. 2006;58:1274–325.
Iordanskii AL, Feldstein MM, Markin VS, Hadgraft J, Plate NA. Modeling of the drug delivery from a hydrophilic transdermal therapeutic system across polymer membrane. Eur J Pharm Biopharm. 2000;49:287–93. https://doi.org/10.1016/S0939-6411(00)00063-1.
Swierniak A, Kimmel M, Smieja J. Mathematical modeling as a tool for planning anticancer therapy. Eur J Pharmacol. 2009;625:108–21.
Wang Z, Deisboeck TS. Mathematical modeling in cancer drug discovery. Drug Discov Today. 2014;19:145–50.
Sanga S, Sinek JP, Frieboes HB, Ferrari M, Fruehauf JP, Cristini V. Mathematical modeling of cancer progression and response to chemotherapy. Expert Rev Anticancer Ther. 2006;6:1361–76. https://doi.org/10.1586/14737140.6.10.1361.
Sun X, Hu B. Mathematical modeling and computational prediction of cancer drug resistance. Brief Bioinform. 2017;19:1382–99. https://doi.org/10.1093/bib/bbx065.
Kim MJ, Gillies RJ, Rejniak KA (2013) Current advances in mathematical modeling of anti-cancer drug penetration into tumor tissues. Front. Oncol. 3 NOV.
Beerenwinkel N, Schwarz RF, Gerstung M, Markowetz F. Cancer evolution: mathematical models and computational inference. Syst Biol. 2015;64:e1–e25. https://doi.org/10.1093/sysbio/syu081.
Ozdemir-Kaynak E, Qutub AA, Yesil-Celiktas O. Advances in glioblastoma multiforme treatment: new models for nanoparticle therapy. Front Physiol. 2018;9.
Serre R, Benzekry S, Padovani L, et al. Mathematical modeling of cancer immunotherapy and its synergy with radiotherapy. In: Cancer Research; 2016. p. 4931–40.
Leder K, Pitter K, Laplant Q, et al. Mathematical modeling of pdgf-driven glioblastoma reveals optimized radiation dosing schedules. Cell. 2014;156:603–16. https://doi.org/10.1016/j.cell.2013.12.029.
Dell’Orco D, Lundqvist M, Oslakovic C, et al. Modeling the time evolution of the nanoparticle-protein corona in a body fluid. PLoS One. 2010;5:e10949. https://doi.org/10.1371/journal.pone.0010949.
Dell’Orco D, Lundqvist M, Cedervall T, Linse S. Delivery success rate of engineered nanoparticles in the presence of the protein corona: a systems-level screening. Nanomedicine. 2012;8:1271–81. https://doi.org/10.1016/j.nano.2012.02.006.
Darabi Sahneh F, Scoglio C, Riviere J. Dynamics of nanoparticle-protein corona complex formation: analytical results from population balance equations. PLoS One. 2013;8:e64690. https://doi.org/10.1371/journal.pone.0064690.
Lopez H, Lobaskin V. Coarse-grained model of adsorption of blood plasma proteins onto nanoparticles. J Chem Phys. 2015:143. https://doi.org/10.1063/1.4936908.
Tavanti F, Pedone A, Menziani MC. A closer look into the ubiquitin corona on gold nanoparticles by computational studies. New J Chem. 2015;39:2474–82. https://doi.org/10.1039/c4nj01752h.
Gentile F, Ferrari M, Decuzzi P. The transport of nanoparticles in blood vessels: the effect of vessel permeability and blood rheology. Ann Biomed Eng. 2008;36:254–61. https://doi.org/10.1007/s10439-007-9423-6.
Tsoi KM, Macparland SA, Ma XZ, et al. Mechanism of hard-nanomaterial clearance by the liver. Nat Mater. 2016;15:1212–21. https://doi.org/10.1038/nmat4718.
Lee TR, Choi M, Kopacz AM, Yun SH, Liu WK, Decuzzi P. On the near-wall accumulation of injectable particles in the microcirculation: smaller is not better. Sci Rep. 2013;3. https://doi.org/10.1038/srep02079.
Müller K, Fedosov DA, Gompper G. Margination of micro- and nano-particles in blood flow and its effect on drug delivery. Sci Rep. 2014;4. https://doi.org/10.1038/srep04871.
Fullstone G, Wood J, Holcombe M, Battaglia G. Modelling the transport of nanoparticles under blood flow using an agent-based approach. Sci Rep. 2015:5. https://doi.org/10.1038/srep10649.
Gaohua L, Abduljalil K, Jamei M, Johnson TN, Rostami-Hodjegan A. A pregnancy physiologically based pharmacokinetic (p-PBPK) model for disposition of drugs metabolized by CYP1A2, CYP2D6 and CYP3A4. Br J Clin Pharmacol. 2012;74:873–85. https://doi.org/10.1111/j.1365-2125.2012.04363.x.
Decuzzi P, Ferrari M. The receptor-mediated endocytosis of nonspherical particles. Biophys J. 2008;94:3790–7. https://doi.org/10.1529/biophysj.107.120238.
Yuan H, Zhang S. Effects of particle size and ligand density on the kinetics of receptor-mediated endocytosis of nanoparticles. Appl Phys Lett. 2010:96. https://doi.org/10.1063/1.3293303.
Dogra P, Adolphi NL, Wang Z, Lin YS, Butler KS, Durfee PN, et al. Establishing the effects of mesoporous silica nanoparticle properties on in vivo disposition using imaging-based pharmacokinetics. Nat Commun. 2018:9. https://doi.org/10.1038/s41467-018-06730-z.
Chauhan VP, Stylianopoulos T, Martin JD, Popović Z, Chen O, Kamoun WS, et al. Normalization of tumour blood vessels improves the delivery of nanomedicines in a size-dependent manner. Nat Nanotechnol. 2012;7:383–8. https://doi.org/10.1038/nnano.2012.45.
Hendriks BS, Reynolds JG, Klinz SG, Geretti E, Lee H, Leonard SC, et al. Multiscale kinetic modeling of liposomal doxorubicin delivery quantifies the role of tumor and drug-specific parameters in local delivery to tumors. CPT Pharmacometrics Syst Pharmacol. 2012;1. https://doi.org/10.1038/psp.2012.16.
Frieboes HB, Wu M, Lowengrub J, Decuzzi P, Cristini V. A computational model for predicting nanoparticle accumulation in tumor vasculature. PLoS One. 2013;8:e56876. https://doi.org/10.1371/journal.pone.0056876.
Stapleton S, Milosevic M, Allen C, Zheng J, Dunne M, Yeung I, et al. A mathematical model of the enhanced permeability and retention effect for liposome transport in solid tumors. PLoS One. 2013;8. https://doi.org/10.1371/journal.pone.0081157.
Sykes EA, Dai Q, Sarsons CD, Chen J, Rocheleau JV, Hwang DM, et al. Tailoring nanoparticle designs to target cancer based on tumor pathophysiology. Proc Natl Acad Sci U S A. 2016;113:E1142–51. https://doi.org/10.1073/pnas.1521265113.
Pascal J, Ashley CE, Wang Z, Brocato TA, Butner JD, Carnes EC, et al. Mechanistic modeling identifies drug-uptake history as predictor of tumor drug resistance and nano-carrier-mediated response. ACS Nano. 2013;7:11174–82. https://doi.org/10.1021/nn4048974.
Leonard F, Curtis LT, Yesantharao P, Tanei T, Alexander JF, Wu M, et al. Enhanced performance of macrophage-encapsulated nanoparticle albumin-bound-paclitaxel in hypo-perfused cancer lesions. Nanoscale. 2016;8:12544–52. https://doi.org/10.1039/c5nr07796f.
Wang Z, Kerketta R, Chuang YL, Dogra P, Butner JD, Brocato TA, et al. Theory and experimental validation of a spatio-temporal model of chemotherapy transport to enhance tumor cell kill. PLoS Comput Biol. 2016;12. https://doi.org/10.1371/journal.pcbi.1004969.
Miller HA, Frieboes HB. Evaluation of drug-loaded gold nanoparticle cytotoxicity as a function of tumor vasculature-induced tissue heterogeneity. Ann Biomed Eng. 2019;47:257–71. https://doi.org/10.1007/s10439-018-02146-4.
Laomettachit T, Puri IK, Liangruksa M. A two-step model of TiO2 nanoparticle toxicity in human liver tissue. Toxicol Appl Pharmacol. 2017;334:47–54. https://doi.org/10.1016/j.taap.2017.08.018.
Saeedi M, Vahidi O, Goodarzi V, Saeb MR, Izadi L, Mozafari M. A new prospect in magnetic nanoparticle-based cancer therapy: taking credit from mathematical tissue-mimicking phantom brain models. Nanomedicine. 2017;13:2405–14. https://doi.org/10.1016/j.nano.2017.07.013.
Chaudhuri A, Battaglia G, Golestanian R. The effect of interactions on the cellular uptake of nanoparticles. Phys Biol. 2011;8. https://doi.org/10.1088/1478-3975/8/4/046002.
Ghaghada KB, Saul J, Natarajan JV, Bellamkonda RV, Annapragada AV. Folate targeting of drug carriers: a mathematical model. J Control Release. 2005;104:113–28. https://doi.org/10.1016/j.jconrel.2005.01.012.
Salvati A, Åberg C, dos Santos T, Varela J, Pinto P, Lynch I, et al. Experimental and theoretical comparison of intracellular import of polymeric nanoparticles and small molecules: toward models of uptake kinetics. Nanomedicine. 2011;7:818–26. https://doi.org/10.1016/j.nano.2011.03.005.
Mukherjee SP, Byrne HJ. Polyamidoamine dendrimer nanoparticle cytotoxicity, oxidative stress, caspase activation and inflammatory response: experimental observation and numerical simulation. Nanomedicine. 2013;9:202–11. https://doi.org/10.1016/j.nano.2012.05.002.
Sorrell I, Shipley RJ, Hearnden V, Colley HE, Thornhill MH, Murdoch C, et al. Combined mathematical modelling and experimentation to predict polymersome uptake by oral cancer cells. Nanomedicine. 2014;10:339–48. https://doi.org/10.1016/j.nano.2013.08.013.
Johannsen M, Gneveckow U, Thiesen B, Taymoorian K, Cho CH, Waldöfner N, et al. Thermotherapy of prostate cancer using magnetic nanoparticles: feasibility, imaging, and three-dimensional temperature distribution. Eur Urol. 2007;52:1653–62. https://doi.org/10.1016/j.eururo.2006.11.023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nanoparticle-based Drug Delivery
Rights and permissions
About this article
Cite this article
Sahai, N., Gogoi, M. & Ahmad, N. Mathematical Modeling and Simulations for Developing Nanoparticle-Based Cancer Drug Delivery Systems: A Review. Curr Pathobiol Rep 9, 1–8 (2021). https://doi.org/10.1007/s40139-020-00219-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40139-020-00219-5