Abstract
Purpose
A recent survey has shown that the COVID-19 pandemic has culminated in dramatical and critical treatment particularly in acute infected patients. In fact, this systematic review-meta-analysis was directly pertained to estimation at the efficient value of some clinical managements to confront the COVID-19 infection.
Methods
Pubmed, Embase, Scopus, Cochrane, and Scholar databases were searched from inception to July 1, 2020, to identify studies reporting the current treatment process and medications (e.g. hydroxychloroquine, antiviral therapy, convalescent plasma, and immunomodulatory agents) for COVID-19. A random-effects model meta-analysis was performed to calculate the relative risk (RR) with 95% confidence intervals (CI). The outcomes of this study were the frequency of negative conversion cases, clinical improvements, mechanical ventilation demand, intensive care unit (ICU) entry, and mortality. The standard treatment refers to the published guidelines and specialist experience which varies in different articles, and the proposed treatment refers to the kind of interest suggested in the included studies.
Results
A number of 45 articles met the eligibility criteria (out of 6793 articles). Among them, 26 articles involving 3263 patients were included in quantitative analysis. Anti-COVID-19 interventions could significantly increase clinical improvement (RR 1.17, 95% CI 1.08–1.27; I2 = 49.8%) and reduce the mortality rate (RR 0.58, 95% CI 0.35–0.95; I2 = 74.8%). Although in terms of negative conversion, ICU entry, and mechanical ventilation demand, clinical intervention had no beneficial effect. The clinical effect of immunomodulatory agents (especially tocilizumab and anakinra) was noticeable compared to other medications with RR of 0.22 (95% CI 0.09–0.53; I2 = 40.9%) for mortality and 1.25 (95% CI 1.07–1.46; I2 = 45.4%) for clinical improvement. Moreover, Antivirals (RR 1.13, 95% CI 1.01–1.26; I2 = 47.0%) and convalescent plasma therapy (RR 1.41, 95% CI 1.01–1.98; I2 = 66.6%) had significant beneficial effects on clinical improvement.
Conclusion
Based on our findings, all the included interventions significantly declined the mortality and enhanced clinical improvements with no effect on negative conversion and mechanical ventilation demand. Especially, immunomodulators and plasma therapy showed favorable outcomes.
Graphical abstract

An evaluation on the efficacy of proposed treatment against COVID-19.
Similar content being viewed by others
Introduction
The newly discovered coronavirus pathogenesis (SARS-CoV-2) has been prevalently broken out as an unprecedented epidemic public health emergency since January 30, 2020 and then it was announced globally as a pandemic on March 11, 2020 by the World Health Organization (WHO). In fact, the high rate of human to human transmission of this virus as quickly as its rapid spreading contagion aggravated the complexity of the situation [1,2,3,4]. SARS-CoV-2, has already infected nearly 14.5 million people worldwide resulting in 607,781 deaths in 216 countries, as of July 21, 2020 [5]. The percentage of mortality attributed to COVID-19 has fallen from 8.1% during week 27 to 6.4% during week 28 (July 11, 2020) but remained above baseline. The overall cumulative hospitalization rate is 113.6 per 100,000 which is a huge burden to the healthcare system [6]. Besides the public health issues, it was stated that COVID-19 prevalence would have considerable effect on the health market especially the pharmaceutical sector [7].
SARS-CoV-2 brings about a condition in which clinical manifestations start with fever, dry cough, or occasional shortness of breath and in some cases acute respiratory distress syndrome (ARDS), multi-organ failure, and death [8]. Ling Lin et al. (2020) suggested a rational hypothetical pathogenesis of SARS-CoV-2 infection that implies virus interaction with angiotensin converting enzyme 2 (ACE2) expressed in target organs subsequent to the passage through the mucous membranes and entrance to peripheral blood from the lungs [9]. Unfortunately, at this juncture, there is no specific medication or clinical approach to managing patients with COVID-19. However, besides the attempts to introduce new vaccines or therapeutic agents, many different clinical trials have been launched to evaluate the efficacy of different existing medications and clinical managements like antiviral drugs, antimalarial drugs, immunomodulatory drugs, stem cell therapy, convalescent plasma therapy and etc. [10,11,12,13,14,15]. Some of these trials terminated with the beneficial influences on patients’ outcomes [10, 12, 16] and some did not [8, 14, 17]. Because of these contradictory reports, there is conflict on the question of which these available interventions could be more affirmatively efficacious and acceptable. Considering that it has been a short time since the SARS-CoV-2 outbreak, most of the reported investigations have limited yields and incomplete bodies of data. In such a pandemic emergency situation, it is mandatory to provide a general overview of current management effectiveness to achieve the best strategy against COVID-19. Furthermore, SARS-CoV-2 is a RNA virus so that its fast mutation can result in a resistance phenotype [18]. Blind medication could trigger the emergence of resistance phenotype as well [18], thus rapid determination of the best clinical approach is necessary.
There have been several systematic review-meta-analyses about COVID-19 that investigated underlying disease and comorbidities, clinical manifestations and imaging findings, paraclinical factors and biomarkers, mortality rate, maternal outcomes and etc. [19,20,21,22,23,24]. Although some systematic reviews were published in the field of therapeutic options against COVID-19 and summarized the trials with inconclusive outcomes [25,26,27,28,29,30]. Zhong et al., provided a systematic review and meta-analysis including the therapies for severe acute respiratory syndrome (SARS), Middle Eastern respiratory syndrome (MERS) mainly besides COVID-19 and assessed their safety and efficacy profiles [31]. Due to daily update of studies regarding anti-COVID-19 interventions, it is mandatory to conduct a comprehensive and updated review on this field. In this study, we conducted a systematic review and meta-analysis to synthesize the results of well-done observational studies and clinical trials to estimate the value of some clinical managements to confront COVID-19.
Methods
The study protocol was approved by the Ethics Review Committee in Research Deputy Department of Shahid Beheshti University of Medical Sciences, Tehran, Iran (REC code, IR.SBMU.RETECH.REC.1399.052).
Search strategy
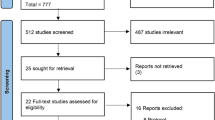
The Cochrane protocol was used to conduct the systematic review [32] and search the databases which were performed and based on the PRISMA guideline (Fig. 1) [33]. International databases consisting of Scopus, PubMed, Cochrane, and Embase were applied to search for the articles from inception to July 1, 2020. The following keywords and MeSH terms consist of: “treatment” OR “therapy” OR “COVID-19 drug treatment” OR “COVID-19 serotherapy” OR “Hydroxy chloroquine” OR “Antiviral Agents” OR “Immunomodulation” OR “plasma” were combined with “COVID-19” OR “severe acute respiratory syndrome coronavirus 2”. The search strategy was attached to the supplementary section. The reference list of all identified documents was also scrutinized due to recognizing the surplus potential eligible studies.
Inclusion and exclusion criteria and outcomes
All types of studies i.e. randomized controlled trials (RCTs), prospective or retrospective cohort studies, and the case series that investigated clinical outcomes and/or viral clearance among adult patients were included to conduct this study. All studies were carried out qualitatively and among them only controlled cohort survives and RCTs were totally used to perform meta-analysis. Meanwhile, studies with these characteristics were excluded: (a) duplicate publications (b) full text in non-English language (c) reviews, letters, conferences, case reports and correspondence (d) descriptive studies about various medications (e) recommendations and guidelines (f) about herbal medicine (g) about vaccines and (h) description on clinical and imaging findings. However, few articles which are still in press also picked out for the analysis to provide the aim of this study. Other steps that must be taken into consideration are presented in Fig. 1. The outcomes of this study were the frequency of negative conversion cases, clinical improvements, mechanical ventilation demand, intensive care unit (ICU) entry, and finally mortality. The standard treatment refers to the published guidelines and specialist experience which varies in different articles, and the proposed treatment refers to the kind of interest suggested in the included studies.
Data extraction and quality assessment
Data extraction standard forms including study characteristics (country, year, type of study), population characterization (total number of cases, sex ratio, mean age, coexisting conditions), intervention characterization (type of treatment provided, days from disease onset to clinical intervention), and outcomes (number of cases needed mechanical ventilation, number of cases need ICU, number of cases with negative conversion, time to negative conversion, time to clinical improvement, and mortality) were filled independently by three investigators. Discrepancies were resolved by the consensus and the final decision of the corresponding author [34]. Clinical improvement was defined according to the seven-point ordinal scales as followed: 1, death; 2, receiving invasive mechanical ventilation; 3, receiving high-flow oxygen; 4, receiving low-flow oxygen; 5 or 6, breathing ambient air; and 7, discharging [35]. The methodological quality of the included studies was assessed independently by two reviewers using Cochrane’s risk of bias tool for RCTs [36], Newcastle-Ottawa Quality Assessment Scale for controlled retrospective studies [37], and NIH Quality Assessment Tool for case series [38].
Statistical analysis
We conducted a meta-analysis by utilization of STATA software version 14.0. The DerSimonian and Laird random-effects meta-analysis methods were used to calculate the relative risk (RR) with 95% confidence interval (CIs) for the efficacy of interventions in RCTs and controlled retrospective studies [39, 40]. In addition, Cochrane’s Q-test and I2 index were used for determining heterogeneity [41,42,43]. When I2 index was lower than 50%, the fixed effect model was used and if I2 index was higher than 50%, the random effect model was utilized [41, 44,45,46,47]. Publication bias was detected using Egger’s test [41,42,43].
Result
Search results
At the end of the search process, 6795 records were retrieved through Pubmed, Embase, Scopus, Cochrane and Scholar searching. After the removal of 1489 duplicated cases, 5304 records remained. At the next step, all the remaining records were screened by investigators, and among them, 3887 studies were removed, because of their irrelevance with COVID-19 treatment. Of the 1417 records, 45 cases met the eligibility criteria, and others were excluded because of the reasons mentioned in Fig. 1. Thus the number of remaining studies included in qualitative synthesis was 45 consist of 11 case series, 15 cohort studies, and 19 RCTs. Among them 26 studies involving 3263 patients were synthesized quantitatively consist of 12 cohort studies and 14 RCTs, subsequently.
Characteristics of included studies
The 45 included studies were categorized in five groups including studies reporting the efficacy of (1) antimalarial agent [8, 48, 49]; (2) antimalarial agent plus antibiotic [10, 50,51,52,53,54]; (3) plasma therapy [11, 55,56,57,58,59,60]; (4) antiviral agents [14,15,16, 35, 49, 53, 54, 61,62,63,64,65,66,67,68,69,70,71,72]; (5) immunomodulatory agents [12, 71,72,73,74,75,76,77,78,79,80,81,82,83,84]. On the whole, 24 studies were performed in china, seven in Italy, four in France, three in the U.S., two in Korea, one in Iran, one in Hong Kong and Qatar, and two were conducted internationally in Germany, Hong Kong, Italy, USA, Singapore, Spain, Taiwan Japan, and France. Two out of four studies evaluating hydroxychloroquine (HCQ), four out of six studies evaluating HCQ plus azithromycin (AZM), six out of seven studies evaluating plasma therapy, four out of ten studies evaluating antiviral agents, and 11 out of 14 studies evaluating immunomodulatory agents reported crucially affirmative effects of intervention. The comparison of all these medical categories were summarized in supplementary material (Table S1). Quality assessment of included studies was also summarized in supplementary material (Table S2, S3, S4).
Meta-analysis
The frequency of negative conversion cases
We pooled the number of 20 studies (including 1141 patients) in a random effect meta-analysis. An overall pooled RR of 1.15 (95% CI 0.92–1.43, I2 = 75.1%) was obtained for the negative conversion which demonstrated that clinical interventions resulted in non-significant increase in positive-to-negative conversion in patients with COVID-19. In subgroup analysis, there was only one study on HCQ (RR 4.57, 95% CI 1.16–18.05) and one study on convalescent plasma (CP) (RR 2.68, 95% CI 1.71–4.20) that reported a significant increase of negative conversion. Moreover, patients who received HCQ plus AZM had a non-significant increase in negative conversion (RR 3.24, 95% CI 0.71–14.74; I2 = 56.6%) (Fig. 2).
Random-effects meta-analysis of the proposed treatment efficacy on the frequency of negative conversion cases relative risk in controlled retrospective and clinical trial studies. RR: relative risk, Event Treatment: Proposed treatment, Event Control: Standard treatment, HCQ: Hydroxychloroquine, AZM: Azithromycin, CP: Convalescent plasma, LPV/r: Lopinavir and Ritonavir, ARB: Arbidol, FAV: Favipiravir, BXM: Baloxavir marboxil, IFN: Interferon, MPZ: Meplazumab, RUX: Ruxolitinib
Clinical improvement
Analysis of 22 studies (including 1462 patients) revealed that, proposed interventions led to a significant increase in clinical improvement (RR 1.17, 95% CI 1.08–1.27; I2 = 49.8%). Based on subgroup analysis, CP (RR 1.41, 95% CI 1.01–1.98; I2 = 66.6%), immunomodulatory agents (RR 1.25, 95% CI 1.07–1.46; I2 = 45.4%), and antivirals (RR 1.13, 95% CI 1.01–1.26; I2 = 47%) showed a notable benefit in this outcome. HCQ-treated group observed the same rate of clinical improvement with standard care group (RR 1.04, 95% CI 0.85–1.28; I2 = 79.3%). There was only one study on HCQ plus AZM excluded which ended up in treatment of all patients in both intervention and control groups (Fig. 3).
Random-effects meta-analysis of the proposed treatment efficacy on the clinical improvement relative risk in controlled retrospective and clinical trial studies. RR: relative risk, Event Treatment: Proposed treatment, Event Control: Standard treatment, HCQ: Hydroxychloroquine, AZM: Azithromycin, CP: Convalescent plasma, LPV/r: Lopinavir and Ritonavir, ARB: Arbidol, FAV: Favipiravir, BXM: Baloxavir marboxil, RDV: Remdesivir, mPRED: Methylprednisolone, IFN: Interferon, BARI: Baricitinib, MPZ: Meplazumab, RUX: Ruxolitinib, ANR: Anakinra, TCZ: Tocilizumab
Mechanical ventilation demand
There were 18 studies (2719 patients) reported data on mechanical ventilation. The overall pooled RR indicated that the interventions could not affect this demand (RR 1.16, 95% CI 0.87–1.54; I2 = 73.5%). Although, subgroup analysis illustrated decreased mechanical ventilation need after the administration of immunomodulatory agents (especially anakinra) (RR 0.75, 95% CI 0.31–1.81; I2 = 38.2%) and antivirals (especially remdesivir and baloxavir marboxil) (RR 0.9, 95% CI 0.73–1.1; I2 = 6.9%) with no significant difference. Surprisingly, HCQ in one study observed more incidence of mechanical ventilation in patients with COVID-19 (RR 2.31, 95% CI 1.39–3.84). (Fig. 4).
Random-effects meta-analysis of the proposed treatment efficacy on the mechanical ventilation demand relative risk in controlled retrospective and clinical trial studies. RR: relative risk, Event Treatment: Proposed treatment, Event Control: Standard treatment, HCQ: Hydroxychloroquine, AZM: Azithromycin, CP: Convalescent plasma, LPV/r: Lopinavir and Ritonavir, ARB: Arbidol, FAV: Favipiravir, RDV: Remdesivir, BXM: Baloxavir marboxil, IFN: Interferon, RUX: Ruxolitinib, ANR: Anakinra, TCZ: Tocilizumab
ICU entry
Overall pooled RR in 16 studies (2116 patients) indicated that all interventions led to an increase in ICU entrance (RR 2.55, 95% CI 1.31–4.97; I2 = 57.7%) except immunomodulatory agents (especially tocilizumab) which resulted in a non-significant reduction (RR 0.73, 95% CI 0.02–26.69; I2 = 86.7%) (Fig. 5).
Random-effects meta-analysis of the proposed treatment efficacy on the ICU entry relative risk in controlled retrospective and clinical trial studies. RR: relative risk, Event Treatment: Proposed treatment, Event Control: Standard treatment, HCQ: Hydroxychloroquine, AZM: Azithromycin, CP: Convalescent plasma, LPV/r: Lopinavir and Ritonavir, ARB: Arbidol, FAV: Favipiravir, BXM: Baloxavir marboxil, IFN: Interferon, RUX: Ruxolitinib, BARI: Baricitinib, ANR: Anakinra, TCZ: Tocilizumab
Mortality
Mortality was reported in 24 studies (2961 patients). The overall pooled results indicated that included therapeutics could significantly reduce the mortality rate in patients with COVID-19 (RR 0.58, 95% CI 0.35–0.95; I2 = 74.8%). In subgroup analysis, immunomodulatory agents (especially tocilizumab and anakinra) significantly decreased this rate (RR 0.22, 95% CI 0.09–0.53; I2 = 40.9%). Moreover, antivirals (especially lopinavir/ritonavir) and CP observed a non-significant reduction in mortality with RR of 0.83 (95% CI 0.55–1.24) and 0.52 (95% CI 0.26–1.03), respectively. Also, HCQ plus AZM had no effect on this outcome (RR 0.99, 95% CI 0.18–5.34; I2 = 80.1%). On the contrary, only one study on HCQ demonstrated higher mortality tendency in the patients (RR 1.57, 95% CI 1.03–2.39) (Fig. 6).
Random-effects meta-analysis of the proposed treatment efficacy on the mortality relative risk in controlled retrospective and clinical trial studies. RR: relative risk, Event Treatment: Proposed treatment, Event Control: Standard treatment, HCQ: Hydroxychloroquine, AZM: Azithromycin, CP: Convalescent plasma, LPV/r: Lopinavir and Ritonavir, RDV: Remdesivir, ARB: Arbidol, FAV: Favipiravir, BXM: Baloxavir marboxil, IFN: Interferon, MPZ: Meplazumab, RUX: Ruxolitinib, mPRED: Methylprednisolone, ANR: Anakinra, TCZ: Tocilizumab
Publication bias
The Egger’s test showed a significant publication bias in term of positive-to-negative conversion (Coefficient = −2.71, p value <0.001) and clinical improvement (Coefficient = −1.40, p value = 0.004). Publication bias in other subgroups including need for mechanical ventilation (Coefficient = −0.54, p value =0.35), ICU entry (Coefficient 2.31, p value = 0.131), and mortality (Coefficient = 0.44, p value = 0.514) was not significant.
Discussion
Despite a several months passed after the presentation of SARS-CoV-2 outbreak, no effective treatment has been submitted and there is still conflict on the efficacy of various treatments. In this pandemic situation, off-label prescription is rational and may lead to establish an effective clinical management strategy [85]. To evaluate the efficacy of current clinical managements against COVID-19 we conducted a literature review focusing on patient outcomes.
Antimalarial agents
Chloroquine (CQ), an antimalarial 4-aminoquinoline, and its derivative hydroxychloroquine (HCQ) have been used for the treatment and prevention of malaria and also autoimmune disorders such as lupus and rheumatoid arthritis due to anti-inflammatory properties [86]. This class of medications acts through some mechanisms against SARS-CoV-2 as follows [87]: prevent virus attachment to the host cell by reducing the glycosylation of ACE2, inhibition of virus internalization and fusion with lysosomes by increasing the pH in these organelles, and block the production of interleukin-6 and other pro-inflammatory cytokines, which are key mediators of ARDS and cytokine storm. It was truly suggested that CQ and HCQ have beneficial effects in patients with COVID-19 [48, 88], although some other studies reported not only the ineffectiveness of CQ or HCQ but also their adverse effects in the patients with COVID-19 [8, 89]. According to our qualitative synthesize, in terms of HCQ with or without AZM, the results were contradictory. It seems that the early administration of HCQ would decrease the rate of hospitalized patient mortality in mild patients [52]. However, Rosenberg et al., by the study of nearly 1000 patients (34% were moderate to severe patients) as the same our findings reported no benefit of HCQ in this outcome [51]. Although, only one study showed that HCQ had superior ability in viral clearance, other outcomes were not affected by the administration of antimalarial agents or even deteriorated. We assumed that it might be due to the heterogeneity in the demographic and clinical characteristics of patients assessed in this study, as authors expressed that patients receiving HCQ were more likely to be male, obese, and diabetic. Some other studies were also reported the ineffectiveness of HCQ [90,91,92]. However, the small sample size of the related studies could not produce reliable conclusions. Considering previous studies and our findings, HCQ with or without AZM does not seem to be effective in treating patients with severe COVID-19.
Antiviral therapies
The current recommended Antiviral agents are mainly based on previous experience showing clinical benefits in treating influenza, Ebola, MERS, SARS, and other viral infections [93]. The efficacy of lopinavir/ritonavir (as an anti-HIV agent), Arbidol, favipiravir, and remdesivir were mostly assessed in this category of medications. These agents share common mechanisms of action against COVID-19, namely the inhibition of cell entry, RNA replication process, and some other post-entry steps [18, 66, 94,95,96]. It was proposed that some antivirals, including neuraminidase inhibitors (e.g., oseltamivir), ganciclovir, acyclovir, and ribavirin, would be ineffective and therefore not recommended for RCTs [18]. Based on our literature review, there was no consensus on the efficacy of antiviral agents in patients suffering from COVID-19. This may originate from the small sample size of some studies or differences in the severity of illness in the patient’s population. Meta-analysis results showed that antiviral therapy could significantly alleviate symptoms in patients with COVID-19. However, in terms of negative conversion, ICU entry, mechanical ventilation, and mortality, antiviral therapy had no significant protective effect. The observed relative ineffectiveness may be due to the partially long period of time between the onset of illness to treatment initiation, as the best time for antiviral therapy is at the initial stages of infection [97, 98]. Although, the U.S. Food and Drug Administration (FDA) announced an emergency use authorization (EUA) for remdesivir in severe hospitalized patients with suspected or confirmed COVID-19 [99], although its efficacy is controversial [100]. Remdesivir may be a good drug of choice, considering its promising beneficial effect in preclinical and clinical studies [101], to conduct robust RCTs immediately after the onset of illness.
Convalescent plasma (CP) therapy
Given the lack of active vaccination or specific clinical managements, use of passive antibody therapy (convalescent plasma transfusions) could be of great value against COVID-19 [102]. The attentions on CP have been increased as a valuable therapy due to collecting a large volume per session and frequent donations are possible without any impact on the donor’s hemoglobin [103]. In order to have an effective CP infusion, donor plasma should be tested for antibody and neutralization activity. It seems that CP acts through viral neutralization, cellular cytotoxicity induced by antibody, activation of complement system, and phagocytosis but the exact mechanism of action has remained elusive [102]. Although, almost all included studies on CP (in severe patients) reported its effectiveness in treating the patients, only one study investigated that there was no significant difference in time to clinical improvement compared to control group [55]. As the authors explained, it might be due to the heterogeneity of patients in the duration of the illness or the early termination of the trial [55]. In our study, CP was associated with a considerable beneficial effect in the negative conversion and clinical symptom improvements that was in accordance with the previous reports [56, 104]. Despite the recommendations on the administration of CP in the early stage of illness, it would be effective even initiated in the late phase of viremia [105]. Consequently, plasma therapy as a safe and attractive method with wide clinical benefits would be suggested in this pandemic for moderate to severe patients.
Immunomodulatory agent
Cytokine storm, inflammation, and cell death are well known physiological consequences of respiratory viral infections related to oxidative stress [106]. Immunomodulatory agents (e.g., corticosteroids, interferons (IFN), monoclonal antibodies, and janus kinase inhibitors) would alleviate the cytokine storm through different mechanism of actions, including interfere with binding of inflammatory cytokines to their receptors, inhibition of cytokine signaling pathway, and alteration of inflammatory cytokine gene expression to inhibit their production [107,108,109,110,111]. Vahedi et al., in a retrospective observational study reported that inclusion of short-term and low-dose of prednisolone would provide clinical value in patients with COVID-19 [112]. Based on our literature review, immunomodulatory therapies were associated with significant protective effects against COVID-19. In agreement with previous researches, our meta-analysis results showed that the administration of immunomodulatory agents (especially tocilizumab and anakinra) significantly decreased the mortality rate and ameliorate clinical symptoms in patients with COVID-19 [113, 114]. Besides, co-administration of immunomodulatory agents with antivirals might give physicians more time to provide supportive treatment for patients with COVID-19 [115]. Therefore, we suggest that immunomodulatory agents should be considered in severely ill patients and who needs ICU admission or mechanical ventilation.
Strengths and limitations
To the best of our knowledge, this is the first systematic review and meta-analysis that focus on only the anti-COVID-19 therapies from December 2020. We included available evidences from cohort studies and RCTs in our meta-analysis and excluded case reports, descriptive guidelines, and poor studies with insufficient data.
In the current pandemic situation, trials are still proceeding and there are few reliable studies in the literature in case of COVID-19. Although articles have become more valuable since May, it is not possible to determine an effective drug with certainty and it needs more times to be clarified. Different variables such as the severity of illness, underlying diseases, the hospital length of stay, experienced protocols and guidelines, specialists’ point of view in choosing therapeutic strategy against COVID-19 would affect the patients’ outcome. Moreover, in some studies multi treatments were administered in critically ill patients which provide the complex conditions for comparing the effect of medications. We suggest highly qualified studies such as large double blind RCTs and cohort studies to evaluate the efficacy of current therapeutics, after the pathogenicity of the disease was truly identified. This review could be helpful for the physician in guiding decision-making due to lack of high quality evidences.
Conclusion
In the pandemic situation, there are still ongoing RCTs that could not help physicians to clarify turnouts in the fields of potential managements, yet. The findings in the present study indicated that, all the interventions significantly reduced the mortality and remarkably increased clinical improvements. However, compared with comparators, interventions had no significant effect on negative conversion and mechanical ventilation demand. In subgroup analysis, some classes of medications, including immunomodulators and plasma therapy showed favorable outcomes. Noticeably, due to some reasons such as heterogeneity of treatments, small sample size in some studies, incomplete outcomes of large reliable RCTs we could not propose a potent management against COVID-19. Therefore, preforming large RCTs would be recommended to evaluate the efficacy of medications for COVID-19.
References
Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020;368(6490):489–93.
Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–8.
Shah SGS, Farrow A. A commentary on World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19). Int J Surg (London, England). 2020;76:128–9.
Lum LHW, Tambyah PA. Outbreak of COVID-19–an urgent need for good science to silence our fears? Singap Med J. 2020;61(2):55–7.
WHO. Coronavirus disease (COVID-19) outbreak situation. [cited 2020 May, 19]; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
CDC. COVIDView, A Weekly Surveillance Summary of U.S. COVID-19 Activity. [cited 2020 May, 19]; Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-07-17-2020.pdf.
Ayati N, Saiyarsarai P, Nikfar S. Short and long term impacts of COVID-19 on the pharmaceutical sector. DARU J Pharmaceut Sci. 2020; 1–7.
Tang W, et al.. Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial. MedRxiv. 2020.
Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia. Emerging microbes & infections. 2020;9(1):727–32.
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56:105949.
Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci. 2020;117(17):9490–6.
Cantini F, et al.. Baricitinib therapy in COVID-19: a pilot study on safety and clinical impact. J Infect. 2020.
Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han Q, et al. Transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11(2):216–28.
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–99.
Chen C, et al.. Favipiravir versus arbidol for COVID-19: a randomized clinical trial. MedRxiv 2020.
Cai Q, Yang M, Liu D, Chen J, Shu D, Xia J, Liao X, Gu Y, Cai Q, Yang Y, Shen C, Li X, Peng L, Huang D, Zhang J, Zhang S, Wang F, Liu J, Chen L, Chen S, Wang Z, Zhang Z, Cao R, Zhong W, Liu Y, Liu L. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering. 2020.
Molina JM, et al.. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Med Mal Infect. 2020;10.
Cao Y-c, Deng Q-x, Dai S-x. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence. Travel Med Infect Dis. 2020:101647.
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential rapid diagnostics, vaccine and therapeutics for 2019 novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Koh J, Shah SU, Chua PEY, Gui H, Pang J. Epidemiological and clinical characteristics of cases during the early phase of COVID-19 pandemic: a systematic review and meta-analysis. Frontiers Med. 2020;7:295.
Emami A, et al.. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8 1.
Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chemistry Lab Med (CCLM). 2020;58(7):1021–8.
Espinosa OA, Zanetti AS, Antunes EF, Longhi FG, Matos TA, Battaglini PF. Prevalence of comorbidities in patients and mortality cases affected by SARS-CoV2: a systematic review and meta-analysis. Rev Inst Med Trop Sao Paulo. 2020;62.
Smith V, Seo D, Warty R, Payne O, Salih M, Chin KL, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020;15(6):e0234187.
Zhang L, Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92(5):479–90.
Rabby MII. Current drugs with potential for treatment of COVID-19: a literature review. J Pharm Pharmaceut Sci. 2020;23(1):58–64.
Tobaiqy M, et al.. Therapeutic Management of COVID-19 Patients: A systematic review. Infect Prev Pract. 2020:100061.
Lima WG, et al.. The potential of drug repositioning as a short-term strategy for the control and treatment of COVID-19 (SARS-CoV-2): a systematic review. Arch Virol. 2020:1–9.
AminJafari A, Ghasemi S. The possible of immunotherapy for COVID-19: A systematic review. Int Immunopharmacol. 2020;83:106455.
Patel TK, et al.. Does Adding of Hydroxychloroquine to the Standard Care Provide any Benefit in Reducing the Mortality among COVID-19 Patients?: a Systematic Review. J NeuroImmune Pharmacol. 2020:1.
Zhong H, Wang Y, Zhang ZL, Liu YX, le KJ, Cui M, et al. Efficacy and safety of current therapeutic options for COVID-19 - lessons to be learnt from SARS and MERS epidemic: A systematic review and meta-analysis. Pharmacol Res. 2020;157:104872.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. : John Wiley & Sons; 2011 4.
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):15–25.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.
Goldman JD, Lye DCB, Hui DS, Marks KM, Bruno R, Montejano R, Spinner CD, Galli M, Ahn MY, Nahass RG, Chen YS, SenGupta D, Hyland RH, Osinusi AO, Cao H, Blair C, Wei X, Gaggar A, Brainard DM, Towner WJ, Muñoz J, Mullane KM, Marty FM, Tashima KT, Diaz G, Subramanian A. Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med. 2020.
Higgins JP, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928.
Wells G, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses, vol. 2015. Ottawa: Ottawa Health Research Institute; 2010.
National Heart, L. and B. Institute, Quality assessment tool for case series studies. National Institutes of Health. 2014.
Elgendy IY, Mahmoud AN, Brilakis ES, Bavry AA. Drug-eluting stents versus bare metal stents for saphenous vein graft revascularisation: a meta-analysis of randomised trials. EuroIntervention: J EuroPCR Collab Working Group Intervent Cardiol European Soci Cardiol. 2018;14(2):215–23.
Gao Y-X, Wang YB, Wan YD, Sun TW, Li Y, Hou LL, et al. Immunosuppressive drugs to reduce the mortality rate in patients with moderate to severe paraquat poisoning: a meta-analysis. J Toxicol Sci. 2020;45(3):163–75.
Kuroki T, et al. Legionella prevalence and risk of legionellosis in Japanese households. Epidemiol Infect. 2017;145(7):1398–408.
Higgins. and S. Thompson, Quantifying heterogeneity in a meta-analysis. Stat Med, 2002. 21(11): p. 1539–1558.
Fakhri Y, Atamaleki A, Asadi A., Ghasemi SM, Mousavi Khaneghah A. Toxin Rev. 2019: 1–11, Bioaccumulation of potentially toxic elements (PTEs) in muscleTilapiaspp fish: a systematic review, meta-analysis, and non-carcinogenic risk assessment.
Fakhri Y, Gasser RB, Rostami A, Fan CK, Ghasemi SM, Javanian M, et al. Toxocara eggs in public places worldwide-a systematic review and meta-analysis. Environ Pollut. 2018;242:1467–75.
Foroutan M, Fakhri Y, Riahi SM, Ebrahimpour S, Namroodi S, Taghipour A, et al. The global seroprevalence of toxoplasma gondii in pigs: a systematic review and meta-analysis. Vet Parasitol. 2019;269:42–52.
Rostami A, Riahi SM, Fakhri Y, Saber V, Hanifehpour H, Valizadeh S, et al. The global seroprevalence of toxoplasma gondii among wild boars: a systematic review and meta-analysis. Vet Parasitol. 2017;244:12–20.
Rostami A, et al.. Seroprevalence estimates for toxocariasis in people worldwide: A systematic review and meta-analysis. PLoS Negl Trop Dis, 2019. 13 (12).
Chen Z., et al., Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. MedRxiv, 2020.
Kim, J.-W., et al., Lopinavir-ritonavir versus hydroxychloroquine for viral clearance and clinical improvement in patients with mild to moderate coronavirus disease 2019. Korean J Int Med. 2020.
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Sevestre J, et al. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: A pilot observational study. Travel Med Infect Dis. 2020;34:101663.
Rosenberg ES, et al.. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York state. Jama. 2020.
Million M, Lagier JC, Gautret P, Colson P, Fournier PE, Amrane S, et al. Full-length title: Early treatment of COVID-19 patients with hydroxychloroquine and azithromycin: A retrospective analysis of 1061 cases in Marseille, France. Travel Med Infect Dis. 2020;35:101738.
Hraiech S, et al. Lack of viral clearance by the combination of hydroxychloroquine and azithromycin or lopinavir and ritonavir in SARS-CoV-2-related acute respiratory distress syndrome. Ann Intensive Care. 2020;10(1):1–3.
Kim MS, et al.. Treatment Response to Hydroxychloroquine, Lopinavir/Ritonavir, and Antibiotics for Moderate COVID 19: A First Report Pharmacol Outcomes South Korea. medRxiv. 2020.
Li, L., et al.. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. Jama. 2020.
Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. Jama. 2020;323(16):1582–9.
Ye M, et al. 2020. Treatment with convalescent plasma for COVID‐19 patients in Wuhan, China. J Med Virol.
Salazar E, et al.. Treatment of Coronavirus Disease 2019 (COVID-19) Patients with Convalescent Plasma. Am J Pathol. 2020.
Perotti C., et al.. Mortality reduction in 46 severe Covid-19 patients treated with hyperimmune plasma. A proof of concept single arm multicenter interventional trial. medRxiv. 2020.
Hegerova L, Gooley TA, Sweerus KA, Maree C, Bailey N, Bailey M, et al. Use of convalescent plasma in hospitalized patients with Covid-19-case series. Blood. 2020;136:759–62.
Ye X, Luo YL, Xia SC, Sun QF, Ding JG, Zhou Y, et al. Clinical efficacy of lopinavir/ritonavir in the treatment of coronavirus disease 2019. Eur Rev Med Pharmacol Sci. 2020;24(6):3390–6.
Lian N, Xie H, Lin S, Huang J, Zhao J, Lin Q. Umifenovir treatment is not associated with improved outcomes in patients with coronavirus disease 2019: a retrospective study. Clin Microbiol Infect. 2020;26:917–21.
Deng L, Li C, Zeng Q, Liu X, Li X, Zhang H, et al. Arbidol combined with LPV/r versus LPV/r alone against Corona virus disease 2019: a retrospective cohort study. J Infect. 2020;81:e1–5.
Zhu Z, Lu Z, Xu T, Chen C, Yang G, Zha T, et al. Arbidol monotherapy is superior to lopinavir/ritonavir in treating COVID-19. J Infect. 2020;81:e21–3.
Lan X, et al.. Lopinavir-ritonavir alone or combined with arbidol in the treatment of 73 hospitalized patients with COVID-19: a pilot retrospective study. medRxiv. 2020.
Lou Y, Liu L, Qiu Y. Clinical outcomes and plasma concentrations of Baloxavir Marboxil and Favipiravir in COVID-19 patients: an exploratory randomized. Controlled Trial. medRxiv. 2020.
Li Y, et al.. An exploratory randomized, controlled study on the efficacy and safety of lopinavir/ritonavir or arbidol treating adult patients hospitalized with mild/moderate COVID-19 (ELACOI). MedRxiv. 2020.
Wang Y, Zhang D, du G, du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–78.
Antinori S, Cossu MV, Ridolfo AL, Rech R, Bonazzetti C, Pagani G, et al. Compassionate remdesivir treatment of severe Covid-19 pneumonia in intensive care unit (ICU) and Non-ICU patients: Clinical outcome and differences in post-treatment hospitalisation status. Pharmacol Res. 2020;158:104899.
Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382(24):2327–36.
Xu P, Huang J, Fan Z, Huang W, Qi M, Lin X, et al. Arbidol/IFN-α2b therapy for patients with Corona virus disease 2019: a retrospective multicenter cohort study. Microbes Infect. 2020;22:200–5.
Hung IF-N, Lung KC, Tso EYK, Liu R, Chung TWH, Chu MY, et al. Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395(10238):1695–704.
Zhou Q, et al.. Interferon-a2b treatment for COVID-19. MedRxiv. 2020.
Dastan F, Nadji SA, Saffaei A, Marjani M, Moniri A, Jamaati H, et al. Subcutaneous administration of interferon beta-1a for COVID-19: a non-controlled prospective trial. Int Immunopharmacol. 2020;85:106688.
Zha L, Li S, Pan L, Tefsen B, Li Y, French N, et al. Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19). Med J Aust. 2020;212(9):416–20.
Bian H, et al.. Meplazumab treats COVID-19 pneumonia: an open-labelled, concurrent controlled add-on clinical trial. MedRxiv. 2020.
Cavalli G, et al.. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020.
Cao Y, Wei J, Zou L, Jiang T, Wang G, Chen L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146:137–146.e3.
Alattar R., Ibrahim TBH, Shaar SH, Abdalla S, Shukri K, Daghfal JN, Khatib MY, Aboukamar M, Abukhattab M, Alsoub HA, Almaslamani MA, Omrani AS. Tocilizumab for the treatment of severe coronavirus disease 2019. J Med Virol. 2020.
Capra R, de Rossi N, Mattioli F, Romanelli G, Scarpazza C, Sormani MP, et al. Impact of low dose tocilizumab on mortality rate in patients with COVID-19 related pneumonia. Eur J Internal Med. 2020;76:31–5.
Campochiaro C, Della-Torre E, Cavalli G, de Luca G, Ripa M, Boffini N, et al. Efficacy and safety of tocilizumab in severe COVID-19 patients: a single-Centre retrospective cohort study. Eur J Internal Med. 2020;76:43–9.
Luo P, Liu Y, Qiu L, Liu X, Liu D, Li J. Tocilizumab treatment in COVID-19: a single center experience. J Med Virol. 2020;92(7):814–8.
Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19:102568.
Xu X, Han M, Li T, Sun W, Wang D, Fu B, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci. 2020;117(20):10970–5.
Shojaei A, Salari P. COVID-19 and off label use of drugs: an ethical viewpoint. DARU. 2020.
Erickson T, Chai P, Boyer E. Chloroquine, hydroxychloroquine and COVID-19. Toxicol Commun. 2020;4(1):40–2.
Gbinigie K, Frie K. Should chloroquine and hydroxychloroquine be used to treat COVID-19? A rapid review. BJGP open. 2020.
Sarma P, Kaur H, Kumar H, Mahendru D, Avti P, Bhattacharyya A, et al. Virological and clinical cure in COVID-19 patients treated with hydroxychloroquine: a systematic review and meta-analysis. J Med Virol. 2020;92:776–85.
Decloedt EH, et al.. Benefit v. risk when usingchloroquine in patients with severe COVID-19 disease. SAMJ: S Afr Med J, 2020. 110(5): p. 0–0, 336.
Chorin E, et al.. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat Med. 2020:1–2.
Mehra MR, et al.. RETRACTED: Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020.
Ellison RT, Rio Cd. Lack of Efficacy of Hydroxychloroquine or Azithromycin on COVID-19 Clinical Course. 2020.
Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical updateThe epidemiology of norovirus gastroenteritis in China: disease burden and distribution of genotypes. Frontiers Med. 2020;14:1–10.
Khamitov R, Loginova SIa, Shchukina VN, Borisevich SV, Maksimov VA, Shuster AM. Antiviral activity of arbidol and its derivatives against the pathogen of severe acute respiratory syndrome in the cell cultures. Vopr Virusol. 2008;53(4):9–13.
Coomes EA, Haghbayan H. Favipiravir, an antiviral for COVID-19? J Antimicrob Chemother. 2020;75(7):2013–4.
Yao TT, Qian JD, Zhu WY, Wang Y, Wang GQ. A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus—a possible reference for coronavirus disease-19 treatment option. J Med Virol. 2020;92(6):556–63.
Stengler M. Nature’s Virus Killers. M. Evans. 2001.
Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. 2020;288:128–38.
Administration UFaD. Coronavirus (COVID-19) Update: FDA Issues Emergency Use Authorization for Potential COVID-19 Treatment. 2020.
Ferner RE, Aronson JK. Remdesivir in covid-19. British Med J Publ Group. 2020.
Al-Tawfiq JA, Al-Homoud AH, Memish ZA. Remdesivir as a possible therapeutic option for the COVID-19. Travel Med Infect Dis. 2020;34:101615.
Yiğenoğlu TN, et al.. Convalescent plasma therapy in patients with COVID-19. J Clin Apher.
Rajam G, Sampson J, M. Carlone G, W. Ades E. An augmented passive immune therapy to treat fulminant bacterial infections. Recent Patents Anti-Infect Drug Dis. 2010;5(2):157–67.
Roback JD, Guarner J. Convalescent plasma to treat COVID-19: possibilities and challenges. Jama, Convalescent Plasma to Treat COVID-19. 2020.
Tiberghien P, Lamballerie X, Morel P, Gallian P, Lacombe K, Yazdanpanah Y. Collecting and evaluating convalescent plasma for COVID-19 treatment: why and how?. Vox Sang. 2020.
Delgado-Roche L, Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020;51:384–7.
Lu CC, Chen MY, Lee WS, Chang YL. Potential therapeutic agents against COVID-19: what we know so far. J Chin Med Assoc. 2020;83(6):534–6.
[cited 2020 July 21]; Available from: https://reference.medscape.com/drugs/immunomodulators.
Favalli EG, Biggioggero M, Maioli G, Caporali R. Baricitinib for COVID-19: a suitable treatment? Lancet Infect Dis. 2020.
Sebba A. Tocilizumab: the first interleukin-6-receptor inhibitor. Am J Health Syst Pharm. 2008;65(15):1413–8.
Wiener S, et al. The mechanism of action of a single dose of methylprednisolone on acute inflammation in vivo. J Clin Invest. 1975;56(3):679–89.
Vahedi E., et al.. The clinical value of two combination regimens in the Management of Patients Suffering from Covid-19 pneumonia: a single centered, retrospective, observational study. DARU J Pharm Sci. 2020:1–10.
Zhang J, Xie B, Hashimoto K. Current status of potential therapeutic candidates for the COVID-19 crisis. Brain Behav Immun. 2020;87:59–73.
Dimopoulos G, et al. Favorable Anakinra Responses in Severe Covid-19 Patients with Secondary Hemophagocytic Lymphohistiocytosis. Cell Host Microbe. 2020;28(1):117–123.e1.
Zhao M. Cytokine storm and immunomodulatory therapy in COVID-19: role of chloroquine and anti-IL-6 monoclonal antibodies. Int J Antimicrob Agents. 2020;55(6):105982.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talaie, H., Hosseini, S.M., Nazari, M. et al. Is there any potential management against COVID-19? A systematic review and meta-analysis. DARU J Pharm Sci 28, 765–777 (2020). https://doi.org/10.1007/s40199-020-00367-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40199-020-00367-4