Abstract
Background and Objectives
Opicapone is a novel catechol-O-methyltransferase (COMT) inhibitor. The purpose of this study was to evaluate the tolerability, pharmacokinetics (including the effect of food) and pharmacodynamics (effect on COMT activity) following single oral doses of opicapone in young healthy male volunteers.
Methods
Single rising oral doses of opicapone (10, 25, 50, 100, 200, 400, 800 and 1,200 mg) were administered to eight groups of eight subjects per group (two subjects randomized to placebo and six subjects to opicapone), under a double-blind, randomized, placebo-controlled design. In an additional group of 12 subjects, a 50 mg single dose of opicapone was administered on two occasions, once having fasted overnight and once with a high-fat high-calorie meal.
Results
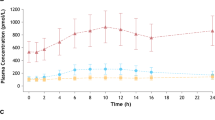
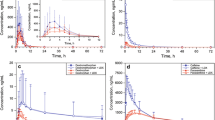
Opicapone was well tolerated at all doses tested. The extent of systemic exposure (area under the plasma concentration–time curve and maximum plasma concentration) to opicapone and metabolites increased in an approximately dose-proportional manner and showed a decrease following concomitant ingestion of a high-fat high-calorie meal. The apparent terminal elimination half-life of opicapone was 0.8–3.2 h. Sulphation appeared to be the main metabolic pathway for opicapone, and both opicapone and the main sulphated metabolite are likely excreted by the biliary route. Maximum COMT inhibition by opicapone was dose dependent, ranged from 36.1 % (10 mg) to 100 % (200 mg and above), and reached statistical significance at all doses tested. The long duration of COMT inhibition by opicapone, however, tended to be independent from the dose taken. The observed half-life of opicapone-induced COMT inhibition in human erythrocytes was 61.6 h (standard deviation [SD] = 37.6 h), which reflects an underlying dissociative process with a kinetic rate constant of 3.1 × 10−6 s−1 (SD = 1.9 × 10−6 s−1). Such a process compares well to the estimated dissociation rate constant (koff) of the COMT–opicapone molecular complex (koff = 1.9 × 10−6 s−1).
Conclusions
Opicapone was well-tolerated and presented dose-proportional kinetics. Opicapone demonstrated marked and sustained inhibition of erythrocyte soluble COMT activity. Based on the observation that the half-life of COMT inhibition is independent of the dose and that it reflects an underlying kinetic process that is consistent with the koff value of the COMT–opicapone complex, we propose that the sustained COMT inhibition, far beyond the observable point of clearance of circulating drug, is due to the long residence time of the reversible complex formed between COMT and opicapone. Globally, these promising results provide a basis for further clinical development of opicapone.





Similar content being viewed by others
References
Morgan JC, Sethi KD. Emerging drugs for Parkinson’s disease. Expert Opin Emerg Drugs. 2006;11(3):403–17.
Schapira AH, Emre M, Jenner P, et al. Levodopa in the treatment of Parkinson’s disease. Eur J Neurol. 2009;16(9):982–9.
Palma PN, Bonifácio MJ, Almeida L, et al. Restoring dopamine levels. In: Simth HJ, Simons C, Sewell RDE, editors. Protein misfolding in neurodegenerative diseases: mechanisms and therapeutic strategies. Boca Raton: CRC Press; 2007. p. 415–45.
Bonifácio MJ, Palma PN, Almeida L, et al. Catechol-O-methyltransferase and its inhibitors in Parkinson’s disease. CNS Drug Rev. 2007;13:352–79.
Nutt JG, Woodward WR, Gancher ST, et al. 3-O-methyldopa and the response to levodopa in Parkinson’s disease. Ann Neurol. 1987;21(6):584–8.
Benetello P, Furlanut M, Zara G, et al. Plasma levels of levodopa and its main metabolites in parkinsonian patients after conventional and controlled-release levodopa-carbidopa associations. Eur Neurol. 1993;33(1):69–73.
Wade LA, Katzman R. 3-O-methyldopa uptake and inhibition of L-dopa at the blood-brain barrier. Life Sci. 1975;17(1):131–6.
Gervas JJ, Muradas V, Bazan E, et al. Effects of 3-OM-dopa on monoamine metabolism in rat brain. Neurology. 1983;33(3):278–82.
Gomes P, Soares-da-Silva P. Interaction between L-DOPA and 3-O-methyl-L-DOPA for transport in immortalised rat capillary cerebral endothelial cells. Neuropharmacology. 1999;38(9):1371–80.
Baas H, Zehrden F, Selzer R, et al. Pharmacokinetic-pharmacodynamic relationship of levodopa with and without tolcapone in patients with Parkinson’s disease. Clin Pharmacokinet. 2001;40(5):383–93.
Muller T, Kolf K, Ander L, et al. Catechol-O-methyltransferase inhibition improves levodopa-associated strength increase in patients with Parkinson disease. Clin Neuropharmacol 2008;31(3):134–40.
Benetello P, Furlanut M, Fortunato M, et al. Levodopa and 3-O-methyldopa in cerebrospinal fluid after levodopa-carbidopa association. Pharmacol Res. 1997;35(4):313–5.
Guttman M, Leger G, Cedarbaum JM, et al. 3-O-methyldopa administration does not alter fluorodopa transport into the brain. Ann Neurol. 1992;31(6):638–43.
Himori N, Mishima K. The COMT inhibitor tolcapone potentiates the anticataleptic effect of Madopar in MPP(+)-lesioned mice. Experientia. 1994;50(10):939–42.
Keranen T, Gordin A, Karlsson M, et al. Inhibition of soluble catechol-O-methyltransferase and single-dose pharmacokinetics after oral and intravenous administration of entacapone. Eur J Clin Pharmacol. 1994;46(2):151–7.
Dingemanse J, Jorga KM, Schmitt M, et al. Integrated pharmacokinetics and pharmacodynamics of the novel catechol-O-methyltransferase inhibitor tolcapone during first administration to humans. Clin Pharmacol Ther. 1995;57(5):508–17.
Baas H, Beiske AG, Ghika J, et al. Catechol-O-methyltransferase inhibition with tolcapone reduces the “wearing off” phenomenon and levodopa requirements in fluctuating parkinsonian patients. Neurology. 1998;50(5 Suppl 5):S46–53.
Kuoppamaki M, Korpela K, Marttila R, et al. Comparison of pharmacokinetic profile of levodopa throughout the day between levodopa/carbidopa/entacapone and levodopa/carbidopa when administered four or five times daily. Eur J Clin Pharmacol. 2009;65(5):443–55.
Brooks DJ. Safety and tolerability of COMT inhibitors. Neurology. 2004;62(1 Suppl 1):S39–46.
Dingemanse J. Issues important for rational COMT inhibition. Neurology. 2000;55 (11 Suppl 4):S24-7; discussion S8-32.
Lang AE, Lees A. Management of Parkinson’s disease: an evidence-based review. Mov Disord. 2002;17(Suppl 4):S45–51.
Nissinen H, Kuoppamaki M, Leinonen M, et al. Early versus delayed initiation of entacapone in levodopa-treated patients with Parkinson’s disease: a long-term, retrospective analysis. Eur J Neurol. 2009;16(12):1305–11.
Ferreira JJ, Rascol O, Poewe W, et al. A double-blind, randomized, placebo and active-controlled study of nebicapone for the treatment of motor fluctuations in Parkinson’s disease. CNS Neurosci Ther. 2010;16:337–47.
Learmonth DA, Kiss LE, Soares-da-Silva P. The chemistry of catechol-O-methyltransferase inhibitors. Int Rev Neurobiol. 2010;95:119–62.
Kiss LE, Ferreira HS, Torrao L, et al. Discovery of a long-acting, peripherally selective inhibitor of catechol-O-methyltransferase. J Med Chem. 2010;53(8):3396–411.
Palma PN, Bonifácio MJ, Loureiro AI, et al. Computation of the binding affinities of catechol-O-methyltransferase inhibitors: multisubstate relative free energy calculations. J Comput Chem. 2012;33(9):970–86.
Bonifácio MJ, Sutcliffe JS, Torrão L, et al. Brain and peripheral levodopa pharmacokinetics in the Cynomolgus monkey following administration of opicapone, a novel catechol-O-methyltransferase inhibitor. Parkinsonism Relat D. 2012;18(S2):S125.
Bonifácio MJ, Torrão L, Loureiro AI, et al. Opicapone: characterization of a novel peripheral long-acting catechol-O-methyltransferase inhibitior. Parkinsonism Relat D 2012;18(S2):S125.
Data on file, Bial, 2012.
FDA/CDER. Guidance for industry: estimating the maximum safe starting dose in initial clinical trials for therapeutics in healthy adult volunteers. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Rockville: FDA/CDER; 2005.
Schultz E, Nissinen E, Kaakkola S. Determination of catechol-O-methyltransferase activity in erythrocytes by high performance liquid chromatography with electrochemical detection. Biomed Chromatogr. 1989;3(2):64–7.
FDA/CDER. Guidance for industry (draft). Food-effect bioavailability and fed bioequivalence studies: study design, data analysis, and labeling. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Rockville: FDA/CDER; 2001.
Silveira P, Vaz-da-Silva M, Almeida L, et al. Pharmacokinetic-pharmacodynamic interaction between BIA 3–202, a novel COMT inhibitor, and levodopa/benserazide. Eur J Clin Pharmacol. 2003;59(8–9):603–9.
Data on file, Bial, 2008.
Ferreira JJ, Almeida L, Cunha L, et al. Effects of nebicapone on levodopa pharmacokinetics, catechol-O-methyltransferase activity, and motor fluctuations in patients with Parkinson disease. Clin Neuropharmacol. 2008;31(1):2–18.
Copeland RA, Pompliano D. Drug–target residence time and its implications for lead optimization. Nat Rev Drug Discov. 2006;1–10.
Tummino PJ, Copeland RA. Residence time of receptor-ligand complexes and its effect on biological function. Biochemistry. 2008;47:5481–92.
Vauquelin G, Van Liefde I. Slow antagonist dissociation and long-lasting in vivo receptor protection. Trends Pharmacol Sci. 2006;27:356–9.
Palma PN, Bonifácio MJ, Loureiro AI, et al. Computation of binding affinity of catechol-O-methyltransferase: opicapone complex. Parkinsonism Relat D 2012;18 (S2):S125.
Vidgren J, Svensson LA, Liljas A. Crystal structure of catechol O-methyltransferase. Nature. 1994;368:354–8.
Rocha JF, Nunes T, Vaz-da-silva M, et al. Pharmacokinetics, pharmacodynamics and tolerability of opicapone, a novel COMT inhibitor, during multiple rising dose regimens in healthy male subjects [abstract]. Parkinsonism Relat D 2012;18 (S2):S126.
Acknowledgments
This study was sponsored by BIAL - Portela & Cª, S.A.
Conflicts of interest
The authors are (Dr Rocha, Dr Palma, Dr Loureiro, Dr Pinto, Dr Bonifácio, Dr Wright, Dr Nunes and Dr Soares-da-Silva) or were (Dr Almeida) employees of Bial – Portela & Cª S.A., the sponsor of the study. A. Falcão received consultancy honoraria from BIAL – Portela & Cª, S.A.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Almeida, L., Rocha, J.F., Falcão, A. et al. Pharmacokinetics, Pharmacodynamics and Tolerability of Opicapone, a Novel Catechol-O-Methyltransferase Inhibitor, in Healthy Subjects. Clin Pharmacokinet 52, 139–151 (2013). https://doi.org/10.1007/s40262-012-0024-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-012-0024-7