Abstract
Introduction
The presence of liver cirrhosis can have a major impact on pharmacodynamics and pharmacokinetics, but guidance for prescribing is lacking.
Objective
The aim of this study is to provide an overview of evidence-based recommendations developed for the safe use of drugs in liver cirrhosis.
Methods
Recommendations were based on a systematic literature search combined with expert opinion from a panel of 10 experts. The safety of each drug was classified as safe, no additional risks known, additional risks known, unsafe, unknown or the safety class was dependent on the severity of liver cirrhosis (Child–Pugh classification). If applicable, drug-specific dosing advice was provided. All recommendations were implemented in clinical decision support systems and on a website.
Results
We formulated 218 recommendations for a total of 209 drugs. For nine drugs, two recommendations were formulated for different administration routes or indications. Drugs were classified as ‘safe’ in 29 recommendations (13.3%), ‘no additional risks known’ in 60 (27.5%), ‘additional risks known’ in 3 (1.4%), and ‘unsafe’ in 30 (13.8%). In 57 (26.1%) of the recommendations, safety depended on the severity of liver cirrhosis and was ‘unknown’ in 39 (17.9%) recommendations. Large alterations in pharmacodynamics were the main reason for classifying a drug as ‘unsafe’. For 67 drugs (31%), a dose adjustment was needed.
Conclusions
Over 200 recommendations were developed for the safe use of drugs in patients with liver cirrhosis. Implementing these recommendations into clinical practice can possibly enhance medication safety in this vulnerable patient group.
Similar content being viewed by others
With a previously developed method, the safety and optimal dosing of more than 200 drugs in patients with liver cirrhosis were evaluated. In this study an overview of the recommendations is given. |
For the majority of the evaluated drugs, changes in pharmacokinetics or pharmacodynamics occurred in patients with liver cirrhosis. Overall, 30% of drugs required dose adjustment and nearly 70 drugs were classified as unsafe in (a stage of) liver cirrhosis. |
Healthcare professionals in The Netherlands are supported during the prescription or dispensing of drugs to patients with liver cirrhosis by alerts from their clinical decision support system and information on a free website. |
1 Introduction
Adverse drug reactions (ADRs) are an important cause of morbidity and mortality worldwide [1, 2]. Patients with hepatic impairment have an increased risk of adverse outcomes with drug use due to the pharmacokinetic and pharmacodynamic changes occurring in liver disease [3, 4]. Most significant are the diminished first-pass effect caused by altered liver blood flow and the decreased activity of drug-metabolizing enzymes. Both result in a higher drug exposure and an increased risk of concentration-dependent ADRs. Furthermore, pathophysiological changes in patients with hepatic impairment increase the risk of specific ADRs, such as renal dysfunction or hepatic encephalopathy [5]. These alterations are considered to be clinically relevant when the liver disease has progressed to liver cirrhosis [3].
Almost 30% of patients with liver cirrhosis experience ADRs; 80% of the ADRs could probably be prevented [6]. Choosing appropriate drugs and doses for these patients is very important, especially because they often use multiple drugs [6, 7]. Practice guidelines can support healthcare professionals in safe prescribing and can reduce the number of inappropriate drug prescriptions, as seen in other patient populations such as older people [8]. For patients with liver cirrhosis, literature regarding pharmacokinetic alterations for several drugs is available [5, 9,10,11,12]; however, we were not aware of a publicly available practice guideline providing recommendations on the safe use of specific drugs in liver cirrhosis [13]. We therefore developed a systematic method to evaluate the safety and dosing of medications to provide recommendations for safe drug use in patients with liver cirrhosis [14]. The aim of this study is to provide an overview of the recommendations for safe drug use for 208 drugs that have been evaluated.
2 Methods
In this study, we used our previously published method to evaluate the safety and dosing of medications to provide recommendations for safe drug use in patients with liver cirrhosis [14]. This method consists of six steps per drug, as described below. Overall, we evaluated 209 drugs, which were chosen because they were (1) often prescribed for complications of liver cirrhosis, or (2) frequently used in the general population.
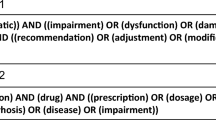
2.1 Step 1: Collection of Evidence
Data regarding the safety and pharmacokinetics of the drug of interest in patients with liver cirrhosis were collected. This evidence was collected in the official Dutch and American product information and in the literature. The literature searches for publications were conducted in PubMed and EMBASE between January and October 2016, and no language restrictions were applied. Studies were included if they related to patients with liver cirrhosis taking the drug of interest and if they reported on outcome data on safety or pharmacokinetics. Citation tracking was used in the Web of Science database to retrieve additional relevant studies.
2.2 Step 2: Data Extraction and Presentation
The following data were extracted from the studies: study design, number and characteristics of included patients and controls (e.g. severity of liver cirrhosis), and information on the intervention. We extracted the following information on outcome(s):
-
Pharmacokinetics: pharmacokinetic parameters (e.g. area under the curve [AUC], maximum plasma concentration [Cmax])
-
Safety: number and type of adverse events and data on discontinuation due to these adverse events
Literature was presented in summary tables and sorted by level of evidence using the classification of the Oxford Centre for Evidence-based Medicine [15]. All evidence was included in an assessment report.
2.3 Step 3: Initial Safety Classification and Dosing Advice
The collected data were used to propose an initial safety classification and dosing advice if applicable. The safety classification (Table 1) was designed to help healthcare professionals efficiently judge the safety of a drug in liver cirrhosis. We added the classification ‘safety class is dependent on severity of cirrhosis’ to the earlier developed classifications (see Table 1) [14]. Pharmacokinetic data were used for the dosing advice. In general, this was advised if the AUC was more than doubled. If the pharmacokinetic alterations were so large that dose reductions were unlikely to allow safe drug use, drugs were classified as ‘unsafe’. The dosing advice could also depend on the severity of liver cirrhosis, expressed as Child–Pugh class (i.e. Child–Pugh A, B or C) [16].
These first three steps were performed by a pharmacist with expertise in drug safety and clinical decision support systems (CDSSs) (RW). Critical steps were verified by a second pharmacist/epidemiologist (SB) and discussed with the expert panel in cases of disagreement.
2.4 Step 4: Consensus of Recommendations by an Expert Panel
An expert panel was composed consisting of 10 members with expertise in the treatment of patients with liver cirrhosis, clinical pharmacology and/or evidence-based medicine. The expert panel evaluated the validity and clinical relevance of the proposed safety classification and dosing advice. The panel concluded by consensus. The final assessment report consisted of the recommendations, supporting evidence and considerations of the expert panel.
2.5 Step 5: Implementation
The recommendations were implemented in all relevant CDSSs in The Netherlands (G-standard and Pharmabase), automatically reaching all pharmacists and numerous general practitioners. If an evaluated medicine was prescribed or dispensed to a patient marked with contraindication ‘liver cirrhosis’, an alert was generated with a short recommendation. Healthcare professionals were referred to a website for more information (http://www.geneesmiddelenbijlevercirrose.nl). This free website also contained a part aimed at patients.
2.6 Step 6: Continuity
To ensure that recommendations remain up-to-date, the expert panel will meet yearly to discuss new literature and comments from healthcare professionals and patients. If necessary, recommendations will be updated.
2.7 Analyses
We determined the total number of recommendations for the 209 drugs evaluated. We also determined the number of drugs per safety class and the number of drugs with dosing advice. It is outside the scope of this paper to show the complete evidence-base we gathered during evaluation of the 209 drugs. To give insight into the type and extent of evidence available, we selected two drugs from every safety class. For these drugs, we described the evidence supporting the classification. This consisted of the number of pharmacokinetic and safety studies and the number of included patients with liver cirrhosis. We also included information on whether the Summary of Product Characteristics (SmPC) contained information on use of the drug in patients with liver cirrhosis.
3 Results
The safety of 209 drugs in patients with liver cirrhosis was evaluated. A total of 218 recommendations were formulated as nine drugs had a different recommendation per route of administration or per indication. Figure 1 represents an overview of the recommendations. Twenty-nine drugs were classified as ‘safe’ (13.3%), 60 as ‘no additional risks known’ (27.5%), 3 as ‘additional risks known’ (1.4%), and 30 as ‘unsafe’ (13.8%). In 57 (26.1%) of the recommendations, safety depended on the severity of liver cirrhosis, and was ‘unknown’ in 39 (17.9%) recommendations. In Table 2, all recommendations are presented. Table 3 shows examples of the evidence supporting the classification of two drugs per safety class. Besides evidence from literature, the last column displays information from the SmPC, which was often lacking or not specifically aimed at patients with liver cirrhosis. The recommendations were successfully implemented in the relevant CDSSs in The Netherlands and on a website.
For 57 drugs, the recommendation depended on the severity of liver cirrhosis, and dosing advice was given for 67 drugs (Fig. 1). The drug simvastatin illustrates the recommendations that were given in such cases. Simvastatin was classified as ‘safe’ for patients with liver cirrhosis Child–Pugh class A or B, under the condition that the patient is started on a low dose (20 mg) and the dose is slowly increased until in the therapeutic range or until ADRs develop. Because of a lack of studies in patients with Child–Pugh class C, the safety of simvastatin was classified as unknown for patients with Child–Pugh class C and no dosing advice was given. All recommendations that depended on the severity of liver cirrhosis, and those with dosing advice, can be found in electronic supplementary Tables 1 and 2, respectively.
We recommended avoiding the use of 30 drugs (classification ‘unsafe’) in all patients with liver cirrhosis. Another 38 drugs were considered unsafe as related to certain Child–Pugh classes (n = 9 Child–Pugh B + C, and n = 29 Child–Pugh C) because of altered pharmacodynamics (n = 41), altered pharmacokinetics (n = 24), or a combination of both (n = 3). Examples of drugs contraindicated because of altered pharmacodynamics were all nonsteroidal anti-inflammatory drugs (NSAIDs). Literature showed that patients with cirrhosis have an increased risk of renal insufficiency with NSAID use compared with healthy controls with more severe consequences. Even so, cirrhotic patients are at risk for gastrointestinal bleeding. Examples of drugs contraindicated due to altered pharmacokinetics were several calcium antagonists (i.e. barnidipine, isradipine). Most calcium antagonists are highly cleared by the liver, resulting in largely increased exposure in patients with cirrhosis compared with healthy controls.
4 Discussion
In this study, we provide an overview of 218 evidence-based recommendations developed to improve safe drug use in patients with liver cirrhosis. Overall, 30% of drugs required dose adjustment and nearly 70 drugs were classified as unsafe in (a stage of) liver cirrhosis. The main reason for unsafe classification were pharmacodynamic changes. The recommendations were implemented in all relevant CDSSs in The Netherlands. In addition, all recommendations are available on a free website (http://www.geneesmiddelenbijlevercirrose.nl).
In this study, we tried to tackle the problem of insufficient information on safe prescribing in patients with liver cirrhosis. A number of comparable studies are available [5, 9,10,11,12]. Most focus on altered pharmacokinetics, while we show that pharmacodynamic changes are also relevant in the decision process. This study is therefore unique in using both pharmacokinetic and pharmacodynamic (safety) literature to develop recommendations.
An important source of prescribing information is the product information (SmPC). We noted a lack of information on liver cirrhosis in the product information, which was also recognized in a study from 2001 that classified the SmPC information on liver disease as “often inconsistent, unclear and unhelpful” [17]. Since 2003 and 2005, the FDA and EMA, respectively, published guidelines for pharmacokinetic research in patients with hepatic impairment and how to present this data in the product information [18, 19]. For further research it would be interesting to study the quality of the information in these new SmPCs. In addition, many agents were licensed before 2003–2005 and these product labels require updating based on these new guidelines [18, 19].
We developed and published the safety classification we used to support healthcare professionals to efficiently judge the safety of a drug in liver cirrhosis [14]. In our original safety classification, there was also an option for classifying drugs cleared for < 20% by the liver as ‘no additional risks known’, although no data were available. Based on the important influence of pharmacodynamics, the expert panel specified this to locally-acting drugs with no systemic uptake (bioavailability [F] < 1%, not based on an extensive first-pass effect). The classification of drugs was not always easy as the following two examples show. Codeine is a prodrug that requires liver metabolism for conversion to the active drug and it can be expected that efficacy will decrease with the increasing severity of liver cirrhosis. Azathioprine was associated with increased adverse events in patients with liver cirrhosis, but is also one of the only effective treatments for autoimmune hepatitis. Our recommendation therefore includes explanations in which we try to deal with such issues by comprehensively discussing the details of the classification of a drug.
The recommendations were implemented on a website and in all relevant CDSSs in The Netherlands. The implementation revealed issues that need attention. First, patients with liver cirrhosis need to be correctly marked in the CDSSs. In The Netherlands, the contraindication ‘hepatic impairment’ was always used for this purpose; however, we noted that most of the patients marked with this contraindication did not have liver cirrhosis, causing an incorrect signal in the CDSSs. Another difficulty is that in a substantial part of the recommendations, the severity of liver cirrhosis needs to be known (i.e. Child–Pugh class). Before these recommendations can be used, gastroenterologists need to determine the Child–Pugh class of their patients and communicate this to the general practitioner and pharmacist. These difficulties are also recognized in literature about implementing contraindications into a CDSS [20] and are important to consider when setting up medication monitoring via a CDSS for these patients.
This study has its limitations. Although we evaluated 209 drugs, this is only a proportion of all drugs available. The choice for these drugs was based on an estimation of the most frequently used drugs in patients with liver cirrhosis and is in good agreement with the literature [21, 22]. We aim to eventually evaluate all drugs. Another limitation is the amount of literature available. As stated in Table 3, for some drugs there were several studies performed in patients with liver cirrhosis, while for others, there were only a few or no studies. Because of the limited literature, 39 drugs were classified as ‘unknown’, including frequently used drugs such as nitrofurantoin. As the recommendations are evidence-based, more research will improve the quality of the recommendations and can better support healthcare professionals. For now, the literature review per drug identifies knowledge gaps and is a good starting point for further research. A third limitation is that the complete recommendations with detailed explanations are currently only available in the Dutch language. Nevertheless, in this study, we provided an overview in English and plan to translate the recommendations in the future.
5 Conclusions
In this study, we provided evidence-based recommendations to aid in prescribing for patients with liver cirrhosis. This is the first study that applies a practical approach providing recommendations that have been implemented in all relevant CDSSs in The Netherlands and on a website. Our advice aids healthcare professionals in tailoring pharmacotherapy for the individual patient with liver cirrhosis, which can possibly prevent ADRs and subsequent morbidity and mortality in vulnerable cirrhotic patients.
References
Thomsen LA, Winterstein AG, Søndergaard B, Haugbølle LS, Melander A. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother. 2007;41(9):1411–26.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients. BMJ. 2004;329(7456):15–9.
Verbeeck RK. Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol. 2008;64(12):1147–61.
Delco F, Tchambaz L, Schlienger R, Drewe J, Krahenbuhl S. Dose adjustment in patients with liver disease. Drug Saf. 2005;28(6):529–45.
Westphal J, Brogard J. Drug administration in chronic liver disease. Drug Saf. 1997;17(1):47–73.
Franz CC, Hildbrand C, Born C, Egger S, Bravo AER, Krähenbühl S. Dose adjustment in patients with liver cirrhosis: impact on adverse drug reactions and hospitalizations. Eur J Clin Pharmacol. 2013;69(8):1565–73.
Lucena IM, Andrade RJ, Tognoni G, Hidalgo R, de la Cuesta F. Multicenter hospital study on prescribing patterns for prophylaxis and treatment of complications of cirrhosis. Eur J Clin Pharmacol. 2002;58(6):435–40.
Zhang YJ, Liu WW, Wang JB, Guo JJ. Potentially inappropriate medication use among older adults in the USA in 2007. Age Ageing. 2011;40(3):398–401.
Schlatter C, Egger SS, Tchambaz L, Krähenbühl S. Pharmacokinetic changes of psychotropic drugs in patients with liver disease. Drug Saf. 2009;32(7):561–78.
Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis - a practical guide. Aliment Pharmacol Ther. 2013;37(12):1132–56.
Steelandt J, Jean-Bart E, Goutelle S, Tod M. A Prediction Model of Drug Exposure in Cirrhotic Patients According to Child-Pugh Classification. Clin Pharmacokinet. 2015;54(12):1245–58.
Rodighiero V. Effects of liver disease on pharmacokinetics. Clin Pharmacokinet. 1999;37(5):399–431.
Hilscher M, Odell L, Myhre L, Prokop L, Talwalkar J. The pharmacotherapy of cirrhosis: concerns and proposed investigations and solutions. J Clin Pharm Ther. 2016;41(6):587–91.
Weersink RA, Bouma M, Burger DM, Drenth JP, Hunfeld NG, Kranenborg M, et al. Evaluating the safety and dosing of drugs in patients with liver cirrhosis by literature review and expert opinion. BMJ Open. 2016;6(10):e012991.
OCEBM Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine. Available at: http://www.cebm.net/index.aspx?0=5653. Accessed 2 Mar 2017.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–9.
Failings in treatment advice. SPCs and black triangles. Drug Ther Bull. 2001;39(4):25–7.
Food and Drug Administration. Guidance for Industry. Pharmacokinetics in Patients with Impaired Hepatic Function: Study Design, Data Analysis, and Impact on Dosing and Labeling. 2008. Available at: https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072123.pdf. Accessed 17 Jan 2017.
European Medicines Agency. Guideline on the evaluation of the pharmacokinetics of medicinal products in patients with impaired hepatic function. 2005. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003122.pdf. Accessed 17 Jan 2017.
Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007;14(1):29–40.
Lucena MI, Andrade RJ, Tognoni G, Hidalgo R, de La Cuesta FS. Drug use for non-hepatic associated conditions in patients with liver cirrhosis. Eur J Clin Pharmacol. 2003;59(1):71–6.
Franz CC, Egger S, Born C, Ratz Bravo AE, Krahenbuhl S. Potential drug-drug interactions and adverse drug reactions in patients with liver cirrhosis. Eur J Clin Pharmacol. 2012;68(2):179–88.
Acknowledgements
The authors would like to thank Minke Kranenborg, Ton Lisman, Eline Okel, Sandra van Putten and Elise Smolders for their contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by ZonMw GGG-STIP Grant number 836044009. ZonMw is the Dutch national organisation for health research and healthcare innovation.
Conflict of interest
Rianne A. Weersink, Margriet Bouma, David M. Burger, Joost P.H. Drenth, S. Froukje Harkes-Idzinga, Nicole G.M. Hunfeld, Herold J. Metselaar, Margje H. Monster-Simons, Katja Taxis and Sander D. Borgsteede have no conflicts of interest directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Weersink, R.A., Bouma, M., Burger, D.M. et al. Evidence-Based Recommendations to Improve the Safe Use of Drugs in Patients with Liver Cirrhosis. Drug Saf 41, 603–613 (2018). https://doi.org/10.1007/s40264-017-0635-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-017-0635-x