Abstract
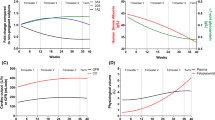
Since the inception of clinical teratology, the vast majority of scientific work has focused on identification of drugs and environmental agents causing malformations in humans as a dichotomous variable (i.e. yes or no), as well as the relative and absolute risks of such occurrences. Generally, the dose dependency of such events has not been investigated. With the establishment of large pregnancy databases, dose-dependence relationships are being uncovered for increasing numbers of medications, including valproic acid, carbamazepine, phenobarbital, lamotrigine, topiramate, and lithium. In this review we discuss newly recognized dose-dependent human teratogens and the implications to counseling and clinical management of pregnant women. The option of limiting the dose below a teratogenic threshold for women who may need these drugs may be important in managing such pregnancies. Similarly, in women that were exposed before they realized they had conceived, this new knowledge may lead to significant improvement in risk assessment. A common denominator of all studies calculating dose-dependent teratogenicity in humans is their use of total daily drug dose. None of these studies have standardized their calculations for women’s body weight. It is quite possible that the teratogenic dose threshold may be below the clinically effective dose levels for specific women, and hence such information needs to be considered and applied individually. With large administrative databases now reporting on drug safety in pregnancy, more accurate data will likely emerge on dose dependency of human teratogens, and these will likely increase the accuracy of risk assessment.
Similar content being viewed by others
References
Cohen LS, Friedman JM, Jefferson JW, et al. A reevaluation of risk of in utero exposure to lithium. JAMA. 1994;271:146–50.
Yacobi S, Ornoy A. Is lithium a real teratogen? What can we conclude from the prospective versus retrospective studies? A review. Isr J Psych Rel Dis. 2008;45:95–106.
Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376:2245–54.
Smithberg M, Dixit PK. Teratogenic effects of lithium in mice. Teratology. 1982;26:239–46.
Tomson T, Battino D, Bonizzoni E, et al. EURAP study group. Dose-dependent risk of malformations with antiepileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol. 2011;10:609–17.
Tomson T, Battino D, Bonizzoni E, et al. Dose-dependent teratogenicity of valproate in mono- and polytherapy: an observational study. Neurology. 2015;85(10):866–72.
Vajda FJ, Hitchcock A, Graham J, et al. Foetal malformations and seizure control: 52 months data of the Australian Pregnancy Registry. Eur J Neurol. 2006;13:645–54.
Mawer G, Clayton-Smith J, Coyle H, et al. Outcome of pregnancy in women attending an outpatient epilepsy clinic: adverse features associated with higher doses of sodium valproate. Seizures. 2002;11:512–6.
Weston J, Bromley R, Jackson CF, et al. Monotherapy treatment of epilepsy in pregnancy: congenital malformation outcomes in the child. Cochrane Database Syst Rev. 2016;11:CD010224.
Diav-Citrin O, Shechtman S, Bar-Oz B, et al. Pregnancy outcome after in utero exposure to valproate: evidence of dose relationship in teratogenic effect. CNS Drugs. 2008;22:325–34.
Thomas SV, Jose M, Divakaran S, et al. Malformation risk of antiepileptic drug exposure during pregnancy in women with epilepsy: results from a pregnancy registry in South India. Epilepsia. 2017;58:274–81.
Bromley RL, Mawer GE, Briggs M, et al. The prevalence of neurodevelopmental disorders in children prenatally exposed to antiepileptic drugs. J Neurol Neurosurg Psychiatry. 2013;84:637–43.
Vajda FJ, O’Brien TJ, Lander CM, et al. The teratogenicity of the newer antiepileptic drugs—an update. Acta Neurol Scand. 2014;130:234–8.
Hernandez-Diaz S, Huybrechts KF, Desai RJ, et al. Topiramate use early in pregnancy and the risk of oral clefts: a pregnancy cohort study. Neurology. 2018;90(4):e342–51.
Morrow J, Russell A, Guthrie E, et al. Malformation risk of antiepileptic drugs in pregnancy: a prospective study from the UK epilepsy and pregnancy register. J Neurol Neurosurg Psychiatr. 2006;77:193–8.
Menegola E, Broccia ML, Nau H, et al. Teratogenic effects of sodium valproate in mice and rats at midgestation and at term. Teratog Carcinog Mutagen. 1996;16:97–108.
Elshama SS, Osman HE, El-Kenawy A-M. Teratogenic effect of carbamazepine use during pregnancy in the mice. Pak J Pharm Sci. 2015;28:201–12.
Kim SH, Lee IC, Baek HS, et al. Dose-response effects of diphenylhydantoin on pregnant dams and embryo-fetal development in rats. Birth Defects Res B. 2012;95:337–45.
Manent JB, Jorquera I, Franco V, et al. Antiepileptic drugs and brain maturation: fetal exposure to lamotrigine generates cortical malformations in rats. Epilepsy Res. 2008;78:131–9.
Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009;200:4–24.
Brent RL. Counseling patients exposed to ionizing radiation during pregnancy. Rev Panam Salud Publica. 2006;20:198–204.
Brent RL. Protection of the gametes, embryo/fetus from prenatal radiation exposure. Health Phys. 2015;108:242–74.
Reinou S, Groen S, Jin Y, et al. Fear of the unknown: ionizing radiation exposure during pregnancy. Am J Obst Gynecol. 2012;203:456–62.
Kaplan YC, Nulman I, Koren G. Dose-dependent risk of malformations with antiepileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Ther Drug Monit. 2015;37:557–8.
Vajda FJ, O’Brien TJ, Graham JE, et al. Dose dependence of fetal malformations associated with valproate. Neurology. 2013;81:999–1003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
GK, AO and MB declare no conflict of interests associated with this research. No funding was received for the conduct or publication of the research presented in this paper.
Rights and permissions
About this article
Cite this article
Koren, G., Berkovitch, M. & Ornoy, A. Dose-Dependent Teratology in Humans: Clinical Implications for Prevention. Pediatr Drugs 20, 331–335 (2018). https://doi.org/10.1007/s40272-018-0294-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-018-0294-0