Abstract
Background
Exposure to acute prolonged sitting can result in vascular dysfunction, particularly within the legs. This vascular dysfunction, assessed using flow-mediated dilation (FMD), is likely the consequence of decreased blood flow-induced shear stress. With mixed success, several sitting interruption strategies have been trialled to preserve vascular function.
Objectives
The objectives of this meta-analysis were to (1) assess the effects of acute prolonged sitting exposure on vascular function in the upper- and lower-limb arteries, and (2) evaluate the effectiveness of sitting interruption strategies in preserving vascular function. Sub-group analyses were conducted to determine whether artery location or interruption modality explain heterogeneity.
Data Sources
Electronic databases (PubMed, Web of Science, SPORTDiscus, and Google Scholar) were searched from inception to January 2020. Reference lists of eligible studies and relevant reviews were also checked.
Study Selection
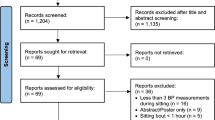
Inclusion criteria for objective (1) were: (i) FMD% was assessed pre- and post-sitting; (ii) studies were either randomised-controlled, randomised-crossover, or quasi-experimental trials; (iii) the sitting period was ≥ 1 h; and (iv) participants were healthy non-smoking adults (≥ 18 years), and free of vascular-acting medication and disease at the time of testing. Additional inclusion criteria for objective (2) were: (i) the interruption strategy must have been during the sitting period; (ii) there was a control (uninterrupted sitting) group/arm; and (iii) the interruption strategy must have involved the participants actively moving their lower- or upper-limbs.
Appraisal and Synthesis Methods
One thousand eight hundred and two articles were identified, of which 17 (22 trials, n = 269) met inclusion criteria for objective (1). Of those 17 articles, 6 studies (9 trials, n = 127) met the inclusion criteria for objective (2). Weighted mean differences (WMD), 95% confidence intervals (95% CI), and standardised mean difference (SMD) were calculated for all trials using random-effects meta-analysis modelling. SMD was used to determine the magnitude of effect, where < 0.2, 0.2, 0.5, and 0.8 was defined as trivial, small, moderate, and large respectively.
Results
(1) Random-effects modelling showed uninterrupted bouts of prolonged sitting resulted in a significant decrease in FMD% (WMD = − 2.12%, 95% CI − 2.66 to − 1.59, SMD = 0.84). Subgroup analysis revealed reductions in lower- but not upper-limb FMD%. (2) Random-effects modelling showed that interrupting bouts of sitting resulted in a significantly higher FMD% compared to uninterrupted sitting (WMD = 1.91%, 95% CI 0.40 to 3.42, SMD = 0.57). Subgroup analyses failed to identify an optimum interruption strategy but revealed moderate non-significant effects for aerobic interventions (WMD = 2.17%, 95% CI − 0.34 to 4.67, SMD = 0.69) and simple resistance activities (WMD = 2.40%, 95% CI − 0.08 to 4.88, SMD = 0.55) and a trivial effect for standing interruptions (WMD = 0.24%, 95% CI − 0.90 to 1.38, SMD = 0.16).
Conclusions
Exposure to acute prolonged sitting leads to significant vascular dysfunction in arteries of the lower, but not upper, limbs. The limited available data indicate that vascular dysfunction can be prevented by regularly interrupting sitting, particularly with aerobic or simple resistance activities.




Similar content being viewed by others
Data Availability
The data analysed for this meta-analysis are available from the corresponding author on reasonable request.
References
Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–28.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–32.
Ballard KD, Duguid RM, Berry CW, Dey P, Bruno RS, Ward RM, et al. Effects of prior aerobic exercise on sitting-induced vascular dysfunction in healthy men. Eur J Appl Physiol. 2017;117:2509–18.
Carter SE, Draijer R, Holder SM, Brown L, Thijssen DH, Hopkins ND. Effect of different walking break strategies on superficial femoral artery endothelial function. Physiol Rep. 2019;7:e14190.
Carter SE, Gladwell VF. Effect of breaking up sedentary time with callisthenics on endothelial function. J Sports Sci. 2017;35:1508–14.
Climie RE, Wheeler MJ, Grace M, Lambert E, Cohen N, Owen N, et al. Simple intermittent resistance activity mitigates the detrimental effect of prolonged unbroken sitting on arterial function in overweight and obese adults. J Appl Physiol. 2018;125:1787–94.
Credeur DP, Miller SM, Jones R, Lee S, Dolbow DR, Fryer SM, et al. Impact of prolonged sitting on peripheral and central vascular health. Am J Cardiol. 2018;123:260–6.
Kruse NT, Hughes WE, Benzo RM, Carr LJ, Casey DP. Workplace strategies to prevent sitting-induced endothelial dysfunction. Med Sci Sports Exerc. 2018;50:801–8.
Morishima T, Restaino RM, Walsh LK, Kanaley JA, Fadel PJ, Padilla J. Prolonged sitting-induced leg endothelial dysfunction is prevented by fidgeting. Am J Physiol-Heart Circ Physiol. 2016;311:H177–H182182.
Morishima T, Restaino RM, Walsh LK, Kanaley JA, Padilla J. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci. 2017;131:1045–53.
Morishima T, Tsuchiya Y, Padilla J, Ochi E. Eight weeks of fish oil supplementation does not prevent sitting-induced leg endothelial dysfunction. Appl Physiol Nutr Metab. 2019;45:55–60.
O’Brien MW, Johns JA, Williams TD, Kimmerly DS. Sex does not influence impairments in popliteal endothelial-dependent vasodilator or vasoconstrictor responses following prolonged sitting. J Appl Physiol. 2019;127:679–87.
Padilla J, Sheldon RD, Sitar DM, Newcomer SC. Impact of acute exposure to increased hydrostatic pressure and reduced shear rate on conduit artery endothelial function: a limb-specific response. Am J Physiol-Heart Circ Physiol. 2009;297:H1103–H1108108.
Restaino RM, Holwerda SW, Credeur DP, Fadel PJ, Padilla J. Impact of prolonged sitting on lower and upper limb micro-and macrovascular dilator function. Exp Physiol. 2015;100:829–38.
Restaino RM, Walsh LK, Morishima T, Vranish JR, Martinez-Lemus LA, Fadel PJ, et al. Endothelial dysfunction following prolonged sitting is mediated by a reduction in shear stress. Am J Physiol Heart Circ Physiol. 2016;310:H648–H653653.
Thosar SS, Bielko SL, Mather KJ, Johnston JD, Wallace JP. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc. 2015;47:843–9.
Thosar SS, Bielko SL, Wiggins CC, Wallace JP. Differences in brachial and femoral artery responses to prolonged sitting. Cardiovasc Ultrasound. 2014;12:50.
Thosar SS, Bielko SL, Wiggins CS, Klaunig JE, Mather KJ, Wallace JP. Antioxidant vitamin C prevents decline in endothelial function during sitting. Med Sci Monit Int Med J Exp Clin Res. 2015;21:1015–21.
Vranish JR, Young BE, Kaur J, Patik JC, Padilla J, Fadel PJ. Influence of sex on microvascular and macrovascular responses to prolonged sitting. Am J Physiol Heart Circ Physiol. 2017;312:H800–H805805.
Lima BB, Hammadah M, Kim JH, Uphoff I, Shah A, Levantsevych O, et al. Association of transient endothelial dysfunction induced by mental stress with major adverse cardiovascular events in men and women with coronary artery disease. JAMA Cardiol. 2019;4:988–96.
Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010;26:631–40.
Ras RT, Streppel MT, Draijer R, Zock PL. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol. 2013;168:344–51.
Xu Y, Arora RC, Hiebert BM, Lerner B, Szwajcer A, McDonald K, et al. Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2014;15:736–46.
Matsuzawa Y, Kwon T, Lennon RJ, Lerman LO, Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4:e002270.
Padilla J, Fadel PJ. Prolonged sitting leg vasculopathy: contributing factors and clinical implications. Am J Physiol Heart Circ Physiol. 2017;313:H722–H728728.
Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, et al. The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35.
Clemes SA, Houdmont J, Munir F, Wilson K, Kerr R, Addley K. Descriptive epidemiology of domain-specific sitting in working adults: the Stormont Study. J Public Health. 2015;38:53–60.
Clemes SA, O’connell SE, Edwardson CL. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J Occup Environ Med. 2014;56:298–303.
Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31:369–71.
Jans MP, Proper KI, Hildebrandt VH. Sedentary behavior in Dutch workers: differences between occupations and business sectors. Am J Prev Med. 2007;33:450–4.
Mabry R, Koohsari MJ, Bull F, Owen N. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health. 2016;16:1003.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81.
Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act. 2012;9:128.
Win AM, Yen LW, Tan KH, Lim RBT, Chia KS, Mueller-Riemenschneider F. Patterns of physical activity and sedentary behavior in a representative sample of a multi-ethnic South-East Asian population: a cross-sectional study. BMC Public Health. 2015;15:318.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6:e1000097.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2008.
Heyland DK, MacDonald S, Keefe L, Drover JW. Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998;280:2013–9.
Heyland DK, Novak F, Drover JW, Jain M, Su X, Suchner U. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA. 2001;286:944–53.
Stoner L, Sabatier MJ. Use of ultrasound for non-invasive assessment of flow-mediated dilation. J Atheroscler Thromb. 2012;19:407–21.
Thijssen DH, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol-Heart Circ Physiol. 2011;300:H2–12.
Thijssen DH, Bruno RM, van Mil AC, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40:2534–47.
Bots ML, Westerink J, Rabelink TJ, de Koning EJ. Assessment of flow-mediated vasodilatation (FMD) of the brachial artery: effects of technical aspects of the FMD measurement on the FMD response. Eur Heart J. 2004;26:363–8.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Furuya-Kanamori L, Barendregt JJ, Doi SA. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16:195–203.
Stoner L, Tarrant MA, Fryer S, Faulkner J. How should flow-mediated dilation be normalized to its stimulus? Clin Physiol Funct Imaging. 2013;33:75–8.
Stoner L, Faulkner J, Sabatier MJ. Is allometric scaling really a panacea for flow-mediated dilation? Commentary on paper by Atkinson and Batterham. Atherosclerosis. 2013;228:280–1.
McLay KM, Nederveen JP, Koval JJ, Paterson DH, Murias JM. Allometric scaling of flow-mediated dilation: is it always helpful? Clin Physiol Funct Imaging. 2018;38:663–9.
Harris RA, Padilla J. Proper, “normalization” of flow-mediated dilation for shear. J Appl Physiol. 2007;103:1108–1108.
Atkinson G, Batterham AM. The percentage flow-mediated dilation index: a large-sample investigation of its appropriateness, potential for bias and causal nexus in vascular medicine. Vasc Med. 2013;18:354–65.
Atkinson G. Shear rate normalization is not essential for removing the dependency of flow-mediated dilation on baseline artery diameter: past research revisited. Physiol Meas. 2014;35:1825–35.
Williams MRI, Westerman RA, Kingwell BA, Paige J, Blombery PA, Sudhir K, et al. Variations in endothelial function and arterial compliance during the menstrual cycle. J Clin Endocrinol Metab. 2001;86:5389–95.
Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW. Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med. 2010;235:111–8.
Harris RA, Tedjasaputra V, Zhao J, Richardson RS. Premenopausal women exhibit an inherent protection of endothelial function following a high-fat meal. Reprod Sci. 2012;19:221–8.
Masayoshi H, Masahiro A, Masato E, Michiro I, Koichi K, Kenji T, et al. Modulation of endothelium-dependent flow-mediated dilatation of the brachial artery by sex and menstrual cycle. Circulation. 1995;92:3431–5.
Shenouda N, Priest SE, Rizzuto VI, MacDonald MJ. Brachial artery endothelial function is stable across a menstrual and oral contraceptive pill cycle but lower in premenopausal women than in age-matched men. Am J Physiol Heart Circ Physiol. 2018;315:H366–H374374.
Pyke KE, Tschakovsky ME. The relationship between shear stress and flow-mediated dilatation: implications for the assessment of endothelial function. J Physiol. 2005;568:357–69.
Cheng C, de Crom R, van Haperen R, Helderman F, Gourabi BM, van Damme LC, et al. The role of shear stress in atherosclerosis. Cell Biochem Biophys. 2004;41:279–94.
Cheng C, Tempel D, Van Haperen R, Van Der Baan A, Grosveld F, Daemen M, et al. Atherosclerotic lesion size and vulnerability are determined by patterns of fluid shear stress. Circulation. 2006;113:2744–53.
Cheng JL, Au JS, MacDonald MJ. Peripheral artery endothelial function responses to altered shear stress patterns in humans. Exp Physiol. 2019;104:1126–35.
Green DJ, Hopman MT, Padilla J, Laughlin MH, Thijssen DH. Vascular adaptation to exercise in humans: role of hemodynamic stimuli. Physiol Rev. 2017;97:495–528.
Ridger V, Krams R, Carpi A, Evans PC. Hemodynamic parameters regulating vascular inflammation and atherosclerosis: a brief update. Biomed Pharmacother. 2008;62:536–40.
Thijssen DH, Dawson EA, Tinken TM, Cable NT, Green DJ. Retrograde flow and shear rate acutely impair endothelial function in humans. Hypertension. 2009;53:986–92.
Kitano A, Shoemaker JK, Ichinose M, Wada H, Nishiyasu T. Comparison of cardiovascular responses between lower body negative pressure and head-up tilt. J Appl Physiol. 2005;98:2081–6.
Walsh LK, Restaino RM, Martinez-Lemus LA, Padilla J. Prolonged leg bending impairs endothelial function in the popliteal artery. Physiol Rep. 2017;5:e13478.
Thijssen DH, Dawson EA, Black MA, Hopman MT, Cable NT, Green DJ. Heterogeneity in conduit artery function in humans: impact of arterial size. Am J Physiol Heart Circ Physiol. 2008;295:H1927–H19341934.
Carter SE, Draijer R, Holder SM, Brown L, Thijssen DH, Hopkins ND. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J Appl Physiol. 2018;125:790–8.
McManus AM, Ainslie PN, Green DJ, Simair RG, Smith K, Lewis N. Impact of prolonged sitting on vascular function in young girls. Exp Physiol. 2015;100:1379–87.
Barone Gibbs B, Kowalsky RJ, Perdomo SJ, Taormina JM, Balzer JR, Jakicic JM. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J Hypertens. 2017;35:2411–8.
Vranish JR, Young BE, Stephens BY, Kaur J, Padilla J, Fadel PJ. Brief periods of inactivity reduce leg microvascular, but not macrovascular, function in healthy young men. Exp Physiol. 2018;103:1425–34.
Author information
Authors and Affiliations
Contributions
CP and GZ completed the literature search. CP, SF, and LS completed quality assessment. CP and GZ extracted all relevant data from selected articles. CP and LS conducted data analysis. CP, SF, KS, and LS wrote the first draft of the manuscript. GZ, BBG, JP, and JP revised the original manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of Interest
Craig Paterson, Simon Fryer, Gabriel Zieff, Keeron Stone, Daniel Credeur, Bethany Barone Gibbs, Jaume Padilla, John Parker, and Lee Stoner declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paterson, C., Fryer, S., Zieff, G. et al. The Effects of Acute Exposure to Prolonged Sitting, With and Without Interruption, on Vascular Function Among Adults: A Meta-analysis. Sports Med 50, 1929–1942 (2020). https://doi.org/10.1007/s40279-020-01325-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-020-01325-5