Abstract
Purpose of Review
Although e-cigarettes have become popular, especially among youth, the health effects associated with e-cigarette use remain unclear. This review discusses current evidence relating to the cardiovascular, pulmonary, and immunological effects of e-cigarettes.
Recent Findings
The use of e-cigarettes by healthy adults has been shown to increase blood pressure, heart rate, and arterial stiffness, as well as resistance to air flow in lungs. Inhalation of e-cigarette aerosol has been shown to elicit immune responses and increase the production of immunomodulatory cytokines in young tobacco-naïve individuals. In animal models, long-term exposure to e-cigarettes leads to marked changes in lung architecture, dysregulation of immune genes, and low-grade inflammation. Exposure to e-cigarette aerosols in mice has been shown to induce DNA damage, inhibit DNA repair, and promote carcinogenesis. Chronic exposure to e-cigarettes has also been reported to result in the accumulation of lipid-laden macrophages in the lung and dysregulation of lipid metabolism and transport in mice. Although, the genotoxic and inflammatory effects of e-cigarettes are milder than those of combustible cigarettes, some of the cardiorespiratory effects of the two insults are comparable. The toxicity of e-cigarettes has been variably linked to nicotine, as well as other e-cigarette constituents, operating conditions, and use patterns.
Summary
The use of e-cigarettes in humans is associated with significant adverse cardiorespiratory and immunological changes. Data from animal models and in vitro studies support the notion that long-term use of e-cigarettes may pose significant health risks.
Similar content being viewed by others
Introduction
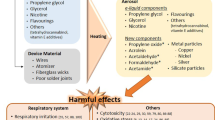
E-cigarettes are electronic nicotine delivery systems (ENDS) that aerosolize a solution of nicotine dissolved in a mixture of propylene glycol and vegetable glycerin. They were designed to deliver nicotine without concurrent exposure to many of the toxic side products generated by the burning of tobacco [1]. Since their introduction in the USA in 2007, e-cigarettes have become increasingly popular [2]. In 2016, the overall use of e-cigarettes in the US adults was 4.5%, which remained stable in 2017, but increased to 5.4% in 2018 [3]. This translates to 11.2 million adults using e-cigarettes in 2016, and 13.7 million adults in 2018 [3]. In 2020, 4.4% adults in the USA reported current e-cigarette use, as estimated by the National Health Interview Survey [4]. E-cigarette use has also become increasing popular among youth and young adults. Analysis of the National Youth Tobacco Survey 2020 shows that 19.6% of high school student (3.02 million) and 4.7% of middle school (550,000) students reported current e-cigarette use [5]. This use of e-cigarettes was much higher than in 2018, when 11.6% of high school students reported current use of only e-cigarettes [6]. Taken together, these data support the growing concern that the use of e-cigarettes, particularly among youth and young adults, is a major public health concern.
Because e-cigarettes do not burn tobacco, and because they generate lower levels of combustion products than conventional cigarettes [7], some believe that e-cigarettes are a safer alternative to combustible cigarettes, and that they could aid smoking cessation among those who will not, or cannot quit smoking [8]. The full inventory of the chemicals generated by combustible cigarettes exceeds several thousand. Some of these chemicals are highly poisonous and toxic, and many incite or promote cancinogenesis, cardiovascular injury, and pulmonary damage [9]. Hence, it seems reasonable to expect that nicotine, without reactive chemicals, must be less toxic than nicotine delivered with a mixture of combustion-generated toxins. This expectation derives the oft-repeated mantra that “people smoke for nicotine, but they die from tar” [10]. And from it, it follows that if all the tar (as well as other combustion products) were removed, inhaling nicotine will be much safer. Unfortunately, for many reasons, the situation is more complicated than expected.
First, avoiding combustion does not remove all noxious chemicals. Although e-cigarettes do not form high levels of strongly carcinogenic benzopyrenes and tobacco-specific nitrosamines, heating mixtures of nicotine and propylene glycol and vegetable glycerin (PG:VG) in e-cigarettes generates reactive carbonyls such as formaldehyde, acetaldehyde, and acrolein [11,12,13,14], which have been variably linked to carcinogenesis [15] , cardiovascular injury [16, 17], and increased risk of cardiovascular disease [18]. The generation of carbonyls from e-cigarettes varies with use patterns, e-liquid ingredients, and operating conditions [19], and even though the extent of carbonyl generation by e-cigarettes is generally lower than by combustible cigarettes, daily carbonyl exposure from e-cigarettes could still exceed exposure limits [20]. Second, e-cigarette aerosols sporadically contain metals (Fe, Ni, Cu, Cr, Zn, Pb), generated by the heating coil [21], which could add to the toxicity of the aerosol. Third, like combustible cigarettes, e-cigarettes produce aerosols that contain fine and ultrafine particles [22], which can trigger cardiovascular events and promote the progression of pulmonary and cardiovascular disease [23]. Finally, a direct comparison of the relative toxicity of e-cigarettes and combustible cigarettes may not be entirely meaningful. Toxicity due to a chemical, drug, or exposure depends upon its dose. Therefore, even though per puff, e-cigarettes may generate lower levels of toxins; their toxicity may approach that of combustible cigarettes if the use of e-cigarettes (exposure/dose) is higher than that of combustible cigarettes. For instance, if e-cigarettes are half as harmful as combustible cigarettes, but are used twice as much, there would be little harm reduction by using e-cigarettes over combustible cigarettes. Therefore, for both e-cigarettes and combustible cigarettes, harm could be reduced only by reducing exposure. Here too, the relationship is not straightforward. The dose response relationship between smoking and ischemic heart disease, for instance, is non-linear. It shows that smoking just 3 cigarettes a day imparts 80% of the harm attributable to smoking 20–40 cigarettes per day [24•]. In other words, 85–92% reduction in exposure results in only 20% harm reduction. Therefore, reducing toxin exposure by using e-cigarettes may not result in proportional harm reduction. Indeed, as discussed below, recent evidence suggests that even though e-cigarettes generate lower levels of toxins than combustible cigarettes, their use may be associated with significant cardiorespiratory injury as well as immune dysregulation.
E-Cigarettes and Respiratory Injury
The lungs are the major site of exposure to inhaled substances. In case of both combustible cigarettes and e-cigarettes, chemicals suspended in aerosols are first inhaled into the lungs and then circulated systemically. As a result, pulmonary cells become the first site of action of inhaled chemicals. Therefore, it is not surprising that chronic inhalation of tobacco smoke is associated with exacerbation of pulmonary diseases such as asthma, emphysema, chronic obstructive pulmonary disease (COPD), and lung cancer [25]. Although, it is still unknown whether e-cigarettes impair lung function in a manner analogous to combustible cigarettes, accumulating evidence suggests that the use of e-cigarettes may be associated with significant lung injury and an increase in the risk of respiratory disease. In an analysis of 705,159 participants of the Behavioral Risk Factor Surveillance System, current e-cigarette use was found to be associated with 75% higher odds of chronic bronchitis, emphysema, or COPD compared with never e-cigarette users, suggesting that the use of e-cigarettes may be associated with pulmonary toxicity, including in those who had never smoked combustible cigarettes [26••]. However, additional work is required to determine whether prolonged use of e-cigarettes increases the risk of COPD or lung cancer. Such data may take decades to appear. E-cigarettes were introduced in the international market only in 2007; therefore, they have not been in use long enough to reveal any potential links with chronic diseases. Nonetheless, as discussed below, emerging data from animal models support the view that exposure to e-cigarettes could result in overt or sub-threshold respiratory injury.
Genotoxicity of E-Cigarettes
Several studies using animal model and cellular systems have reported that exposure to e-cigarette aerosols or extracts results in genotoxic effects such as DNA damage or inhibition of DNA repair. Much like exposure to combustible cigarettes, mice exposed to e-cigarette aerosol have been reported to develop lung adenocarcinomas and bladder urothelial hyperplasia, both of which are extremely rare in mice exposed to vehicle control or filtered air [27••]. Although in this study mice were exposed to e-cigarette aerosols at levels much higher than expected in humans, the results do raise the possibility that e-cigarettes have the capacity to initiate tumorigenic or carcinogenic changes. Additional support for this possibility is provided by studies showing that e-cigarette aerosol-exposed mice have significant amounts of O6-medG adducts in the lung, bladder, and heart; and that nicotine and its metabolite–nicotine-derived nitrosamine ketone can increase mutational susceptibility and tumorigenic transformation of culture human bronchial epithelial and urothelial cells [28]. Thus, the O6-medG adducts could be formed by the metabolism of nicotine into nitrosamines, which is then converted to N’-nitrosonornicotine (NNN) and 4-(methylnitrosoamino)-1-(3-pyridyl)-1-butanone (NNK). NNK can be further converted to methyldiazohydroxide, which can methylate deoxyguanosines and thymidines in DNA [28, 29]. Therefore, it seems plausible that nicotine in e-cigarette aerosols could increase the risk of carcinogenesis by inducing DNA damage, a possibility further underscored by the observation that exposure to e-cigarette aerosols inhibits DNA repair activity and DNA repair proteins—XPC (xeroderma pigmentosum, complement group C) and OGG1/2 (8-oxoguanine glycosylase) in the lung [28]. DNA damage has also been reported upon exposure of human oral and lung epithelial cells to e-cigarette aerosols [30]. Interestingly, in these cells, the accumulation of DNA damage was also accompanied by a decrease in the expression of OGG1, an enzyme essential for the removal of oxidative DNA damage [30]. Because nicotine is present in all tobacco products, this could be one mechanism by which tobacco products can promote carcinogenesis.
Genotoxic effects of e-cigarettes have been demonstrated in a variety of other cellular models as well. Canistro et al. found that e-cigarettes have a powerful booster effect on phase-I carcinogen-bioactivating enzymes including activators of polycyclic aromatic hydrocarbons (PAHs), and increase production of reactive oxygen species (ROS) and DNA oxidation to 8-hydroxy 2’-deoxyguanosine—co-mutagenic and cancer-initiating effects that can significantly increase the risk of carcinogenesis [31]. Increases in DNA damage have also been observed in human alveolar type II cells, lung epithelial cells, and distal lung tissue explants exposed to e-cigarette aerosols [32, 33]. Although genotoxicity and DNA damage induced by e-cigarette aerosol extract were much lower than with combustible cigarettes, the observation that extracts containing nicotine caused a greater decrease in cell viability and significantly greater DNA damage than those without nicotine [32] suggests that the genotoxicity of e-cigarettes may be attributable in part to nicotine. Although specific mechanisms underlying the toxicity of nicotine containing aerosol extracts were not investigated, these results add to the evidence base implicating nicotine in the genotoxicity of tobacco products.
Effects of E-Cigarettes on Lung Structure and Function
Evidence from animal models suggests that exposure to e-cigarette aerosols could induce structural changes in the lung and significantly compromise lung function. Mice exposed to e-cigarette aerosols show increased bronchoalveolar lavage (BAL) fluid cellularity, Muc5ac production, oxidative stress markers [34], and IL-1β [35], indicating on-going inflammation. Changes in these biomarkers were associated with decrements in parenchymal lung function in terms of both functional residual capacity and high trans-respiratory pressures [36]. Garcia-Arcos et al. report that exposure to e-cigarette aerosols increases airway hyperreactivity, distal space enlargement, mucin production, cytokine, and protease expression in mice, indicating that inhalation of e-cigarettes could trigger effects normally associated with the development of COPD [37]. Significantly, exposure to nicotine-free e-cigarettes did not affect these parameters, which suggests that pulmonary injury induced by e-cigarettes may be in part mediated by nicotine [37]. In rats, exposure to e-cigarette aerosols leads to the appearance disorganized alveolar and bronchial epithelium suggesting incipient pulmonary injury [38]. Chronic exposure to e-cigarette aerosols at levels comparable to the use of e-cigarettes and tobacco cigarettes by humans led to emphysematous lung destruction, with a significant enlargement of alveolar airspace, and loss of peripheral vasculature [39]. In this study, e-cigarettes were as damaging to pulmonary structures as combustible tobacco cigarettes. Moreover, the enlargement of alveolar space and the loss of capillaries were also observed in mice exposed to nicotine [39], suggesting that nicotine by itself may be sufficient to induce COPD-like lung injury, at least in animal models.
Respiratory Effects of E-Cigarettes in Humans
Because several animal studies use high levels of e-cigarette aerosols for exposure and high levels of nicotine, their relevance to the effects of e-cigarette use on pulmonary function in humans remains uncertain. Moreover, some of the results obtained with animal models do not translate to humans as it remains unclear to what extent the pathology seen in animal models may appear in people who use e-cigarettes. However, the few studies that have examined the effects of e-cigarettes in humans have found the acute use of e-cigarettes by smoking-naïve healthy subjects to be associated with increases in flow resistance, indicating obstruction of the conducting airways [40] as well as an increases in serum indices of oxidative stress and ICAM-1 (intercellular adhesion molecule 1), reaching a peak approximately 1–2 h after inhalation of e-cigarette aerosols, suggesting tissue injury and inflammation [41]. In addition, BALF from chronic e-cigarette users shows significant inflammatory changes as indicated by increased levels of in neutrophil, elastase, matrix metalloproteases (MMP) 2, and 9 activities from nonsmokers [42], and their airways appear “friable and erythematous,” indicating on-going subclinical injury [43•]. Daily e-cigarette use, without concurrent or past tobacco use, was also associated with a significant decrease in lung function (as measured by forced expiratory volume FEV1 and the ratio of FEV1 and FVC, forced vital capacity) [44], suggesting that some of the pulmonary effects of e-cigarettes in animal models are also seen in humans.
In comparison with non-smokers, the levels of neutrophil elastase, MMP-2, MMP-9 activities were elevated in BALF from e-cigarette users, suggesting that repeated use of e-cigarettes disrupts the protease-antiprotease balance by increasing proteolysis in the lung, which may increase the risk of developing chronic lung disease [42]. Induced sputum from e-cigarette users show elevated levels of elastase and MMP-9, which are innate defense proteins associated with COPD [45]. Interestingly, bronchial brush biopsies and lavage samples reveal approximately 300 proteins differentially expressed in airways of e-cigarette users, a pattern of changes different from those seen in smokers [43•]. In addition, sporadic case reports document diffuse alveolar hemorrhage syndrome [46] and hypersensitive pneumonitis accompanied by interlobular septal thickening and pleural effusions [47], suggesting that the use of e-cigarettes could lead to subacute respiratory injury or failure even in young adults.
The use of e-cigarettes could also exacerbate asthma. Although not much is known about e-cigarettes and incident asthma, there is evidence to suggest that individuals with mild asthma who use e-cigarettes have worse respiratory outcomes than non-tobacco product users as evidenced by increased respirator total impedance, respiratory system resistance [48]. However, a 3.5-year observational study of a cohort of nine daily e-cigarette users found no respiratory symptoms and no pathological changes in the lung [49]. In contrast, cases of eosinophilic inflammation, alveolar bleeding, and acute ground-glass lung opacities as well as fibrosis have been reported in individuals using e-cigarettes only for a few months [50]. Such contradictory findings suggest that the adverse effects of e-cigarettes may be a more sporadic and may be limited to some, potentially more sensitive individuals or to specific products, constituents, and use patterns.
Perhaps, the most striking manifestation of e-cigarette-induced lung injury is evidenced by cases of e-cigarette or vaping-induced lung injury (EVALI) reported in 2019–2020. As of February 2020, a total of 2087 hospitalized cases or death have been reported by the Centers for Disease Control (CDC) [51]. Evaluation of 10 lung biopsies showed that EVALI was characterized by acute to subacute lung injury, multifocal ground glass-opacity, frequently with organizing consolidation, interlobular septal thickening, diffuse alveolar damage, and organizing pneumonia, changes indicative of extensive lung damage, fluid accumulation, airway collapse, and fibrosis that often resulted in death [52]. Although the specific e-cigarette constituents responsible for the EVALI outbreak are yet to be unambiguously identified, the observation that vitamin E acetate, tetrahydrocannabinol (THC), or its metabolites were identified in BALF from most EVALI cases [53] indicates that additives or cutting agents added to the e-liquids may be important contributing factors, even though some EVALI patients reported using only nicotine-containing products [54]. Regardless of the triggering agent, the national outbreak of EVALI brought to fore not only the risk of inhaling mixtures of unknown constituents, but also the risk that may be associated with the use of e-cigarettes. Many EVALI patients had a history of asthma, cardiac disease, or obesity [55], which may have made them more susceptible to pulmonary injury.
Cardiovascular Effects of E-Cigarettes
In addition to the pulmonary cells, the cardiovascular tissue is also a major target of e-cigarettes. We know from previous work that the heart, blood vessels, and blood constituents are highly sensitive to inhaled toxins [56]. Indeed, cardiovascular disease is a major cause of morbidity and mortality in smokers, and smoking contributes to 17% of all cardiovascular deaths globally, about 3 million deaths per year [57]. However, in contrast with carcinogenesis, the effects of smoking on ischemic heart disease appear at lower levels of exposure [24•] and may be due to tobacco smoke constituents different from those that cause cancer [58]. Moreover, many of the cardiovascular effects of smoking may be related to nicotine, which stimulates the sympathetic nervous system [59], and acts additively with angiotensin II to promote cardiovascular remodeling [60]. Therefore, it is not surprising that acute use of e-cigarettes increases blood pressure and heart rate.
Human Studies
In healthy adults, the use of e-cigarettes leads to an acute increase in both systolic and diastolic blood pressure as well as aortic stiffness [40, 61] to a magnitude similar to that observed with smoking a combustible cigarette [62]. These effects are accompanied by a marked shift in cardiac sympathovagal balance towards sympathetic predominance, as indicated by an increase in the low-frequency component of heart rate variability [63••]. Because such sympathomimetic effects are not seen in e-cigarettes without nicotine [63••], it is likely that nicotine is the main constituent that elicits the hemodynamic changes seen after acute inhalation of e-cigarette aerosols. Habitual use of e-cigarettes has been found to be associated with a shift in cardiac autonomic balance towards sympathetic predominance [64]. Because chronic sympathetic hyperactivity increases cardiovascular workload and hemodynamic stress and predisposes to endothelial dysfunction, coronary spasms, left ventricular hypertrophy, and arrhythmias [65], and it increases mortality risk, [66] it seems plausible that the persistent sympathetic predominance in e-cigarette users may be indicative of incipient cardiovascular injury, which over time may develop into clinically meaningful pathology.
Further evidence that the use of e-cigarettes impairs cardiovascular function is provided by studies showing that the use of e-cigarettes decreases flow-mediated dilation (FMD) [67, 68, 69•], peak velocity, and the hyperemic index [67], while increasing arterial stiffness [61] and diminishing acetylcholine-mediated vasodilation [61]. The decrease in FMD observed in humans inhaling e-cigarette aerosol has been recapitulated in rats exposed to aerosols derived from JUUL and other previous generation e-cigarettes [70•]. Even though FMD changes in response to e-cigarettes are lower than those observed with combustible cigarettes [69•], the observations that the use of e-cigarette is associated with an increase in oxidative stress [41, 68, 69•] and decreased bioavailability of nitric oxide [69•] and as well as diminished rates of nitric oxide production from endothelial cells [71] support the notion that e-cigarettes cause endothelial injury. Decreased nitric oxide production in endothelial cells has also been noted in endothelial cells exposed to flavoring agents used in e-cigarettes [72,73,74]. Acute exposure to e-cigarettes also increases the levels of circulating endothelial progenitor cells to levels similar in magnitude to that observed after smoking a combustible cigarette [75], and elevates the levels of circulating extracellular vesicles derived from the endothelium in healthy individuals [76], suggesting that using e-cigarettes could compromise vascular repair and incite vascular injury.
Cardiotoxicity of E-Cigarettes in Experimental Models
That inhalation of e-cigarettes could lead to vascular impairment is further supported by evidence from in vitro studies and animal models. In cell culture systems, exposure to condensates of e-cigarette aerosol decrease endothelial permeability, and exposure to nicotine by itself triggers dose-dependent loss of endothelial barrier and inhibits cell proliferation [13]. However, inhalation of e-cigarettes may also generate stable toxins in the plasma that could induce toxicity. When exposed to serum isolated from e-cigarette users, human-induced pluripotent stem cell-derived endothelial cells show an increase in ROS production and cytokine expression as well as a loss of pro-angiogenic properties [77], suggesting that inhalation of e-cigarettes could result in the generation of metastable toxins that can diffuse from the lung to the blood, leading to systemic toxicity. Many of these cellular changes (such as loss of barrier function) may be linked directly to nicotine [13], but other more toxic change may be due to reactive products such as acrolein [13], which are generated from the degradation of PG:VG and may affect the lung and blood vessels independent of nicotine.
In concordance with data obtained from cell culture system, evidence from animal models supports the view that the use of e-cigarettes may be associated with significant cardiovascular injury. In mice, inhalation of e-cigarette aerosols—4h/day/5 days/week for 8 month—has been reported to lead to 2.5- to 2.8-fold increase in aortic arterial stiffness, and a decrease in maximal aortic relaxation to methacholine [78]. Although these effects were similar to those observed with combustible cigarettes, exposure to e-cigarette alone did not lead to emphysema-associated changes in respiratory function as seen in mice exposed to combustible cigarettes [78], suggesting that combustible cigarettes are more potent than e-cigarettes in inducing emphysema in mice. Kuntic et al. [68] have reported that in mice, exposure to e-cigarette aerosols has detrimental effects on endothelial function, markers of oxidative stress, inflammation, and lipid peroxidation. The authors found that increased oxidative stress by e-cigarettes was mediated by the activation of NADPH oxidase (NOX-2), and was recapitulated by acrolein, suggesting that acrolein may be a key mediator of increases in vascular, cerebral, and pulmonary oxidative stress, secondary to e-cigarette aerosol inhalation [68]. To study the effects of tobacco smoke and e-cigarettes on atherogenesis, Szostak et al. exposed apoE-null mice to these aerosols for 6 months. They found that e-cigarette aerosols increased pulse wave velocity and arterial stiffness, although these effects were smaller than those observed with combustible tobacco smoke [79]. In addition to vascular changes, exposure to e-cigarette aerosol in mice has also been shown to increase platelet aggregation, and shorten thrombosis occlusion and bleeding time [80], changes that could establish a pro-thrombotic state in humans and increase the risk of cardiovascular events. However, whether e-cigarettes affect thrombotic responses in humans has not been studied, but merits further investigation.
E-Cigarettes and the Immune Response
Human Studies
Although the effects of e-cigarettes on immunity are only beginning to be studied, emerging evidence suggests that e-cigarette use affects both innate and acquired immunity. In healthy, smoking-naïve individuals, serum levels of ROS and ICAM-1 increase within 2 h of exposure [41], and chronically, e-cigarette users show an increase in plasma IgE levels [81], suggesting that inhalation of e-cigarette aerosol may be a significant immune challenge, leading to the activation of multiple inflammatory responses. Nasal scrape biopsies from e-cigarette users show a decrease in the expression of a large number of immune-related genes [82]. Because e-cigarette users showed greater suppression of genes than smokers, and because more genes were suppressed by e-cigarette use than by smoking, it appears that even though some of the effects of e-cigarettes and combustible cigarettes may be similar, the use of e-cigarettes induces extensive immune changes that differ from those seen with conventional cigarettes. Although the implications of these findings remain unclear, e-cigarette use associated reduction in chemokines at the level of the epithelium could affect the recruitment and activation of innate immune cells and defense against fungal, bacterial, and viral infection. However, additional work is required to assess the functional consequences of the suppression of immune-related genes in e-cigarette users.
Immunogenic Responses of E-Cigarette Aerosols In Vitro
Data showing the immunological effects of e-cigarettes in humans are complemented by a range of in vitro studies using immune cells. For example, it has been shown that exposure to e-cigarette aerosol extract increases the production of proinflammatory cytokines such as IL-6 by immune cells such as macrophages [83] and dendritic cells [84]. IL-6 production is also increased in primary human airway epithelial cells exposed to e-liquids, and this inflammatory response is amplified by nicotine [85]. In view of these reports, it seems that e-liquids or extracts of e-cigarette aerosols activate both immune and non-immune cells, and the resultant changes in the production of immunomodulating cytokines may result in the development of a pro-inflammatory state in the lung. The development of an inflammatory state may also extend to other tissues and organs as diverse as nasal epithelial cells [86], cerebral cortex [87], and primary small airway epithelial cells [88]. Nevertheless, whether this inflammation is in the causal pathway that contributes to heightened disease risk of e-cigarette use remains unclear.
Stimulation of cytokine production in macrophages by e-cigarette exposure is accompanied by a decrease in their phagocytic activity. Exposure of macrophages to e-cigarette aerosol condensate has been reported to result in a 50-fold increase in ROS production and a significant inhibition of phagocytosis [83], efferocytosis, and bacterial clearance [89], and exposing THP-1 macrophages to e-cigarette aerosol extracts has been shown to decrease the intracellular burden of Mycobacterium tuberculosis [90]. Similarly, when exposed to freshly generated e-cigarette aerosol at the air-liquid interface, alveolar macrophages and neutrophils show reduced anti-microbial activity against Staphylococcus aureus [91]. Taken together, these findings suggest that the use of e-cigarette could suppress the anti-microbial function of both macrophages and neutrophils.
Further evidence supporting the view that e-cigarette use may interfere with anti-microbial activity comes from studies showing that epithelial cells exposed to e-cigarette aerosols are more susceptible to infection when challenged by Porphyromonas gingivalis and Fusobacterium nucleatum [92], suggesting that e-cigarette constituents can prevent microbial clearance by the epithelium. Additionally, human neutrophils exposed to e-cigarette aerosols show reduction in chemotaxis, ROS production, and decreased rate of phagocytosis of bacterial bioparticles [93]. Inhalation of nicotine has also been shown to affect dust-mite-induced recruitment of eosinophils in mice [94]. Thus, a combination of an increase in tissue infectivity and decreased chemotaxis and clearance by e-cigarette constituents, including flavors [95, 96], could significantly increase the risk of respiratory infections in e-cigarette users, and significantly modify their allergic response.
Immune Changes in Animal Models
Data from animal models corroborate in vitro results which suggest that e-cigarette constituents induce inflammation and dysregulate anti-microbial responses. Mice inhaling e-cigarette aerosols show an increased number of dendritic cells, CD4+ T cells, and CD19+ B cells in the lung [97], suggesting on-going inflammation. A similar increase in inflammatory cell influx of macrophages and T-lymphocytes and pro-inflammatory cytokines in BALF has been observed in mice chronically exposed to e-cigarettes [98]. The inflammatory state established by e-cigarettes was accompanied by an increase in ACE2 [98], which, given that the protein is involved in binding SARS-CoV-2, might affect susceptibility to infection by the virus. Indeed, in a recent online survey, COVID-19 diagnosis was 5 times more likely among ever-users of e-cigarettes only and 7 times more likely among dual users than non-users [99]. However, additional work is required to substantiate these findings.
In contrast to animal studies showing an increase in airway inflammation upon inhalation of e-cigarette aerosols, Madison et al. [100••] report no increase in pulmonary inflammation or emphysematous changes in the lungs of mice exposed to e-cigarettes for 4 months. Nevertheless, when infected with the flu virus, the e-cigarette-exposed mice showed augmented weight loss, delayed immune responses to infection, persistent lung inflammation, and edema, as well as increased hemorrhage and mortality than mice breathing only room air. Interestingly, macrophages isolated from the BAL fluid of these mice showed increased lipid accumulation. This disruption of lipid homoeostasis in macrophages, which was independent of nicotine, was characterized by a distinct increase in phospholipid species with a concomitant decrease in neutral triglycerides and the expression of Abca1—the macrophage transporter responsible for the removal of intracellular cholesterol and phospholipids. Even though their significance remains to be fully assessed, the changes in macrophage lipid metabolism and transport may be linked to the disruption of innate immune responses and increased susceptibility to inhaled pathogens [100••]. The e-cigarette-induced changes in lipid metabolism of macrophages in mice are particularly interesting because similar lipid-laden macrophages have also been observed in humans who use e-cigarettes, particularly in individuals with e-cigarette-associated pneumonia [101, 102]. Similar lipid-laden macrophages have also been detected in the BAL fluid of EVALI patients [103]. Although such lipid-laden macrophages have also been found in the lung of smokers, in e-cigarette users, these macrophages are associated with inflammatory cytokines such as IL-4 and IL-10, but not with smoking-related cytokines [104], suggesting that the pathophysiological changes induced by e-cigarettes in macrophages may be different in nature from that afflicted by combustible cigarettes.
Perspective and Conclusions
E-cigarettes were developed with the expectation that the delivery of nicotine without combustion-derived chemicals would prevent or minimize most of the adverse effects of smoking. This expectation was based on the belief that nicotine per se has little contribution to the pathology of smoking. However, extensive evidence suggests that this view may not be correct. Work discussed above clearly shows that the hemodynamic effects of e-cigarette use may be due to nicotine alone [63••]. It has also been reported that nicotine by itself could promote DNA damage [28], induce lung injury [37, 39], amplify immune responses [85], and disrupt endothelial barriers [13]. Nonetheless, this toxicity profile of nicotine, thrown in sharp relief by recent findings, is in stark contrast with decades of experience showing a good safety profile of nicotine replacement therapies. Reasons for disparate toxicity profiles of nicotine in different scenarios remain unclear; however, it seems likely that long-term effects of nicotine alone are not well known, or that toxicity of nicotine may depend on the route and speed of administration. That differences in the pharmacokinetics of inhaled and ingested nicotine elicit different effects is highlighted by a recent study showing that inhalation of nicotine-base in mice (twice daily, 5 days/week for 8 weeks) substantially reduced the house dust mite-induced recruitment of eosinophils, as measured in BALF, but oral nicotine administration had no effect [94]. Therefore, the relative activity of dermally or orally administered nicotine versus inhaled nicotine needs to be critically evaluated for an overall assessment of the potential health effects of e-cigarettes. Such considerations should also be extended to the toxicological evaluation of PG:VG, flavors, operating conditions, device types, and use patterns before reliably estimating the intrinsic and the relative harm of e-cigarettes.
In many studies, the effects observed with e-cigarettes are of the same magnitude as those seen with combustible cigarettes; however, in most cases, pathologic changes due to e-cigarettes are milder than those with combustible cigarettes [32, 69•, 79]. Indeed, switching from combustible cigarettes to e-cigarettes has been reported to improve endothelial function and vascular stiffness [105]. However, it is unclear whether this acute improvement in vascular function persists with chronic use of e-cigarettes. Hence, neither short-term improvements nor the relatively milder changes in some parameters with e-cigarettes versus combustible cigarettes imply unalloyed harm reduction. As reported by several investigators [43•, 100••, 104], the nature and the type of tissue injury inflicted by e-cigarettes are distinct from that caused by combustible cigarettes. For instance, even though in animal models, e-cigarettes, unlike combustible cigarettes, do not cause emphysematous changes, they stimulate the accumulation of lipid-laden macrophages, which could lead to dysregulation of the pulmonary surfactant and thereby compromise air-exchange and alter innate immunity [100••], pathological changes distinct from those seen with combustible cigarettes. Likewise, e-cigarettes alter the expression of many more genes than combustible cigarettes and the pattern of these changes differ between the two products [43•]. Therefore, comparing e-cigarettes with combustible cigarettes using the same readouts and endpoints may be misleading as the two exposures differ markedly in the nature of the injury they induce and the types of tissues they affect. Finally, that e-cigarettes may be less harmful than combustible cigarettes may be irrelevant to sole e-cigarette users, because there is incontrovertible evidence that the use of e-cigarettes is significantly more harmful than not using nicotine and tobacco products at all. Given that a high proportion of e-cigarette use is now among tobacco-naïve youth [5], the absolute harm associated with the use of these devices (independent of their harm relative to combustible cigarettes) needs to be further investigated and highlighted.
In summary, the weight-of-evidence discussed above warrants the view that the use of e-cigarettes has multiple adverse health effects. Acute use of e-cigarettes leads to an increase in heart rate and blood pressure [40], as well as obstruction of conducting airways [39], and arterial stiffness [61]. Flow-mediated dilation is diminished [69•], transcutaneous oxygen tension is decreased [106], and a characteristic immune response [40, 41, 81] is activated. Chronic use of e-cigarettes has been found to be associated with a shift in cardiac autonomic balance towards sympathetic predominance [64] and dysregulation of immune-related genes [82]. In animal models, long-term exposure to e-cigarette aerosols lead to DNA damage and inhibition of DNA repair and the development of adenocarcinoma and bladder urothelial hyperplasia [28]. Lipid-laden macrophages accumulate in the lung, accompanied by extensive changes in lipid metabolism and transport [100••]. Taken together, these observations raise the possibility that habitual use of e-cigarettes could cause tissue injury, which could compromise lung function and increase the risk of developing heart disease and stroke. The use of e-cigarettes could also compromise the ability to remove microbial pathogens and thereby increase susceptibility to viral, fungal, and bacterial infection. Data from experimental models also support the notion that the use of e-cigarettes could increase the risk of developing several types of cancer. Nevertheless, it remains to be seen whether long-term use of e-cigarettes is indeed associated with such adverse events in humans.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130:1418–36.
Mirbolouk M, Charkhchi P, Kianoush S, Uddin SI, Orimoloye OA, Jaber R, et al. Prevalence and distribution of e-cigarette use among US adults: behavioral risk factor surveillance system, 2016. Ann Intern Med. 2018;169:429–38.
Obisesan OH, Osei AD, Uddin SMI, Dzaye O, Mirbolouk M, Stokes A and Blaha MJ. Trends in e-cigarette use in adults in the United States, 2016-2018. JAMA Internal Medicine. 2020;180:1394–1398.
https://www.cdc.gov/nchs/nhis/erkeyindicators.htm. Accessed 16 Jan 2021.
Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, King BA. E-cigarette use among middle and high school students - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1310–2.
Tam J. E-cigarette, combustible, and smokeless tobacco product use combinations among youth in the united states, 2014-2019. Addict Behav. 2020;112:106636.
Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23:133–9.
Bhatnagar A. Cardiovascular perspective of the promises and perils of e-cigarettes. Circ Res. 2016;118:1872–5.
Goldman LR, Benowitz N, Bhatnagar A, Dominici F, Fienberg S, Friedman GD, Hammond SK, He J, Oparil S, Peterson E, Trapido E. Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. Report of the Institute of Medicine of the National Academies. 2009.
Russell MA. Low-tar medium-nicotine cigarettes: a new approach to safer smoking. Br Med J. 1976;1:1430–3.
Belushkin M, Tafin Djoko D, Esposito M, Korneliou A, Jeannet C, Lazzerini M, et al. Selected harmful and potentially harmful constituents levels in commercial e-cigarettes. Chem Res Toxicol. 2020;33:657–68.
Kosmider L, Kimber CF, Kurek J, Corcoran O, Dawkins LE. Compensatory puffing with lower nicotine concentration e-liquids increases carbonyl exposure in e-cigarette aerosols. Nicotine Tob Res. 2018;20:998–1003.
Schweitzer KS, Chen SX, Law S, Van Demark M, Poirier C, Justice MJ, et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. Am J Phys Lung Cell Mol Phys. 2015;309:L175–87.
Ogunwale MA, Li M, Ramakrishnam Raju MV, Chen Y, Nantz MH, Conklin DJ, et al. Aldehyde detection in electronic cigarette aerosols. ACS Omega. 2017;2:1207–14.
Schwilk E, Zhang L, Smith MT, Smith AH, Steinmaus C. Formaldehyde and leukemia: an updated meta-analysis and evaluation of bias. J Occup Environ Med. 2010;52:878–86.
Augenreich M, Stickford J, Stute N, Koontz L, Cope J, Bennett C and Ratchford SM. Vascular dysfunction and oxidative stress caused by acute formaldehyde exposure in female adults. American Journal of Physiology-Heart and Circulatory Physiology. 2020;319:H1369–H1379.
Srivastava S, Sithu SD, Vladykovskaya E, Haberzettl P, Hoetker DJ, Siddiqui MA, et al. Oral exposure to acrolein exacerbates atherosclerosis in apoE-null mice. Atherosclerosis. 2011;215:301–8.
DeJarnett N, Conklin DJ, Riggs DW, Myers JA, O’Toole TE, Hamzeh I, Wagner S, Chugh A, Ramos KS and Srivastava S. Acrolein exposure is associated with increased cardiovascular disease risk. Journal of the American Heart Association. 2014;3:e000934.
Ward AM, Yaman R, Ebbert JO. Electronic nicotine delivery system design and aerosol toxicants: a systematic review. PLoS One. 2020;15:e0234189.
Son Y, Bhattarai C, Samburova V and Khlystov A. Carbonyls and carbon monoxide emissions from electronic cigarettes affected by device type and use patterns. Int J Environ Res Public Health. 2020;17:2767.
Olmedo P, Goessler W, Tanda S, Grau-Perez M, Jarmul S, Aherrera A, et al. Metal concentrations in e-cigarette liquid and aerosol samples: the contribution of metallic coils. Environ Health Perspect. 2018;126:027010.
Schober W, Szendrei K, Matzen W, Osiander-Fuchs H, Heitmann D, Schettgen T, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217:628–37.
Kaufman JD, Elkind MS, Bhatnagar A, Koehler K, Balmes JR, Sidney S, Burroughs Peña MS, Dockery DW, Hou L, Brook RD. Guidance to reduce the cardiovascular burden of ambient air pollutants: a policy statement from the American Heart Association. Circulation. 2020;142:e432–e447.
Pope CA 3rd, Burnett RT, Turner MC, Cohen A, Krewski D, Jerrett M, et al. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure-response relationships. Environ Health Perspect. 2011;119:1616–21 This study shows a non-linear dose-response relationship between smoking and ischemic heart disease.
US Department of Health and Human Services. "The health consequences of smoking—50 years of progress: a report of the Surgeon General." (2014). The health consequences of smoking—50 years of progress: a report of the surgeon general. In US Department of Health and Human Services: Citeseer; 2014.
Osei AD, Mirbolouk M, Orimoloye OA, Dzaye O, Uddin SMI, Benjamin EJ, et al. Association between e-cigarette use and chronic obstructive pulmonary disease by smoking status: behavioral risk factor surveillance system 2016 and 2017. Am J Prev Med. 2020;58:336–42 Analysis of a large observational study of 705,159 participants showing an association between e-cigarette use and chronic bronchitis, emphysema, and chronic obstructive pulmonary disease.
Tang MS, Wu XR, Lee HW, Xia Y, Deng FM, Moreira AL, et al. Electronic-cigarette smoke induces lung adenocarcinoma and bladder urothelial hyperplasia in mice. Proc Natl Acad Sci U S A. 2019;116:21727–31 Direct evidence showing that exposure to e-cigarettes causes cancer in an animal model.
Lee HW, Park SH, Weng MW, Wang HT, Huang WC, Lepor H, et al. E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proc Natl Acad Sci U S A. 2018;115:E1560–9.
Kankanamage RNT, Ghosh AB, Jiang D, Gkika K, Keyes T, Achola LA, et al. Metabolites of tobacco- and e-cigarette-related nitrosamines can drive Cu(2+)-mediated DNA oxidation. Chem Res Toxicol. 2020;33:2072–86.
Ganapathy V, Manyanga J, Brame L, McGuire D, Sadhasivam B, Floyd E, et al. Electronic cigarette aerosols suppress cellular antioxidant defenses and induce significant oxidative DNA damage. PLoS One. 2017;12:e0177780.
Canistro D, Vivarelli F, Cirillo S, Babot Marquillas C, Buschini A, Lazzaretti M, et al. E-cigarettes induce toxicological effects that can raise the cancer risk. Sci Rep. 2017;7:2028.
Rankin GD, Wingfors H, Uski O, Hedman L, Ekstrand-Hammarstrom B, Bosson J, et al. The toxic potential of a fourth-generation E-cigarette on human lung cell lines and tissue explants. J Appl Toxicol. 2019;39:1143–54.
Bahmed K, Lin CR, Simborio H, Karim L, Aksoy M, Kelsen S, et al. The role of DJ-1 in human primary alveolar type II cell injury induced by e-cigarette aerosol. Am J Phys Lung Cell Mol Phys. 2019;317:L475–85.
Glynos C, Bibli SI, Katsaounou P, Pavlidou A, Magkou C, Karavana V, et al. Comparison of the effects of e-cigarette vapor with cigarette smoke on lung function and inflammation in mice. Am J Phys Lung Cell Mol Phys. 2018;315:L662–72.
Husari A, Shihadeh A, Talih S, Hashem Y, El Sabban M, Zaatari G. Acute exposure to electronic and combustible cigarette aerosols: effects in an animal model and in human alveolar cells. Nicotine Tob Res. 2016;18:613–9.
Larcombe AN, Janka MA, Mullins BJ, Berry LJ, Bredin A, Franklin PJ. The effects of electronic cigarette aerosol exposure on inflammation and lung function in mice. Am J Phys Lung Cell Mol Phys. 2017;313:L67–79.
Garcia-Arcos I, Geraghty P, Baumlin N, Campos M, Dabo AJ, Jundi B, et al. Chronic electronic cigarette exposure in mice induces features of COPD in a nicotine-dependent manner. Thorax. 2016;71:1119–29.
Cirillo S, Vivarelli F, Turrini E, Fimognari C, Burattini S, Falcieri E, et al. The customizable e-cigarette resistance influences toxicological outcomes: lung degeneration, inflammation and oxidative stress-induced in a rat model. Toxicol Sci. 2019;172:132–145.
Reinikovaite V, Rodriguez IE, Karoor V, Rau A, Trinh BB, Deleyiannis FW, et al. The effects of electronic cigarette vapour on the lung: direct comparison to tobacco smoke. Eur Respir J. 2018;51.
Antoniewicz L, Brynedal A, Hedman L, Lundback M, Bosson JA. Acute effects of electronic cigarette inhalation on the vasculature and the conducting airways. Cardiovasc Toxicol. 2019;19:441–50.
Chatterjee S, Tao JQ, Johncola A, Guo W, Caporale A, Langham MC, et al. Acute exposure to e-cigarettes causes inflammation and pulmonary endothelial oxidative stress in nonsmoking, healthy young subjects. Am J Phys Lung Cell Mol Phys. 2019;317:L155–66.
Ghosh A, Coakley RD, Ghio AJ, Muhlebach MS, Esther CR Jr, Alexis NE, et al. Chronic e-cigarette use increases neutrophil elastase and matrix metalloprotease levels in the lung. Am J Respir Crit Care Med. 2019;200:1392–401.
Ghosh A, Coakley RC, Mascenik T, Rowell TR, Davis ES, Rogers K, et al. Chronic e-cigarette exposure alters the human bronchial epithelial proteome. Am J Respir Crit Care Med. 2018;198:67–76 The study shows a unique signature of gene expression changes due to e-cigarette exposure.
Meo SA, Ansary MA, Barayan FR, Almusallam AS, Almehaid AM, Alarifi NS, et al. Electronic cigarettes: impact on lung function and fractional exhaled nitric oxide among healthy adults. Am J Mens Health. 2019;13:1557988318806073.
Reidel B, Radicioni G, Clapp PW, Ford AA, Abdelwahab S, Rebuli ME, et al. E-cigarette use causes a unique innate immune response in the lung, involving increased neutrophilic activation and altered mucin secretion. Am J Respir Crit Care Med. 2018;197:492–501.
Agustin M, Yamamoto M, Cabrera F, Eusebio R. Diffuse alveolar hemorrhage induced by vaping. Case Rep Pulmonol. 2018;2018:9724530.
Sommerfeld CG, Weiner DJ, Nowalk A, Larkin A. Hypersensitivity pneumonitis and acute respiratory distress syndrome from e-cigarette use. Pediatrics. 2018;141, e20163927.
Lappas AS, Tzortzi AS, Konstantinidi EM, Teloniatis SI, Tzavara CK, Gennimata SA, et al. Short-term respiratory effects of e-cigarettes in healthy individuals and smokers with asthma. Respirology. 2018;23:291–7.
Polosa R, Cibella F, Caponnetto P, Maglia M, Prosperini U, Russo C, et al. Health impact of E-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked. Sci Rep. 2017;7:13825.
Suhling H, Welte T, Fuehner T. Three patients with acute pulmonary damage following the use of e-cigarettes-a case series. Dtsch Arztebl Int. 2020;117:177–82.
https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#latest-information. Accessed 10 Jan 2021.
Reagan-Steiner S, Gary J, Matkovic E, Ritter JM, Shieh WJ, Martines RB, et al. Pathological findings in suspected cases of e-cigarette, or vaping, product use-associated lung injury (EVALI): a case series. Lancet Respir Med. 2020;8:1219–32.
Blount BC, Karwowski MP, Shields PG, Morel-Espinosa M, Valentin-Blasini L, Gardner M, et al. Vitamin e acetate in bronchoalveolar-lavage fluid associated with EVALI. N Engl J Med. 2020;382:697–705.
Ghinai I, Navon L, Gunn JKL, Duca LM, Brister S, Love S, et al. Characteristics of persons who report using only nicotine-containing products among interviewed patients with e-cigarette, or vaping, product use-associated lung injury - Illinois, August-December 2019. MMWR Morb Mortal Wkly Rep. 2020;69:84–9.
Werner AK, Koumans EH, Chatham-Stephens K, Salvatore PP, Armatas C, Byers P, et al. Hospitalizations and deaths associated with EVALI. N Engl J Med. 2020;382:1589–98.
Bhatnagar A. Cardiovascular pathophysiology of environmental pollutants. Am J Phys Heart Circ Phys. 2004;286:H479–85.
http://www.healthdata.org/data-visualization/tobacco-visualization. Accessed 10 Jan 2021.
Haussmann H-J. Use of hazard indices for a theoretical evaluation of cigarette smoke composition. Chem Res Toxicol. 2012;25:794–810.
Bhatnagar A. E-cigarettes and cardiovascular disease risk: evaluation of evidence, policy implications, and recommendations. Curr Cardiovasc Risk Rep. 2016;10:24.
Colombo ES, Davis J, Makvandi M, Aragon M, Lucas SN, Paffett ML, et al. Effects of nicotine on cardiovascular remodeling in a mouse model of systemic hypertension. Cardiovasc Toxicol. 2013;13:364–9.
Chaumont M, de Becker B, Zaher W, Culie A, Deprez G, Melot C, et al. Differential effects of e-cigarette on microvascular endothelial function, arterial stiffness and oxidative stress: a randomized crossover trial. Sci Rep. 2018;8:10378.
Vlachopoulos C, Ioakeimidis N, Abdelrasoul M, Terentes-Printzios D, Georgakopoulos C, Pietri P, et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers. J Am Coll Cardiol. 2016;67:2802–3.
Moheimani RS, Bhetraratana M, Peters KM, Yang BK, Yin F, Gornbein J, et al. Sympathomimetic effects of acute e-cigarette use: role of nicotine and non-nicotine constituents. J Am Heart Assoc. 2017;6:e006579. This study provides clear evidence that the hemodynamic effects of e-cigarettes are due to nicotine.
Moheimani RS, Bhetraratana M, Yin F, Peters KM, Gornbein J, Araujo JA, et al. Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: implications for cardiovascular risk. JAMA Cardiol. 2017;2:278–84.
Metra M, Nodari S, D’Aloia A, Bontempi L, Boldi E, Cas LD. A rationale for the use of beta-blockers as standard treatment for heart failure. Am Heart J. 2000;139:511–21.
Tsuji H, Venditti FJ Jr, Manders ES, Evans JC, Larson MG, Feldman CL, et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation. 1994;90:878–83.
Caporale A, Langham MC, Guo W, Johncola A, Chatterjee S, Wehrli FW. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology. 2019;293:97–106.
Kuntic M, Oelze M, Steven S, Kroller-Schon S, Stamm P, Kalinovic S, et al. Short-term e-cigarette vapour exposure causes vascular oxidative stress and dysfunction: evidence for a close connection to brain damage and a key role of the phagocytic NADPH oxidase (NOX-2). Eur Heart J. 2020;41:2472–83.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150:606–12 First study to show that inhalation of e-cigarette affects flow-mediated dialation.
Rao P, Liu J, Springer ML. JUUL and combusted cigarettes comparably impair endothelial function. Tob Regul Sci. 2020;6:30–7 This study replicates e-cigarette-induced changes in flow-mediated dilation in well-controlled animal model.
Fetterman JL, Keith RJ, Palmisano JN, McGlasson KL, Weisbrod RM, Majid S, et al. Alterations in vascular function associated with the use of combustible and electronic cigarettes. J Am Heart Assoc. 2020;9:e014570.
Wolkart G, Kollau A, Stessel H, Russwurm M, Koesling D, Schrammel A, et al. Effects of flavoring compounds used in electronic cigarette refill liquids on endothelial and vascular function. PLoS One. 2019;14:e0222152.
Fetterman JL, Weisbrod RM, Feng B, Bastin R, Tuttle ST, Holbrook M, et al. Flavorings in tobacco products induce endothelial cell dysfunction. Arterioscler Thromb Vasc Biol. 2018;38:1607–15.
Noel JC, Rainer D, Gstir R, Rainer M, Bonn G. Quantification of selected aroma compounds in e-cigarette products and toxicity evaluation in HUVEC/Tert2 cells. Biomed Chromatogr. 2020;34:e4761.
Antoniewicz L, Bosson JA, Kuhl J, Abdel-Halim SM, Kiessling A, Mobarrez F, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85.
Mobarrez F, Antoniewicz L, Hedman L, Bosson JA, Lundback M. Electronic cigarettes containing nicotine increase endothelial and platelet derived extracellular vesicles in healthy volunteers. Atherosclerosis. 2020;301:93–100.
Lee WH, Ong SG, Zhou Y, Tian L, Bae HR, Baker N, et al. modeling cardiovascular risks of e-cigarettes with human-induced pluripotent stem cell-derived endothelial cells. J Am Coll Cardiol. 2019;73:2722–37.
Olfert IM, DeVallance E, Hoskinson H, Branyan KW, Clayton S, Pitzer CR, et al. Chronic exposure to electronic cigarettes results in impaired cardiovascular function in mice. J Appl Physiol (1985). 2018;124:573–82.
Szostak J, Wong ET, Titz B, Lee T, Wong SK, Low T, et al. A 6-month systems toxicology inhalation study in ApoE(-/-) mice demonstrates reduced cardiovascular effects of E-vapor aerosols compared with cigarette smoke. Am J Physiol Heart Circ Physiol. 2020;318:H604–31.
Qasim H, Karim ZA, Silva-Espinoza JC, Khasawneh FT, Rivera JO, Ellis CC, et al. Short-term e-cigarette exposure increases the risk of thrombogenesis and enhances platelet function in mice. J Am Heart Assoc. 2018;7:e009264.
Jackson M, Singh KP, Lamb T, McIntosh S, Rahman I. Flavor preference and systemic immunoglobulin responses in e-cigarette users and waterpipe and tobacco smokers: a pilot study. Int J Environ Res Public Health. 2020;17:640.
Martin EM, Clapp PW, Rebuli ME, Pawlak EA, Glista-Baker E, Benowitz NL, et al. E-cigarette use results in suppression of immune and inflammatory-response genes in nasal epithelial cells similar to cigarette smoke. Am J Phys Lung Cell Mol Phys. 2016;311:L135–44.
Scott A, Lugg ST, Aldridge K, Lewis KE, Bowden A, Mahida RY, et al. Pro-inflammatory effects of e-cigarette vapour condensate on human alveolar macrophages. Thorax. 2018;73:1161–9.
Chen IL, Todd I, Tighe PJ, Fairclough LC. Electronic cigarette vapour moderately stimulates pro-inflammatory signalling pathways and interleukin-6 production by human monocyte-derived dendritic cells. Arch Toxicol. 2020;94:2097–112.
Wu Q, Jiang D, Minor M, Chu HW. Electronic cigarette liquid increases inflammation and virus infection in primary human airway epithelial cells. PLoS One. 2014;9:e108342.
Rouabhia M, Piche M, Corriveau MN, Chakir J. Effect of e-cigarettes on nasal epithelial cell growth, Ki67 expression, and pro-inflammatory cytokine secretion. Am J Otolaryngol. 2020;41:102686.
Prasedya ES, Ambana Y, Martyasari NWR, Aprizal Y. Nurrijawati, Sunarpi: Short-term E-cigarette toxicity effects on brain cognitive memory functions and inflammatory responses in mice. Toxicol Res. 2020;36:267–73.
Gellatly S, Pavelka N, Crue T, Schweitzer KS, Day BJ, Min E, et al. Nicotine-free e-cigarette vapor exposure stimulates il6 and mucin production in human primary small airway epithelial cells. J Inflamm Res. 2020;13:175–85.
Serpa GL, Renton ND, Lee N, Crane MJ, Jamieson AM. Electronic nicotine delivery system aerosol-induced cell death and dysfunction in macrophages and lung epithelial cells. Am J Respir Cell Mol Biol. 2020;63:306–16.
Gomez AC, Rodriguez-Fernandez P, Villar-Hernandez R, Gibert I, Muriel-Moreno B, Lacoma A, et al. E-cigarettes: effects in phagocytosis and cytokines response against Mycobacterium tuberculosis. PLoS One. 2020;15:e0228919.
Hwang JH, Lyes M, Sladewski K, Enany S, McEachern E, Mathew DP, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med (Berl). 2016;94:667–79.
Pushalkar S, Paul B, Li Q, Yang J, Vasconcelos R, Makwana S, et al. Electronic cigarette aerosol modulates the oral microbiome and increases risk of infection. iScience. 2020;23:100884.
Corriden R, Moshensky A, Bojanowski CM, Meier A, Chien J, Nelson RK, et al. E-cigarette use increases susceptibility to bacterial infection by impairment of human neutrophil chemotaxis, phagocytosis, and NET formation. Am J Phys Cell Phys. 2020;318:C205–14.
Gahring LC, Myers EJ, Rogers SW. Inhaled aerosolized nicotine suppresses the lung eosinophilic response to house dust mite allergen. Am J Phys Lung Cell Mol Phys. 2020;319:L683–92.
Hickman E, Herrera CA, Jaspers I. Common E-cigarette flavoring chemicals impair neutrophil phagocytosis and oxidative Burst. Chem Res Toxicol. 2019;32:982–5.
Ween MP, Whittall JJ, Hamon R, Reynolds PN, Hodge SJ. Phagocytosis and inflammation: exploring the effects of the components of e-cigarette vapor on macrophages. Phys Rep. 2017;5.
Szafran BN, Pinkston R, Perveen Z, Ross MK, Morgan T, Paulsen DB, et al. Electronic-cigarette vehicles and flavoring affect lung function and immune responses in a murine Model. Int J Mol Sci. 2020;21:6022.
Wang Q, Sundar I, Li D, Lucas J, Muthumalage T, McDonough S, et al. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR alpha7 receptor: role of nAChR alpha7 in ACE2 Covid-19 receptor regulation. Res Sq. 2020.
Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67:519–23.
Madison MC, Landers CT, Gu BH, Chang CY, Tung HY, You R, et al. Electronic cigarettes disrupt lung lipid homeostasis and innate immunity independent of nicotine. J Clin Invest. 2019;129:4290–304 Data from animal models in this study provide strong evidence that exposure to e-cigarettes generates lipid-laden macrophages in the lung and disrupts lipid metabolism and transport.
Itoh M, Aoshiba K, Herai Y, Nakamura H, Takemura T. Lung injury associated with electronic cigarettes inhalation diagnosed by transbronchial lung biopsy. Respirol Case Rep. 2018;6:e00282.
McCauley L, Markin C, Hosmer D. An unexpected consequence of electronic cigarette use. Chest. 2012;141:1110–3.
Mughal MS, Dalmacion DLV, Mirza HM, Kaur IP, Dela Cruz MA, Kramer VE. E-cigarette or vaping product use associated lung injury, (EVALI) - A diagnosis of exclusion. Respir Med Case Rep. 2020;31:101174.
Shields PG, Song MA, Freudenheim JL, Brasky TM, McElroy JP, Reisinger SA, et al. Lipid laden macrophages and electronic cigarettes in healthy adults. EBioMedicine. 2020;60:102982.
George J, Hussain M, Vadiveloo T, Ireland S, Hopkinson P, Struthers AD, et al. Lang CC: cardiovascular effects of switching from tobacco cigarettes to electronic cigarettes. J Am Coll Cardiol. 2019;74:3112–20.
Chaumont M, Tagliatti V, Channan EM, Colet JM, Bernard A, Morra S, et al. Short halt in vaping modifies cardiorespiratory parameters and urine metabolome: a randomized trial. Am J Phys Lung Cell Mol Phys. 2020;318:L331–44.
Funding
The work in the laboratories of R.K. and A.B. is supported in part by the National Institutes of Health and Center for Tobacco Products under Award Number HL12016. However, the content of this view is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health or the U.S. Food and Drug Administration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tobacco
Rights and permissions
About this article
Cite this article
Keith, R., Bhatnagar, A. Cardiorespiratory and Immunologic Effects of Electronic Cigarettes. Curr Addict Rep 8, 336–346 (2021). https://doi.org/10.1007/s40429-021-00359-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-021-00359-7