Abstract
Objective and design
To test the hypothesis that a continuous infusion of the vasopressin analog terlipressin is associated with less organ dysfunction as compared to intermittent bolus infusion in an ovine sepsis model.
Subjects
Twenty-seven adult female sheep.
Treatment
All sheep were subjected to a Salmonella typhosa endotoxin infusion (10 ng/kg/min). After 16 h of endotoxemia, the surviving animals (n = 24) were randomized to (1) an untreated control group, (2) a continuous terlipressin group (2 mg/24 h), or (3) a terlipressin bolus group (1 mg/6 h).
Methods
Hemodynamic variables were measured and blood was withdrawn at specific time points for the assessment of organ functions.
Results
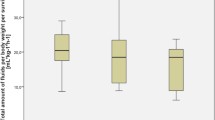
Continuous terlipressin infusion was associated with improved surrogate parameters of myocardial, renal, and hepatic function as compared with terlipressin bolus infusion. Reduced vascular hyperpermeability was evidenced by an attenuated decrease in plasma protein concentrations in sheep treated with continuous terlipressin infusion as compared to bolus injection or no treatment.
Conclusions
Continuous infusion of low-dose terlipressin preserved several surrogate parameters of organ function better than intermittent bolus injections in sheep with systemic inflammation.






Similar content being viewed by others
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Landry DW, Oliver JA. The pathogenesis of vasodilatory shock. N Engl J Med. 2001;345:588–95.
O’Brien A, Clapp L, Singer M. Terlipressin for norepinephrine-resistant septic shock. Lancet. 2002;359:1209–10.
Albanese J, Leone M, Delmas A, Martin C. Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med. 2005;33:1897–902.
Leone M, Albanese J, Delmas A, Chaabane W, Garnier F, Martin C. Terlipressin in catecholamine-resistant septic shock patients. Shock. 2004;22:314–9.
Ioannou G, Doust J, Rockey DC. Terlipressin for acute esophageal variceal hemorrhage. Cochrane Database Syst Rev 2001:CD002147.
Medel J, Boccara G, Van de Steen E, Bertrand M, Godet G, Coriat P. Terlipressin for treating intraoperative hypotension: can it unmask myocardial ischemia? Anesth Analg. 2001;93:53–5.
Morelli A, Rocco M, Conti G, Orecchioni A, De Gaetano A, Cortese G, et al. Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med. 2004;30:597–604.
Scharte M, Meyer J, Van Aken H, Bone HG. Hemodynamic effects of terlipressin (a synthetic analog of vasopressin) in healthy and endotoxemic sheep. Crit Care Med. 2001;29:1756–60.
Asfar P, Hauser B, Ivanyi Z, Ehrmann U, Kick J, Albicini M, et al. Low-dose terlipressin during long-term hyperdynamic porcine endotoxemia: effects on hepatosplanchnic perfusion, oxygen exchange, and metabolism. Crit Care Med. 2005;33:373–80.
Morelli A, Ertmer C, Lange M, Westphal M. Continuous terlipressin infusion in patients with septic shock: less may be best, and the earlier the better? Intensive Care Med. 2007;33:1669–70.
Lange M, Morelli A, Ertmer C, Koehler G, Broking K, Hucklenbruch C, et al. Continuous versus bolus infusion of terlipressin in ovine endotoxemia. Shock. 2007;28:623–9.
Westphal M, Sielenkamper AW, Van Aken H, Stubbe HD, Daudel F, Schepers R, et al. Dopexamine reverses the vasopressin-associated impairment in tissue oxygen supply but decreases systemic blood pressure in ovine endotoxemia. Anesth Analg. 2004;99:878–85.
Westphal M, Stubbe H, Sielenkamper AW, Ball C, Van Aken H, Borgulya R, et al. Effects of titrated arginine vasopressin on hemodynamic variables and oxygen transport in healthy and endotoxemic sheep. Crit Care Med. 2003;31:1502–8.
Fincke R, Hochman JS, Lowe AM, Menon V, Slater JN, Webb JG, et al. Cardiac power is the strongest hemodynamic correlate of mortality in cardiogenic shock: a report from the SHOCK trial registry. J Am Coll Cardiol. 2004;44:340–8.
Ertmer C, Bone HG, Morelli A, Van Aken H, Erren M, Lange M, et al. Methylprednisolone reverses vasopressin hyporesponsiveness in ovine endotoxemia. Shock. 2007;27:281–8.
Rehberg S, Ertmer C, Kohler G, Spiegel HU, Morelli A, Lange M, et al. Role of arginine vasopressin and terlipressin as first-line vasopressor agents in fulminant ovine septic shock. Intensive Care Med. 2009;35:1286–96.
Petersen MB. The effect of vasopressin and related compounds at V1a and V2 receptors in animal models relevant to human disease. Basic Clin Pharmacol Toxicol. 2006;99:96–103.
Bernadich C, Bandi JC, Melin P, Bosch J. Effects of F-180, a new selective vasoconstrictor peptide, compared with terlipressin and vasopressin on systemic and splanchnic hemodynamics in a rat model of portal hypertension. Hepatology. 1998;27:351–6.
Nilsson G, Lindblom P, Ohlin M, Berling R, Vernersson E. Pharmacokinetics of terlipressin after single i.v. doses to healthy volunteers. Drugs Exp Clin Res. 1990;16:307–14.
Morelli A, Ertmer C, Rehberg S, Lange M, Orecchioni A, Cecchini V, et al. Continuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot study. Crit Care. 2009;13:R130.
Ouattara A, Landi M, Le Manach Y, Lecomte P, Leguen M, Boccara G, et al. Comparative cardiac effects of terlipressin, vasopressin, and norepinephrine on an isolated perfused rabbit heart. Anesthesiology. 2005;102:85–92.
Evora PR, Pearson PJ, Rodrigues AJ, Viaro F, Schaff HV. Effect of arginine vasopressin on the canine epicardial coronary artery: experiments on V1-receptor-mediated production of nitric oxide. Arq Bras Cardiol. 2003;80:483–94.
Dunser MW, Mayr AJ, Stallinger A, Ulmer H, Ritsch N, Knotzer H, et al. Cardiac performance during vasopressin infusion in postcardiotomy shock. Intensive Care Med. 2002;28:746–51.
Dunser MW, Mayr AJ, Ulmer H, Knotzer H, Sumann G, Pajk W, et al. Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation. 2003;107:2313–9.
Duenser MW, Hasibeder WR. Dear vasopressin, where is your place in septic shock? Crit Care. 2005;9:134–5.
Luckner G, Dunser MW, Jochberger S, Mayr VD, Wenzel V, Ulmer H, et al. Arginine vasopressin in 316 patients with advanced vasodilatory shock. Crit Care Med. 2005;33:2659–66.
Farand P, Hamel M, Lauzier F, Plante GE, Lesur O. Review article: organ perfusion/permeability-related effects of norepinephrine and vasopressin in sepsis. Can J Anaesth. 2006;53:934–46.
Schuller D, Mitchell JP, Calandrino FS, Schuster DP. Fluid balance during pulmonary edema. Is fluid gain a marker or a cause of poor outcome? Chest. 1991;100:1068–75.
Laporte R, Wisniewska H, Callejas L, Russell J, Landry D, Rivière P. The selective V1a receptor agonist FE202158 reverses platelet activated factor (PAF)-induced hypotension, vascular leak, impaired tissue perfusion, and mortality in rats. Shock. 2008;Suppl 1(Abstract):P21.
Traber D. Selective V1a receptor agonists in experimental septic shock. Crit Care. 2007;11(Abstract):P51.
Bichet DG, Razi M, Lonergan M, Arthus MF, Papukna V, Kortas C, et al. Hemodynamic and coagulation responses to 1-desamino[8-d-arginine] vasopressin in patients with congenital nephrogenic diabetes insipidus. N Engl J Med. 1988;318:881–7.
Acknowledgments
The authors thank Katharina Goering, Markus Sporkmann, Mareike Bommert, and Marga Kaiser for expert technical assistance during the experiments. Terlipressin (Haemopressin®) was provided by Prof. Dr. Klaus D. Doehler (Medizinische Hochschule Hannover, Hannover, Germany). This study was supported by Curatis Pharma GmbH and MM GmbH, Hannover, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: Artur Bauhofer.
Rights and permissions
About this article
Cite this article
Lange, M., Ertmer, C., Rehberg, S. et al. Effects of two different dosing regimens of terlipressin on organ functions in ovine endotoxemia. Inflamm. Res. 60, 429–437 (2011). https://doi.org/10.1007/s00011-010-0299-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-010-0299-9