Abstract
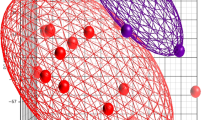
Escherichia coli and Staphylococcus epidermidis are predominant causes of neonatal sepsis, particularly affecting preterm infants. Susceptibility to infection has been attributed to “immature” innate monocyte defences, but no studies have assessed global transcriptional responses of neonatal monocytes to these pathogens. Here, we aimed to identify and characterise the neonatal monocyte transcriptional responses to E. coli and S. epidermidis and the role of common modifiers such as gestational age (GA) and exposure to chorioamnionitis (a common complication of preterm birth) to better understand early life innate immune responses. RNA-sequencing was performed on purified cord blood monocytes from very preterm (< 32 weeks GA) and term infants (37–40 weeks GA) following standardised challenge with live S. epidermidis or E. coli. The major transcriptional changes induced by either pathogen were highly conserved between infant groups and stimuli, highlighting a common extant neonatal monocyte response to infection, largely mediated by TLR/NF-κB/TREM-1 signalling. In addition, we observed an activated interferon-centred immune response specific to stimulation with E. coli in both preterm and term infants. These data provide novel insights into the functionality of neonatal monocytes at birth and highlight potential pathways that could be targeted to reduce the harmful effects of bacterial-induced inflammation in sepsis. E. coli and S. epidermidis elicit common transcriptional changes in cord monocytes. The common transcriptional response is mediated by TLR/NF-κB/TREM-1 signalling. IFN genes are differentially regulated by E. coli and S. epidermidis in monocytes. These responses are largely unaffected by GA or exposure to chorioamnionitis.
Key messages
-
E. coli and S. epidermidis elicit common transcriptional changes in cord monocytes.
-
The common transcriptional response is mediated by TLR/NF-κB/TREM-1 signalling.
-
IFN-genes are differentially regulated by E. coli and S. epidermidis in monocytes.
-
These responses are largely unaffected by GA or exposure to chorioamnionitis.




Similar content being viewed by others
References
Auffray C, Sieweke MH, Geissmann F (2009) Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol 27:669–692
de Jong E, Strunk T, Burgner D, Lavoie PM, Currie A (2017) The phenotype and function of preterm infant monocytes: implications for susceptibility to infection. Journal of Leukocyte Biology. https://doi.org/10.1189/jlb.4RU0317-111R
Strunk T, Richmond P, Prosser A, Simmer K, Levy O, Burgner D, Currie A (2011) Method of bacterial killing differentially affects the human innate immune response to Staphylococcus epidermidis. Innate Immun 17:508–516
Stoll BJ, Hansen NI, Sanchez PJ, Faix RG, Poindexter BB, Van Meurs KP, Bizzarro MJ, Goldberg RN, Frantz ID, 3rd, Hale EC et al (2011) Early onset neonatal sepsis: the burden of group B streptococcal and E. coli disease continues. Pediatrics 127: 817–826
Dong Y, Speer CP (2015) Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed 100:F257–F263
Moine P, Abraham E (2004) Immunomodulation and sepsis: impact of the pathogen. Shock 22:297–308
Oblak A, Jerala R (2015) The molecular mechanism of species-specific recognition of lipopolysaccharides by the MD-2/TLR4 receptor complex. Mol Immunol 63:134–142
Bi D, Qiao L, Bergelson I, Ek CJ, Duan L, Zhang X, Albertsson A-M, Pettengill M, Kronforst K, Ninkovic J et al (2015) Staphylococcus epidermidis bacteremia induces brain injury in neonatal mice via toll-like receptor 2-dependent and -independent pathways. J Infect Dis. https://doi.org/10.1093/infdis/jiv231
van der Poll T, Opal SM (2008) Host–pathogen interactions in sepsis. Lancet Infect Dis 8:32–43
Tang BMP, McLean AS, Dawes IW, Huang SJ, Cowley MJ, Lin RCY (2008) Gene-expression profiling of Gram-positive and Gram-negative sepsis in critically ill patients. Crit Care Med 36:1125–1128
Strunk T, Doherty D, Jacques A, Simmer K, Richmond P, Kohan R, Charles A, Burgner D (2012) Histologic chorioamnionitis is associated with reduced risk of late-onset sepsis in preterm infants. Pediatrics 129:e134–e141
Goldenberg RL, Hauth JC, Andrews WW (2000) Intrauterine infection and preterm delivery. New Engl J Med 342:1500–1507
Macaubas S, Burton T, Yabuhara H, Smallacombe K, Jenmalm H (1999) Regulation of T-helper cell responses to inhalant allergen during early childhood. Clin Exp Allergy 29:1223–1231
Kirkham LA, Corscadden KJ, Wiertsema SP, Currie AJ, Richmond PC (2013) A practical method for preparation of pneumococcal and nontypeable Haemophilus influenzae inocula that preserves viability and immunostimulatory activity. BMC Res Notes 6:522
Wisgrill L, Groschopf A, Herndl E, Sadeghi K, Spittler A, Berger A, Förster-Waldl E (2016) Reduced TNF-α response in preterm neonates is associated with impaired nonclassic monocyte function. J Leukoc Biol 100:607–612
Liao Y, Smyth GK, Shi W (2013) The Subread aligner: fast, accurate and scalable read mapping by seed-and-vote. Nucleic Acids Res 41:e108
Liao Y, Smyth GK, Shi W (2014) featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30:923–930
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, Smyth GK (2015) limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. https://doi.org/10.1093/nar/gkv007
Law CW, Chen Y, Shi W, Smyth GK (2014) voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol 15: R29
Robinson MD, Oshlack A (2010) A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol 11:R25
Wu D, Lim E, Vaillant F, Asselin-Labat M-L, Visvader JE, Smyth GK (2010) ROAST: rotation gene set tests for complex microarray experiments. Bioinformatics 26:2176–2182
de Jager W, te Velthuis H, Prakken BJ, Kuis W, Rijkers GT (2003) Simultaneous detection of 15 human cytokines in a single sample of stimulated peripheral blood mononuclear cells. Clin Diagn Lab Immunol 10:133–139
Gay NJ, Symmons MF, Gangloff M, Bryant CE (2014) Assembly and localization of Toll-like receptor signalling complexes. Nat Rev Immunol 14:546–558
Martin M, Schifferle RE, Cuesta N, Vogel SN, Katz J, Michalek SM (2003) Role of the phosphatidylinositol 3 kinase-Akt pathway in the regulation of IL-10 and IL-12 by Porphyromonas gingivalis lipopolysaccharide. J Immunol 171:717–725
Dickinson P, Smith CL, Forster T, Craigon M, Ross AJ, Khondoker MR, Ivens A, Lynn DJ, Orme J, Jackson A et al (2015) Whole blood gene expression profiling of neonates with confirmed bacterial sepsis. Genomics Data 3:41–48
Smith CL, Dickinson P, Forster T, Craigon M, Ross A, Khondoker MR, France R, Ivens A, Lynn DJ, Orme J et al (2014) Identification of a human neonatal immune-metabolic network associated with bacterial infection. Nat Commun 5:4649
Wynn JL, Guthrie SO, Wong HR, Lahni P, Ungaro R, Lopez MC, Baker HV, Moldawer LL (2015) Postnatal age is a critical determinant of the neonatal host response to sepsis. Mol Med 21:496–504
Nau GJ, Richmond JFL, Schlesinger A, Jennings EG, Lander ES, Young RA (2002) Human macrophage activation programs induced by bacterial pathogens. Proc Natl Acad Sci U S A 99:1503–1508
Garofoli F, Borghesi A, Mazzucchelli I, Tzialla C, Di Comite A, Tinelli C, Manzoni P, Stronati M (2010) Preterm newborns are provided with triggering receptor expressed on myeloid cells-1. Int J Immunopathol Pharmacol 23: 1297–1301
Arts RJW, Joosten LAB, van der Meer JWM, Netea MG (2013) TREM-1: intracellular signaling pathways and interaction with pattern recognition receptors. J Leukoc Biol 93:209–215
Bouchon A, Facchetti F, Weigand MA, Colonna M (2001) TREM-1 amplifies inflammation and is a crucial mediator of septic shock. Nature 410:1103–1107
Qian L, Weng X-W, Chen W, Sun C-H, Wu J (2014) TREM-1 as a potential therapeutic target in neonatal sepsis. Int J Clin Exp Med 7:1650–1658
Saldir M, Tunc T, Cekmez F, Cetinkaya M, Kalayci T, Fidanci K, Babacan O, Erdem G, Kocak N, Sari E (2015) Endocan and soluble triggering receptor expressed on myeloid cells-1 as novel markers for neonatal sepsis. Pediatrics & Neonatology
Arízaga-Ballesteros V, Alcorta-García MR, Lázaro-Martínez LC, Amézquita-Gómez JM, Alanís-Cajero JM, Villela L, Castorena-Torres F, Lara-Díaz VJ (2015) Can sTREM-1 predict septic shock & death in late-onset neonatal sepsis? A pilot study. Int J Infect Dis 30:27–32
Lu Y-C, Yeh W-C, Ohashi PS (2008) LPS/TLR4 signal transduction pathway. Cytokine 42:145–151
Doyle SE, Vaidya SA, O'Connell R, Dadgostar H, Dempsey PW, T-T W, Rao G, Sun R, Haberland ME, Modlin RL et al (2002) IRF3 mediates a TLR3/TLR4-specific antiviral gene program. Immunity 17:251–263
Kovarik P, Castiglia V, Ivin M, Ebner F (2016) Type I interferons in bacterial infections: a balancing act. Front Immunol 7:652
Ulas T, Pirr S, Fehlhaber B, Bickes MS, Loof TG, Vogl T, Mellinger L, Heinemann AS, Burgmann J, Schoning J et al (2017) S100-alarmin-induced innate immune programming protects newborn infants from sepsis. Nat Immunol 18:622–632
Härtel C, Osthues I, Rupp J, Haase B, Röder K, Göpel W, Herting E, Schultz C (2008) Characterisation of the host inflammatory response to Staphylococcus epidermidis in neonatal whole blood. Arch Dis Child Fetal Neonatal Ed 93:F140–F145
Sadeghi K, Berger A, Langgartner M, Prusa AR, Hayde M, Herkner K, Pollak A, Spittler A, Forster-Waldl E (2007) Immaturity of infection control in preterm and term newborns is associated with impaired toll-like receptor signaling. J Infect Dis 195:296–302
Strunk T, Prosser A, Levy O, Philbin V, Simmer K, Doherty D, Charles A, Richmond P, Burgner D, Currie A (2012) Responsiveness of human monocytes to the commensal bacterium Staphylococcus epidermidis develops late in gestation. Pediatr Res 72:10–18
Marchant EA, Kan B, Sharma AA, van Zanten A, Kollmann TR, Brant R, Lavoie PM (2015) Attenuated innate immune defenses in very premature neonates during the neonatal period. Pediatr Res. https://doi.org/10.1038/pr.2015.132
Sharma AA, Jen R, Brant R, Ladd M, Huang Q, Skoll A, Senger C, Turvey SE, Marr N, Lavoie PM (2014) Hierarchical maturation of innate immune defences in very preterm neonates. Neonatology 106:1–9
Lissner MM, Thomas BJ, Wee K, Tong A-J, Kollmann TR, Smale ST (2015) Age-related gene expression differences in monocytes from human neonates, young adults, and older adults. PLoS One 10:e0132061
Levy O, Coughlin M, Cronstein BN, Roy RM, Desai A, Wessels MR (2006) The adenosine system selectively inhibits TLR-mediated TNF-alpha production in the human newborn. J Immunol 177:1956–1966
Meijerink M, Ulluwishewa D, Anderson RC, Wells JM (2011) Cryopreservation of monocytes or differentiated immature DCs leads to an altered cytokine response to TLR agonists and microbial stimulation. J Immunol Methods 373:136–142
Funding
This project was kindly supported by funding from the National Health & Medical Research Council of Australia, the Princess Margaret Hospital Foundation, and the BrightSpark Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Electronic supplementary material
ESM 1
(PDF 737 kb)
Rights and permissions
About this article
Cite this article
de Jong, E., Hancock, D.G., Hibbert, J. et al. Identification of generic and pathogen-specific cord blood monocyte transcriptomes reveals a largely conserved response in preterm and term newborn infants. J Mol Med 96, 147–157 (2018). https://doi.org/10.1007/s00109-017-1609-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-017-1609-2