Abstract
Aims/hypothesis
The impact of early vitamin E supplementation on vascular function in diabetes remains unresolved. Therefore, we examined the effects of vitamin E on functional and structural parameters and on chemical markers that are disturbed in diabetes in mesenteric and femoral arteries.
Methods
Segments of both arteries, taken from control and 8-week-old streptozotocin diabetic Wistar rats that were treated or not with vitamin E, were mounted on wire and pressure myographs, after which endothelium-dependent and -independent vasodilation was assessed. Passive mechanical wall properties and the localisation and levels of protein kinase C (PKC)-β2 and AGE were evaluated in these vessels.
Results
Vitamin E supplementation was associated with improved endothelium-dependent and -independent vasodilatation in mesenteric arteries from diabetic rats. Impaired endothelium-dependent vasodilatation in diabetic mesenteric vessels was associated with PKC-β2 up-regulation and this was prevented by vitamin E supplementation. Increased AGE accumulation and plasma isoprostane levels in diabetic rats were not changed by vitamin E. In the femoral artery, vitamin E supplementation had no effect on endothelium-dependent or -independent vasodilatation, but did prevent the wall stiffening associated with diabetes.
Conclusions/interpretation
Early vitamin E supplementation has a beneficial effect on diabetes-induced endothelial dysfunction in resistance arteries. This benefit may arise from a direct effect on smooth muscle function, as a result of inhibition of the PKC-β2 isoform by vitamin E.
Similar content being viewed by others
Introduction
Abnormal vascular reactivity is a hallmark of the complications of diabetes [1, 2]. Increased oxidative stress, as a result of hyperglycaemia, impairs endothelium-dependent relaxation [3] and leads to vascular wall thickening via vascular smooth muscle hypertrophy and hyperplasia [4], and to stiffening through the formation of AGE [5]. Vitamin E decreases protein kinase C (PKC) activation [6], a key mediator of the vasoconstrictor response to oxidative stress [7]. However, the benefits of vitamin E supplementation (VitE) in diabetes are variable, with improved endothelium-dependent vasodilatation seen in conduit arteries in streptozotocin (STZ)-induced diabetic rats [8]. Low dose VitE did not reverse vasodilator dysfunction in mesenteric arteries from STZ-diabetic rats [9]. In one small study, VitE improved flow-mediated dilatation in the brachial artery of subjects with Type 1 diabetes, while it had no effect on arterial compliance [10].
Although one randomised placebo-controlled clinical trial has demonstrated that VitE reduces the incidence of cardiovascular events in patients with established cardiovascular disease [11], two recent prospective clinical trials found no benefit from VitE [12, 13]. However, there are no published reports of the impact of VitE on the primary prevention of cardiovascular disease in humans. This may be more important since oxidative stress-induced injury in diabetes may not, once established, be reversible by later antioxidant therapy [1].
To test this hypothesis, we used the well-characterised rat STZ model to examine the ability of a higher dose of VitE early in the course of diabetes to prevent or reduce endothelial vasodilator dysfunction and changes in mechanical wall properties in arteries. The effects of VitE were studied in two muscular arteries, the mesenteric and femoral arteries. We examined possible mechanisms of action for vitamin E, including direct effects on the level of reactive oxygen species, effects on arterial wall PKC-β2, and effects on AGE accumulation.
Materials and methods
Animals
Diabetes was induced in 8-week-old male Wistar rats (Central Animal Services, Monash University, Melbourne, Australia) by injection of STZ (60 mg/kg) into the tail vein as described previously [14]. Diabetic rats and control rats received standard chow (containing 50 mg VitE per kg) or chow supplemented with (+)-α-tocopherol (VitE) at 1 g/kg of rat body weight per day. Since diabetes is associated with hyperphagia, diabetic and control rats were caged separately and extra standard chow was provided subsequently to the diabetic animals. After 8 weeks the rats were anaesthetised, weighed and killed by decapitation. The experiments in this study comply with the guidelines of the National Health and Medical Research Council of Australia: “Code of Practice for the Care and Use of Animals for Scientific Purposes”.
Blood was collected and plasma glucose concentration was measured immediately. Plasma and whole blood was frozen (−80 °C) for later measurements of glycohaemoglobin (GHb), lipids, plasma VitE and 8-isoprostane concentrations. Femoral arteries and the mesenteric bed were freed of adipose and loose connective tissue. Lengths of 10 to 15 mm of each bed were retained for immediate study while the remaining tissue was weighed and snap-frozen in liquid nitrogen for localisation and semi-quantification of arterial wall PKC-β2.
Functional studies
Segments of 1° femoral artery and 2° mesenteric arcade were mounted on a myograph for measurement of isometric tension [14]. Segments were continuously superfused with isoglycaemic physiological saline solution (PSS) at 35 °C at 4 ml/min. The solution contained (mmol/l): NaCl 120, KCl 5, NaHCO3 25, KH2PO4 1, MgSO4 1.2, CaCl2 2.5, glucose 11, and was gassed with O2 95%, CO2 5%. Endothelial function was tested using acetylcholine (ACh) in segments pre-contracted with phenylephrine (10−6–10−5 mol/l). Concentration-relaxation curves were obtained in control PSS, in Nω-nitro-l-arginine methyl ester (l-NAME, 10−4 mol/l), and l-NAME and indomethacin (10−6 mol/l) as described [14]. Relaxations persisting in the presence of both blockers represent the contribution of endothelium-derived hyperpolarising factor (EDHF) [14]. Endothelium-independent relaxation was tested using sodium nitroprusside (SNP). All drugs were purchased from Sigma, St Louis, Mo., USA.
Passive mechanical wall properties
Leak-free segments of each artery were mounted on a pressure myograph, the proximal end tied to a glass cannula, the distal end tied off and set pressure maintained via a servo-control system (Living Systems, Burlington, Vt., USA). The myograph was mounted on an inverted microscope fitted with a video camera and the image was projected on to a monitor screen, from which length, wall thickness and outside diameter of the segment were measured (×300 magnification). Segments were superfused at 10 ml/min with zero-Ca2+ PSS containing EGTA (1 mmol/l). Intraluminal pressure (P) was increased in increments (10–120 mm Hg, expressed in Pa), and external diameter (OD), length (L) and wall thickness (h) were measured (in µm) at each pressure. The following parameters were derived: internal diameter (ID µm) = OD−2h; wall stress (kPa) = P(ID)/(2h); wall strain = ID−(IDextrapolated to 0 mm Hg pressure)/(IDextrapolated to 0 mm Hg pressure). The rate constant of an exponential function fitted to the stress–strain relationship was determined using Prism software (GraphPad, San Diego, Calif., USA).
AGE determinations
Vascular AGE content was determined by immunohistochemistry as described [15]. In brief, sections were incubated with a polyclonal AGE antibody that recognises the non-fluorescent AGE, carboxymethyllysine [16]. Vascular AGE staining was then characterised using semi-quantitative image analysis methods. The AGE-associated fluorescence of collagen extracted was also estimated in vascular tissue samples following pepsin digestion (400 mg/ml) and acid hydrolysis [17]. Results were normalised for the hydroxyproline content of the supernatant determined by standard methods [18]. Incomplete digestion of AGE-modified tissue proteins results in the production of AGE-peptides with a low molecular weight. These accumulate in the serum and accurately reflect the level of tissue AGE-modification in experimental diabetes [19]. Plasma AGE-peptides present in plasma samples were assayed using a flow injection assay system with on-line spectrofluorometric detection [19].
Protein kinase C-β2 immunohistochemistry
A modification of the ABC immunoglobulin enzyme bridge technique [20] was used on formalin-fixed paraffin sections of vessels. Endogenous peroxidase activity was eliminated by incubating sections in 0.3% hydrogen peroxide for 20 min. Sections were then incubated with normal goat serum for 20 min and with PKC-β2 primary antibody (Santa Cruz Biotechnologies, Santa Cruz, Calif., USA). The latter was done overnight at 4 °C. Tissue sections were consecutively stained with biotinylated IgG and avidin-biotin horseradish peroxidase complex (Vectastain ABC ELITE kit, Vector Laboratories, Burlingame, Calif., USA). Peroxidase activity was demonstrated using 3,3-diaminobenzidine in 0.03% hydrogen peroxide. Sections were counterstained in Harris’ haematoxylin and mounted in dePex (BDH, Merck, Poole, UK).
Blood glucose and GHb levels
Blood glucose (mmol/l) was measured by reflectance as described [14]. GHb levels were measured by an automated HPLC assay based on affinity chromatography (CLC330 HbA1c analyser; Primus, Kansas City, Kan., USA).
Lipid measurements
Total cholesterol, triglycerides and HDL-cholesterol were measured by commercial enzymatic assays using a DADE Behring Dimension RxL Chemistry Analyser (Dade Behring Diagnostics, Sydney, Australia). CVs were 1.9% at 3.4 mmol/l, 1.3% at 7 mmol/l and 4.4% at 0.65 mmol/l.
Plasma vitamin E concentrations
Plasma vitamin E (α and γ tocopherol) was measured using reverse phase HPLC with an ultraviolet absorption detector [21].
Plasma isoprostane
Free plasma 8-isoprostane was analysed by an Enzymatic Immuno Assay (Cayman Chemical, Ann Arbor, Mich., USA). The performance characteristics as assessed by the manufacturer for intra- and inter-assay CVs were less than 10%.
Data analysis
Relaxations (tension) were expressed as per cent of the contraction evoked by phenylephrine. Sigmoid curves were fitted to concentration–relaxation curves using the least-squares method (Prism software) [14]. Maximal relaxation (Vmax), the concentration of drug that produced 50% of Vmax (EC50) and pD2 values (−log EC50) were compared between treatment groups. Values of n quoted indicate the number of rats in the group. Student’s t test or ANOVA were used for testing, and differences were accepted as statistically significant when p was less than 0.05.
Results
Animal weights and circulating biochemical parameters
Body weight
Body weights of control (250±3 g, n=33) and diabetic rats (256±4 g, n=29) were similar (p=0.3) at the time of STZ injection. Weights at 8 weeks following injection were significantly lower in diabetic animals and were not affected by VitE (Table 1).
Blood glucose and GHb levels
At 8 weeks, diabetic rats were hyperglycaemic and GHb levels were elevated. VitE did not influence these variables (Table 1).
Plasma vitamin E levels
Total plasma vitamin E levels were similar in all rats fed standard chow (control 24±2 [n=14] versus diabetic rats 25±2 µmol/l [n=12]), with most being α-tocopherol. Levels of α-tocopherol were more than three-fold greater in rats receiving VitE (control 66±6 [n=19] vs diabetic rats 196±40 µmol/l [n=17], p<0.01).
Lipids
Total cholesterol, HDL and triglyceride levels were higher in diabetic than in control rats. VitE was associated with a decrease in all of these parameters in controls, but not with lower plasma cholesterol levels in diabetic rats (Table 1).
Isoprostanes
Plasma total isoprostane concentrations were about two-fold higher in diabetic than in control rats (p<0.01). VitE was associated with a significant reduction in isoprostane in control but not in diabetic rats (Table 1).
Functional responses
Endothelium-dependent vasodilatation in mesenteric arteries
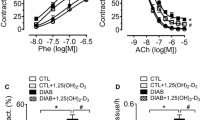
In rats fed standard chow, higher concentrations of ACh were required to achieve relaxation in mesenteric arteries of diabetic compared with control rats (pD2 7.10±0.08, n=9, vs 7.70±0.04, n=10, p<0.0001). VitE had no effect on ACh-induced relaxation in arteries from controls but significantly improved the sensitivity to ACh (pD2 7.42±0.04, n=12, p=0.0005) in vessels of diabetic rats (Fig. 1a, b). The pD2 value in the presence of l-NAME and indomethacin, which represents EDHF, was significantly reduced in diabetic rats (pD2 6.03±0.21, n=9, vs 6.67±0.07, n=10, p=0.007) and was not affected by VitE in vessels of either control or diabetic rats (Fig. 1a, b).
Acetylcholine reduced the tension evoked by phenylephrine in segments of mesenteric (a, b) and femoral (c, d) arteries (squares). Subsequently, nitric oxide and prostanoid production were blocked with l-NAME and indomethacin respectively (circles). Rats fed with standard chow, open symbols; rats fed with vitamin E supplement, filled symbols
Endothelium-dependent vasodilatation in femoral arteries
There was no difference in endothelium-dependent relaxation in femoral arteries of diabetic or control rats fed standard chow or VitE (Fig. 1c, d). Endothelium-dependent relaxation was abolished in all femoral arteries by l-NAME (Fig. 1c, d).
Endothelium-independent vasodilatation
In rats fed standard chow, there was no difference between diabetic and control rats with regard to relaxation of mesenteric and femoral arteries in response to SNP (Table 2). VitE significantly improved the sensitivity to SNP in mesenteric arteries of diabetic and control rats, but did not affect SNP-induced relaxation in femoral arteries (Table 2). The improvement in sensitivity to endothelium-independent SNP and endothelium-derived nitric oxide (NO) in mesenteric arteries from diabetic rats was equivalent at approximately two-fold in both cases.
Passive mechanical wall properties
Mesenteric arteries
The maximum ID reached was significantly greater in vessels from diabetic than in those from control rats fed standard chow. Wall thickness at 90–120 mm Hg remained the same (diabetic, 27±2 µm, n=3 vs control rats, 26±2 µm, n=4). Wall stress was increased in diabetic arteries (Fig. 2), reflecting the difference in internal diameter. The rate constant of the stress–strain relationship was similar in vessels from control (4.85±0.77, n=4) and diabetic rats (5.11±0.62, n=3) (Fig. 3).
Internal diameter and wall stress of arterial segments. Segments were superfused in the absence of calcium and pressure was increased incrementally. Internal diameter was measured and wall stress calculated in mesenteric (a, b) and femoral (c, d) arteries from control (filled symbols) and diabetic rats (open symbols) fed either standard chow (controls n=4; diabetic n=3) or standard chow with added vitamin E (n=10 controls; n=8 diabetic). Squares, rats on standard chow; circles, rats on added vitamin E. *, p<0.05 control vs diabetic rats; #, p<0.05 added vitamin E vs standard chow, for entire curve
In mesenteric arteries (a), there was no difference in the stress–strain relationship in diabetes or following vitamin E supplementation (VitE). Conversely in femoral arteries (b), stiffness was increased in diabetes and this was prevented by VitE. Filled squares: control rats fed standard chow; open squares: diabetic rats fed standard chow. Filled circles: control rats fed VitE; open circles: diabetic rats fed VitE. * p<0.05 control vs diabetic rats. # p<0.05 VitE vs standard chow for the entire curve. Numbers of animals: as Figure 2
VitE resulted in a striking thinning of the walls of mesenteric arteries from both control (21±1 µm, n=10) and diabetic rats (21±1 µm, n=8), and prevented the increase in internal diameter in diabetic rats (Fig. 2). Wall stress was significantly increased by VitE in tissues from control and diabetic rats (Fig. 2), reflecting the reduced wall thickness. The rate constant of the stress–strain relationship in arteries from control (5.03±0.65, n=10) and diabetic rats (5.40±0.77, n=8) was unchanged following VitE (Fig. 3).
Femoral arteries
Internal diameter, wall thickness at 90–120 mm Hg (diabetic, 52±1 µm, n=3 vs control rats, 58±6 µm, n=4) and wall stress were similar in femoral arteries from diabetic and control rats (Fig. 2). VitE significantly reduced wall thickness (diabetic, 39±2 µm, n=8 vs control rats, 44±3 µm, n=10) but wall stress was not affected (Fig. 2). The stress–strain relationship was markedly shifted to the left in femoral arteries from diabetic vs control rats, with a significantly elevated rate constant (diabetic 6.27±0.76 vs control rats 4.11±0.32, p=0.03), and this was prevented by VitE (diabetic, 4.15±0.65, n=8 vs control rats, 4.57±0.77, n=10) (Fig. 3).
Protein kinase C-β2 localisation and levels
Levels of the PKC isoform PKC-β2, as assessed by immunohistochemical staining, were greater in mesenteric arteries from diabetic (n=8) (Fig. 4c, e) than in those from control rats fed standard chow (n=7; p=0.03) (Fig. 4a, e). VitE did not affect PKC-β2 levels in mesenteric arteries from control rats (n=7; p=0.8) (Fig. 4b, e), but in arteries from diabetic rats the levels were reduced to values that did not differ from controls (n=8; p=0.2) (Fig. 4d, e).
Protein kinase C (PKC)-β2 was significantly greater in mesenteric arteries of diabetic rats fed normal chow (c) than in control rats on standard chow (a) and this was normalised by vitamin E supplementation (d). Combined data are shown in (e). n=7 in (a) and (b); n=8 in (c) and (d); * significantly different from control rats. C+VitE, control rats on vitamin E supplement; D+VitE, diabetic rats on vitamin E supplement
Levels of PKC-β2 were also higher in femoral arteries of diabetic (3.8±0.8%, n=8) vs control rats (1.3±0.4%, n=8, p=0.02) fed standard chow, but were unchanged by VitE (diabetic, 2.6±0.7%, n=10, p=0.3 vs control rats, 0.7±0.1%, n=9, p=0.2).
In both arteries, immunohistochemical staining appeared to be greatest in the smooth muscle cells of the medial layer.
AGE localisation and levels
Vascular staining for AGE was significantly increased in vessels of diabetic versus control rats, both in mesenteric arteries (diabetic, 4.0±0.3%, n=5 vs control rats, 2.2±0.6%, n=5, p<0.01) and femoral arteries (diabetic, 3.6±0.4%, n=6 vs control rats, 0.9±0.2%, n=7, p<0.01). Mesenteric artery AGE-fluorescence and plasma AGE peptide were also increased in diabetic rats to a similar extent (Fig. 5). VitE did not significantly modify vascular AGE-staining or AGE-fluorescence in either rat group.
AGE and pentosidine-like fluorescence in mesenteric arteries and plasma AGE peptide were all increased in diabetic rats fed normal chow and were not influenced by vitamin E supplementation (VitE). * p<0.05 control vs diabetic rats; n=6 (a, b); (c) n=13 control, n=19 C+VitE (control + VitE), n=12 diabetic, n=16 D+VitE (diabetic + VitE)
Discussion
This study demonstrates that early VitE improves endothelium-dependent relaxation in small resistance mesenteric arteries of diabetic rats (Table 3). This is consistent with observations in patients with diabetes [10]. Some previous studies of VitE in STZ-induced diabetes have failed to show any significant effect on endothelium-dependent relaxation in the mesenteric arteries, although in those studies a five- to ten-fold lower dose of VitE was used [9]. Indeed, supplementation with a higher dose of VitE improved endothelium-dependent relaxation in the aorta [8] and prevented the decline in blood flow to hindlimb nerves after 2 months of STZ-induced diabetes [22], similar to our present findings in small resistance arteries.
The effect of early VitE on vasorelaxation in diabetes appears to reflect an improvement in the response to NO, as the component of endothelium-dependent relaxation attributed to EDHF was unaltered. Significantly, VitE enhanced endothelium-independent relaxation in response to SNP in mesenteric arteries, indicating a direct effect of VitE on NO availability and/or vasodilator mechanisms in the smooth muscle (Table 3). VitE improved the component of endothelium-dependent vasodilation attributable to NO in mesenteric arteries, although this component did not appear to be impaired by diabetes. In contrast, VitE had little effect on the response attributable to EDHF, the principal component of vasodilation impaired in diabetes.
Improvements in vasodilator function in small mesenteric arteries in this study were independent of changes in plasma isoprostanes. Important physiological effects of VitE involve its incorporation into vascular tissue [23], including inhibition of leucocyte adhesion to endothelial cells [24], reduced smooth muscle proliferation [25] and protection against oxidant-mediated cytotoxicity [26]. It is possible that the benefit derived from VitE on endothelial function may be concentration-dependent and occur regardless of its effect on oxidant stress as measured by isoprostane levels. Nevertheless, isoprostane levels cannot be considered universal markers of oxidative stress, in particular in the vasculature where other pathways may predominate, such as NADPH oxidase [27].
Diabetes is associated with markedly increased expression of PKC-β, especially in the smooth muscle layer (Fig. 4). Early VitE prevented the diabetes-associated rise in PKC-β levels in mesenteric arteries of diabetic rats (Table 3). PKC-β has significant actions in endothelial and smooth muscle cells of blood vessels [1, 28]. PKC may contribute to abnormal vascular reactivity via increased production of superoxide radicals [20], and in endothelial cells it may impair NO production by reducing NO synthase protein levels [29]. In vascular smooth muscle, enhanced PKC-β2 activity is associated with hypertrophy and hyperplasia [4]. Enhanced plasma membrane phospholipase D activity [4] and an increase in diacylglycerol levels [30] are thought to underlie the enhanced PKC-β2 activity in hyperglycaemia. The inhibition of PKC-β2 activation by VitE has been documented in diabetes [4, 6, 31]. VitE abrogates the increase in hyperglycaemia-induced PKC-β2, diacylglycerol, phospholipase D and changes in cell number and size. The mechanisms by which VitE inhibits PKC activation are unclear. The fact that other antioxidants, even β-tocopherol, do not inhibit PKC suggests that these mechanisms are not related to the anti-oxidant effect of vitamin E [32]. The inhibitory effect of α-tocopherol (VitE) on PKC activation is concordant with its effect on phosphorylation of the myristolated, alanine-rich C kinase substrate protein, a substrate of PKC [25], and with the fact that it also increased protein phosphatase type 2A activity, which results in PKC-dephosphorylation [32]. These observations suggest that a ligand/receptor type of mechanism is the basis of the action of VitE on PKC. There is also evidence that VitE may inhibit PKC translocation to the cell membrane [25].
VitE had no effect on endothelium-dependent relaxation in femoral arteries from diabetic rats (Table 3). We have previously reported that this artery (at ~300 µm diameter) is resistant to the effects of diabetes [14]. In contrast to the mesenteric arteries, the significantly elevated PKC-β2 activation in femoral arteries from diabetic rats was not affected by VitE (Table 3). This suggests that PKC-β2 activation does not have deleterious effects on relaxation pathways in this artery and may explain its resistance to the effects of diabetes. It may be that metabolic cross-talk between the endothelium and smooth muscle is required for the expression of dysfunction involving PKC-β. This notion arises from our previous observations showing that, while endothelial and smooth muscle cells are well connected via myo-endothelial gap junctions in mesenteric arteries, the two cell types are not connected in femoral arteries [33]. This difference may provide a clue to resolving the different susceptibilities between arterial beds to dysfunction in diabetes, a suggestion that requires further study.
There are no previous studies of the effect of VitE on passive mechanical wall properties of resistance vessels. Previous studies in patients with Type 1 diabetes failed to demonstrate any significant effect of VitE on brachial arterial compliance measured in vivo [10, 34], despite improved endothelium-dependent vasodilatation. Increased intestinal perfusion in the setting of diabetes-induced hyperphagia may contribute to an increase in maximum internal diameter in mesenteric arteries (Table 3). The fact that this increase in diameter was not associated with a change in the stress–strain relationship suggests remodelling in the absence of a change in mechanical properties. The relatively small number of control tissues studied means that these conclusions are made with caution.
The similarity between vascular flow responses of pair-fed diabetic rats and those of diabetic rats with free access to food suggests that diabetes, and not hyperphagia, may determine the changes mentioned above [35]. In contrast, femoral arteries appeared to be restricted in their ability to increase in diameter and were significantly stiffer in diabetes (Table 3), with the suggestion of a change in wall composition. While VitE markedly reduced wall thickness in both arteries, this is probably achieved by re-arrangement of the components and/or structure of the wall, rather than by an altered wall composition in mesenteric arteries. Again, the number of control tissues here was relatively small. VitE prevented the diabetes-associated stiffening in femoral arteries. This is likely to be independent of PKC-β since the content of this kinase in femoral arteries was unchanged by VitE. While AGE are important causes of altered mechanical wall properties in diabetes [5, 36], VitE did not influence the AGE content of arteries from diabetic rats.
A number of studies, primarily in Type 2 diabetes, have assessed the role of VitE and related compounds on endothelial function and oxidative stress, with varying results [37, 38]. Nevertheless, recent large trials [12, 13] have reported no benefit from VitE in the prevention of cardiovascular disease in individuals with and without diabetes. It should be appreciated that the data presented here suggest that the potential benefit of VitE in diabetes occurs early, prior to the onset of irreversible structural and functional changes in resistance vessels. As a result, VitE may be better used in the primary prevention of vascular disease, rather than the secondary prevention of vascular events in patients with established vascular disease.
Abbreviations
- ACh:
-
acetylcholine
- EDHF:
-
endothelium-derived hyperpolarising factor
- GHb:
-
glycohaemoglobin
- h:
-
wall thickness
- ID:
-
internal diameter
- L:
-
length
- l-NAME:
-
Nω-nitro-l-arginine methyl ester
- NO:
-
nitric oxide
- OD:
-
outside diameter
- P:
-
intraluminal pressure
- PKC:
-
protein kinase C
- PSS:
-
physiological saline solution
- SNP:
-
sodium nitroprusside
- STZ:
-
streptozotocin
- VitE:
-
vitamin E supplementation
- Vmax :
-
maximal relaxation
References
Feener EP, King GL (1997) Vascular dysfunction in diabetes mellitus. Lancet 350:SI9–SI13
De Vriese AS, Verbeuren TJ, Van de Voorde J, Lameire NH, Vanhoutte PM (2000) Endothelial dysfunction in diabetes. Br J Pharmacol 130:963–974
Andrews HE, Brukdorfer KR, Dunn RC, Jacobs M (1987) Low-density lipoproteins inhibit endothelium-dependent relaxation in rabbit aorta. Nature 327:237–239
Yasunari K, Kohno M, Kano H, Yokokawa K, Minami M, Yoshikawa J (1999) Antioxidants improve impaired insulin-mediated glucose uptake and prevent migration and proliferation of cultured rabbit coronary smooth muscle cells induced by high glucose. Circulation 99:1370–1378
Wolffenbuttel BHR, Boulanger CM, Crijns FRL et al. (1998) Breakers of advanced glycation end-products restore large artery properties in experimental diabetes. Proc Natl Acad Sci USA 95:4630–4634
Kunisaki M, Fumio U, Nawata H, King GL (1996) Vitamin E normalizes diacylglycerol—protein kinase C activation induced by hyperglycaemia in rat vascular tissues. Diabetes 45 [Suppl 3]:S117–S119
Sugiyama S, Kugiyama K, Ohgushi M, Fujimoto K, Yasue H (1994) Lysophosphatidylcholine in oxidized low-density lipoprotein increases endothelial susceptibility to polymorphonuclear leukocyte-induced endothelial dysfunction in porcine coronary arteries: role of protein kinase C. Circ Res 74:565–575
Keegan A, Walbank H, Cotter MA, Cameron NE (1995) Chronic vitamin E treatment prevents defective endothelium-dependent relaxation in diabetic rat aorta. Diabetologia 38:1475–1478
Palmer AM, Thomas CR, Gopaul N et al. (1998) Dietary antioxidant supplementation reduces lipid peroxidation but impairs vascular function in small mesenteric arteries of the streptozotocin-diabetic rat. Diabetologia 41:148–156
Skyrme-Jones RAP, O’Brien RC, Berry KL, Meredith IT (2000) Vitamin E supplementation improves endothelial function in type 1 diabetes mellitus: a randomized, placebo-controlled study. J Am Coll Cardiol 36:94–102
Stephens NG, Parsons A, Schofield PM, Kelly F, Cheeseman K, Mitchinson MJ (1996) Randomized controlled trial of vitamin E in patients with coronary disease: Cambridge Heart Antioxidant Study (CHAOS). Lancet 347:781–786
Yusuf S for the Heart Outcomes Prevention Evaluation Study Investigators (2000) Vitamin E supplementation and cardiovascular events in high risk patients. New Engl J Med 342:154–160
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:23–33
Wigg SJ, Tare M, Tonta MA, O’Brien RC, Meredith IT, Parkington HC (2001) Comparison of effects of diabetes mellitus on an EDHF-dependent and an EDHF-independent artery. Am J Physiol 281:H232–H240
Soulis T, Cooper ME, Sastra S et al. (1997) Relative contributions of advanced glycation and nitric oxide synthase inhibition to aminoguanidine-mediated renoprotection in diabetic rats. Diabetologia 40:1141–1151
Van der Pijl JW, Daha MR, van den Born J et al. (1998) Extracellular matrix in human diabetic nephropathy: reduced expression of heparan sulphate in skin basement membrane. Diabetologia 41:791–798
Candido R, Forbes JM, Thomas MC et al. (2003) A breaker of advanced glycation end products attenuates diabetes-induced myocardial structural changes. Circ Res 92:785–792
Stegemann H, Stalder K (1967) Determination of hydroxyproline. Clin Chim Acta 18:267–273
Wrobel K, Wrobel K, Garay-Sevilla ME, Nava LE, Malacara JM (1997) Novel analytical approach to monitoring advanced glycosylation end products in human serum with on-line spectrophotometric and spectrofluorometric detection in a flow system. Clin Chem 43:1563–1569
Ohara Y, Peterson TE, Zheng B, Kuo JF, Harrison DG (1994) Lysophosphatidylcholine increases vascular superoxide anion production via protein kinase C activation. Arterioscler Thromb 14:1007–1013
Cuesta Sanz D, Castro Santa-Cruz M (1986) Simultaneous measurement of retinol and alpha-tocopherol in human serum by high-performance liquid chromotography with ultraviolet detection. J Chromatogr 380:140–144
Cotter MA, Love A, Watt MJ, Cameron NE, Dines KC (1995) Effects of natural free radical scavengers on peripheral nerve and neurovascular function in diabetic rats. Diabetologia 38:1285–1294
Keaney JF, Gaziano JM, Xu A et al. (1994) Low-dose α-tocopherol improves and high-dose α-tocopherol worsens endothelial vasodilator function in cholesterol-fed rabbits. J Clin Invest 93:844–851
Faruqi R, de la Motta C, DiCorleto P (1994) Alpha tocopherol inhibits agonist-induced monocytic cell adhesion to cultured human endothelial cells. J Clin Invest 94:592–600
Boscoboinik D, Szewczyk A, Azzi A (1991) Alpha-tocopherol (vitamin E) regulates vascular smooth muscle cell proliferation and protein kinase C activity. Arch Biochem Biophys 286:264–269
Hennig B, Enoch C, Chow CK (1987) Protection by vitamin E against endothelial cell injury by linoleic acid hydroperoxides. Nutr Res 7:1253–1260
Chen X, Touyz RM, Park JB, Schiffrin EL (2001) Antioxidant effects of vitamins C and E are associated with altered activation of vascular NADPH oxidase and superoxide dismutase in stroke-prone SHR. Hypertension 38:606–611
Beckman JA, Goldfine AB, Gordon MB, Garrett LA, Creager MA (2002) Inhibition of protein kinase Cβ prevents impaired endothelium-dependent vasodilation caused by hyperglycemia in humans. Circ Res 90:107–111
Ohara Y, Sayegh HS, Yamin JJ, Harrison DG (1995) Regulation of endothelial constitutive nitric oxide synthase by protein kinase C. Hypertension 25:415–420
Muniyappa R, Srinivas PR, Ram JL, Walsh MF, Sowers JR (1998) Calcium and protein kinase C mediate high-glucose-induced inhibition of inducible nitric oxide synthase in vascular smooth muscle cells. Hypertension 31:289–295
Ganz MB, Seftel A (2000) Glucose-induced changes in protein kinase C and nitric oxide are prevented by vitamin E. Am J Physiol 278:E146–E152
Azzi A, Breyer I, Feher M et al. (2000) Specific cellular responses to α-tocopherol. J Nutr 130:1649–1652
Sandow SL, Tare M, Coleman HA, Hill CE, Parkington HC (2002) Involvement of myoendothelial gap junctions in the actions of endothelium-derived hyperpolarizing factor. Circ Res 90:1108–1113
Berry KL, Skyrme-Jones RAP, Cameron JD, O’Brien RC, Meredith IT (1999) Systemic arterial compliance is reduced in young patients with IDDM. Am J Physiol 276:H1839–H1845
Jeremy JY, Thompson CS, Mikhailidis DP (1992) Differential changes of prostanoid synthesis by the gastrointestinal tract, mesenteric vasculature and hepatic portal vein of diabetic rats: comparison between pair and ad libitum feeding. In Vivo 6:635–639
Huijberts MSP, Wolffenbuttel BHR, Struijker Boudier HAJ et al. (1993) Aminoguanidine treatment increases elasticity and decreases fluid filtration of large arteries from diabetic rats. J Clin Invest 92:1407–1411
Chowienczyk PJ, Brett SE, Gopaul NK et al. (2000) Oral treatment with an antioxidant (raxofelast) reduces oxidative stress and improves endothelial function in men with type II diabetes. Diabetologia 43:974–977
Gazis A, White DJ, Page SR, Cockcroft JR (1999) Effect of oral vitamin E (α-tocopherol) supplementation on vascular endothelial function in Type 2 diabetes mellitus. Diabetic Med 16:304–311
Acknowledgements
This study was supported by the National Heart Foundation of Australia and the National Health and Medical Research Council of Australia (M. C. Thomas, postgraduate biomedical scholarship). It was also supported by the Juvenile Diabetes Research Foundation (J. Forbes, postdoctoral fellowship).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wigg, S.J., Tare, M., Forbes, J. et al. Early vitamin E supplementation attenuates diabetes-associated vascular dysfunction and the rise in protein kinase C-β in mesenteric artery and ameliorates wall stiffness in femoral artery of Wistar rats. Diabetologia 47, 1038–1046 (2004). https://doi.org/10.1007/s00125-004-1411-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1411-x