Abstract
Aims/hypothesis
Glucose homeostasis is determined by an interplay between insulin secretion and insulin action. In Type 1 diabetes, autoimmune destruction of pancreatic beta cells leads to impaired insulin secretion. However, the contribution of impaired insulin action (insulin resistance) to the development of Type 1 diabetes has received little attention. We investigated whether insulin resistance was a risk factor for progression to Type 1 diabetes.
Methods
Islet-antibody-positive first-degree relatives of Type 1 diabetes probands were followed for 4.0 years (median). Insulin secretion was measured as first-phase insulin response (FPIR) to intravenous glucose. Insulin resistance was estimated by homeostasis model assessment of insulin resistance (HOMA-R). We compared subjects who progressed (n=43) and subjects who did not progress (n=61) to diabetes, including 21 pairs matched for age, sex, islet antibodies and FPIR.
Results
Progressors had higher insulin resistance relative to insulin secretion at baseline (median HOMA-R : FPIR 0.033 vs 0.013, p<0.0001). According to Cox proportional hazards analysis, islet antibody number, FPIR, fasting plasma glucose, fasting serum insulin, HOMA-R and log(HOMA-R : FPIR) were each predictive of progression to diabetes. However, log(HOMA-R : FPIR) (hazard ratio 2.57 per doubling, p<0.001) was the only metabolic variable independently associated with progression. In the matched comparison, progressors had higher fasting glucose, fasting insulin, HOMA-R and HOMA-R : FPIR, both at baseline and during the follow-up pre-clinical phase.
Conclusions/interpretation
Relatives positive for islet antibodies who progress most rapidly to diabetes have a subtle disturbance of insulin–glucose homeostasis years before the onset of symptoms, distinguished by greater insulin resistance for their level of insulin secretion. Taking steps to reduce this insulin resistance could therefore delay the development of Type 1 diabetes.
Similar content being viewed by others
Introduction
Type 1 diabetes is an autoimmune disease in which destruction of pancreatic islet beta cells leads to insulin deficiency. In first-degree relatives of Type 1 diabetes probands, the presence of circulating autoantibodies to the islet antigens insulin, GAD or tyrosine phosphatase-like insulinoma antigen 2 (IA2) denotes underlying islet autoimmune pathology and an increased risk of diabetes. Risk has been shown to be related to the number of antigen specificities, the level of islet antibodies, specific HLA alleles, and the degree of impaired insulin secretion [1, 2, 3, 4], but prediction remains inexact. Improved prediction would facilitate the counselling of at-risk individuals and the selection of subjects for intervention trials to prevent clinical disease.
Glucose disposal and prevailing glycaemia are determined not only by insulin secretion but also by insulin action [5]. In contrast to in Type 2 diabetes, impaired insulin action or insulin resistance has not been considered to play a major role in the pathogenesis of Type 1 diabetes. Nevertheless, insulin resistance has been documented in established Type 1 diabetes [6] and physiological states of insulin resistance such as puberty [7] and pregnancy [8] are associated with the onset of Type 1 diabetes [9, 10]. First-degree relatives positive for islet antibodies who are at increased risk of Type 1 diabetes have varying degrees of insulin resistance [11], but whether insulin resistance influences progression to clinical disease has not been documented. Interestingly, in the non-obese diabetic mouse model of Type 1 diabetes, hyperinsulinaemia, a marker of insulin resistance, antedates clinical disease [12], and the incidence of diabetes has been reduced by treatment with rosiglitazone, a thiazolidinedione drug that decreases insulin resistance [13].
If insulin resistance is found to play a role in the progression to human Type 1 diabetes, this would have important implications not only for risk prediction but also for intervention to reduce insulin resistance and delay the onset of diabetes. Therefore, in a cohort of first-degree Type 1 diabetes relatives positive for islet antibodies, we prospectively examined measures of insulin resistance and insulin secretion to determine whether insulin resistance is, in itself, a risk factor for progression to clinical disease.
Subjects and methods
Subjects
A total of 3773 relatives of Type 1 diabetes probands were screened for islet antibodies in the population-based Melbourne Pre-Diabetes Family Study [14] (Fig. 1). Of these, 104 relatives (3%) confirmed as positive for one or more islet antibodies were followed annually, testing for islet antibodies and using an IVGTT to measure first-phase insulin response (FPIR). All participants provided written informed consent to participate in the study, and all procedures were approved by institutional ethics committees.
Over a median follow-up period of 4.0 years, 43 subjects progressed (progressors) and 61 did not progress (non-progressors) to diabetes (Fig. 1, Table 1). Diagnosis of diabetes was based on symptoms (polydipsia, polyuria, weight loss) and plasma glucose levels, as laid out in the American Diabetes Association criteria [15].
Islet antibodies
Insulin autoantibodies (IAA) were measured by precipitation of 125I-(A14)-labelled human insulin [16]. Antibodies to GAD (GAD Ab) and IA2 (IA2 Ab) were measured by precipitation of 35S-methionine-labelled, in vitro transcribed and translated GAD65 or IA2 [17]. These assays have shown optimal sensitivity and specificity in International Workshops and Standardization Programs conducted by the Immunology of Diabetes Society (e.g. in [2]). The specificity and sensitivity of our assays in the 2003 Diabetes Antibody Standardization Program were: IAA (95%, 26%), GAD Ab (97%, 80%) and IA2 Ab (100%, 68%). Thresholds for positivity established as the 97.5% percentile of unselected healthy school children were: IAA, 100 U/ml; GAD Ab, 5 U/ml; and IA2 Ab, 3 U/ml. Until 1995, all individuals were screened for islet cell antibodies (ICA) by standard indirect immunofluorescence, as well as for GAD Ab, IA2 Ab and IAA. The ICA assay was discontinued in 1995. Thus, all relatives positive for GAD Ab, IA2 Ab or IAA, and also for ICA prior to 1995, were included in the analysis.
Insulin secretory function and insulin resistance
The IVGTT was performed according to the ICARUS protocol [18] by one of two research nurses. Subjects were instructed to maintain their normal dietary intake and to include at least 150 g of carbohydrate per day for at least 3 days before the test. They fasted for 10 to 12 hours overnight and abstained from smoking, coffee consumption and excessive physical activity for 24 hours before the test. Intravenous glucose (0.5 g/kg body weight as a 25% solution, up to a maximum of 35 g) was injected over 3 minutes into an antecubital vein. Blood samples were collected from a cannula in situ 5 minutes before and immediately prior to injection of glucose, as well as 1, 2, 3, 5, 7 and 10 minutes after injection. Serum insulin was measured with a commercial radioimmunoassay kit (Pharmacia, Uppsala, Sweden); the inter-assay coefficient of variation was 3% at levels of 15 and 50 mU/l, and 5% at 138 mU/l. FPIR, a validated measure of beta cell function, was calculated as the sum of the serum insulin concentrations at 1 and 3 minutes after i.v. glucose [18]. Samples from each subject were all analysed in the same assay. In our study, the mean inter-assay coefficient of variation for FPIR in healthy young adults was 11.4% [19].
Insulin resistance was estimated by the homeostasis model assessment of insulin resistance (HOMA-R) [20] as fasting insulin (mU/l) × fasting glucose (mmol/l)/22.5. In a large adult population, the median HOMA-R was 2.1 [21]. HOMA-R was calculated from the mean of the fasting insulin and glucose values at −5 and 0 minutes both at baseline (from the IVGTT at recruitment) and serially over the duration of follow-up (median number of IVGTTs = 4).
Statistical analysis
Differences in age, body weight percentile, number of islet antibody specificities, islet antibody levels, follow-up time and metabolic parameters between the whole cohort of progressors and non-progressors were analysed by the non-parametric Mann–Whitney test. Differences between the frequency of HLA types were analysed by the chi square test for trend. The association between HOMA-R and FPIR was analysed by least squares regression. Potential predictive variables for progression to diabetes were analysed by a Cox proportional hazards model using baseline data. Age band (0–5, 6–10, 11–20, 21–30, 31–40, >40) at baseline and islet antibody number (at baseline, as a continuous variable) were included in all analyses to avoid confounding, although only the number of antibodies was associated with significantly increased hazard. Sex was also added to the model at various stages but appeared unrelated to progression. The ‘standard’ model was obtained by adding FPIR (discretised by quartiles). Additional potential predictive variables were then added: fasting plasma glucose, fasting serum insulin, HOMA-R, log(fasting insulin : FPIR) and log(HOMA-R : FPIR). These additional variables were evaluated, either as continuous covariates or when discretised by quartile, using the likelihood ratio (LR) test. Untransformed fasting insulin : FPIR and HOMA-R : FPIR were not included because they were heavily skewed and their inclusion in the model gave unstable estimates. The ratios were therefore log transformed and base-2 logs were used for ease of interpretation. The ability of log(fasting insulin : FPIR) or log(HOMA-R : FPIR) to supplant other metabolic variables was then tested by including them in a revised model with age band and number of islet antibodies. The LR test was then used to determine whether any of the other variables significantly improved the model.
In addition to the multivariate analysis, a clinical approach was adopted in which progressors were individually matched with non-progressors as closely as possible for age, sex, number of islet antibodies and FPIR. Most progressors with very low FPIR could not be matched, because FPIR in non-progressors was, of course, normal. Consequently, a comparison was possible between 21 progressors and non-progressors. Differences between matched progressors and non-progressors were analysed by a paired t test. The rate of change of HOMA-R values over time was calculated as the slope of the linear regression line. For follow-up measures of HOMA-R and other metabolic parameters, the mean of serial values in each subject was calculated, followed by a calculation of the median of these for the whole group.
Results
Progressors were comparable in age, sex, body weight percentile and HLA DR allele frequency to non-progressors, but were distinguished by a higher number and higher levels of islet antibodies (Table 1). Non-progressors were obviously followed for longer, the median time to diabetes in progressors being 2.7 years. Although baseline HOMA-R was correlated with baseline FPIR (r=0.53, p<0.0001), the progressors had greater insulin resistance for their level of insulin secretion (Fig. 2). Thus, the ratio (median [interquartile range]) of fasting insulin : FPIR at baseline was significantly higher in progressors than in non-progressors (0.146 [0.091–0.236] vs 0.061 [0.050–0.074], p<0.0001), as was the ratio of HOMA-R : FPIR (0.033 [0.012–0.057] vs 0.013 [0.011–0.017], p<0.0001). Similarly, during follow-up, fasting insulin : FPIR and HOMA-R : FPIR were greater in progressors (Table 1).
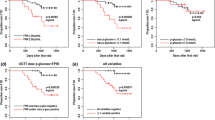
Kaplan–Meier survival curves according to HOMA-R : FPIR quartiles demonstrated that higher baseline HOMA-R : FPIR ratios were associated with an increased risk of progression to diabetes (Fig. 3). Cox proportional hazards analysis was performed to determine whether the fasting insulin : FPIR and HOMA-R : FPIR ratios were independent risk factors for progression to diabetes. The analysis was initially based on a standard model incorporating islet antibody number, FPIR and age. Islet antibody number and FPIR were confirmed to be independently associated with progression to diabetes. Age, included to avoid confounding, was not consistently associated with progression. Metabolic variables, namely fasting glucose, fasting insulin, HOMA-R, log(fasting insulin : FPIR) and log(HOMA-R : FPIR), added separately to the standard model, were each associated with progression (Table 2). Given that log(HOMA-R : FPIR) is derived from HOMA-R and FPIR, it was substituted for FPIR in the standard model to determine whether it supplanted the other metabolic variables. In the revised model (Table 2), islet antibody number (hazard ratio 3.16 per antibody, p<0.001) and log(HOMA-R : FPIR) (hazard ratio 2.57 per doubling, p<0.001) were independently associated with progression. When the other metabolic variables, fasting glucose, fasting insulin, HOMA-R and FPIR were added separately to the revised model they were no longer independently associated with progression. Thus, log(HOMA-R : FPIR) supplanted the other metabolic variables for association with progression to diabetes (Table 2). Log(fasting insulin : FPIR) in place of log(HOMA-R : FPIR) in the revised model also supplanted fasting glucose (hazard ratio 1.74, p=0.098), fasting insulin (hazard ratio 1.00, p=0.90), HOMA-R (hazard ratio 1.04, p=0.74) and FPIR (hazard ratio 2.84 per doubling, p<0.001) (p=0.17).
In the matched pair comparison, progressors and non-progressors were similar for age, sex ratio, body weight percentile, frequency of HLA DR3,4 alleles and number of islet antibody specificities, levels of islet antibodies and baseline FPIR (Table 3). Despite being within the population reference range, fasting plasma glucose and fasting serum insulin were higher at baseline in matched progressors. In addition, progressors had greater insulin resistance relative to insulin secretion at baseline and during follow-up (Table 3).
Three other findings require comment. Firstly, HOMA-R declined with time to diabetes in progressors but remained unchanged in non-progressors, the rate of change (mean of the slopes of individual regression lines) being −0.40 compared with 0.05 (p=0.010). Because the decrease in HOMA-R over time was lower than that in FPIR, the ratio of HOMA-R : FPIR increased over time in progressors (Table 3). Secondly, 22 of the 104 relatives were positive for ICA only, but none progressed to diabetes. Their HOMA-R, FPIR and HOMA-R : FPIR were not significantly different from those of the other non-progressors, but the subjects were significantly older (mean age 35.1±2.9 vs 17.5±1.8 years, p<0.0001). Thirdly, although IAA could theoretically interfere with the measurement of insulin, we found there to be no relationship between IAA and HOMA-R either in the whole cohort (r=0.07) or separately in progressors (r=0.23) and non-progressors (r=−0.34).
Discussion
This is the first study to investigate longitudinally both insulin secretion and insulin resistance in the progression to clinical Type 1 diabetes. Progression to diabetes in first-degree relatives positive for islet antibodies was associated with an increase in insulin resistance relative to insulin secretion, independently of known risk markers. While fasting insulin has been used in the past as an index of insulin resistance, HOMA-R has been shown to correlate better with results from hyperinsulinaemic–euglycaemic clamp studies [20]. HOMA-R has been widely applied as an index of insulin resistance in people with NGT [20, 22, 23] and in those with IGT or diabetes [24, 25, 26], and has also been used to document insulin resistance in longitudinal studies [27]. This is an important consideration, as invasive techniques for direct measurement of insulin resistance would not be feasible or ethically acceptable in longitudinal studies involving children.
Relatives positive for islet antibodies who progressed most rapidly to clinical diabetes had evidence of disturbed insulin–glucose homeostasis years before diagnosis. Their increased fasting plasma glucose and serum insulin levels compared with the non-progressors, although still within the normal ranges, account for their higher baseline HOMA-R values. Further evidence for this subtle disturbance was the increase in HOMA-R relative to FPIR, which increased over time to diabetes, indicating progressive dysregulation of the relationship between insulin action and insulin secretion. The significance of these findings lies in the fact that the most rapid progressors can be identified early, even when metabolic parameters such as fasting glucose, fasting insulin and FPIR are still within the normal ranges. It is important to note, however, that a single estimation of HOMA-R could be misleading, as HOMA-R decreases as individuals approach clinical disease, most probably because fasting insulin levels decline. Nevertheless, as we demonstrate here, HOMA-R is best interpreted in the context of insulin secretion; the HOMA-R : FPIR ratio was increased in progressors not only at baseline but also during follow-up and the progression to diabetes. Furthermore, log(HOMA-R : FPIR) was superior to HOMA-R or FPIR alone for estimating risk. The use of an alternative ratio, log(fasting insulin : FPIR), yielded similar results.
Insulin resistance in individuals with islet autoimmunity could have a genetic–constitutional basis, or could be secondary to the autoimmune disease process itself. The commonest association of insulin resistance is with obesity, and children who develop diabetes have been shown to have an increased BMI in the first year of life [28]. In our cohort, body weight percentile was not significantly different between progressors and non-progressors. However, this measure may not accurately reflect visceral adiposity and insulin resistance [29], and subtle differences in body composition between the progressors and the non-progressors cannot be excluded. Alternatively, insulin resistance may reflect a more aggressive form of autoimmune disease mediated, for example, by immuno-inflammatory factors that also mediate beta cell destruction. Such factors include TNF-α and IL-6 [30], which have been implicated in insulin resistance [31, 32], and, conceivably, autoantibodies to the insulin receptor, which have been reported to be associated with IAA [33]. Further studies are required to determine whether autoimmune mechanisms in Type 1 diabetes contribute to insulin resistance. Because plasma glucose is determined by the interplay of insulin secretion and insulin action [5], one would expect insulin resistance to lead to an earlier appearance of hyperglycaemia when beta cell function is compromised by autoimmune disease. Furthermore, an increase in plasma glucose secondary to insulin resistance could augment islet inflammation and beta cell death. Glucose has been shown to induce the pro-inflammatory cytokine IL-1β in islets [34], to up-regulate expression of the Fas death receptor [35] and autoantigens [36, 37] in beta cells, and to induce beta cell apoptosis [38].
The finding that insulin resistance in individuals positive for islet antibodies is a risk factor for progression to clinical diabetes has several important implications. Firstly, it should improve risk prediction, currently based on FPIR and islet antibody parameters, and should therefore assist in counselling individuals and families. Secondly, it could allow at-risk individuals to be stratified into more uniform risk groups for recruitment into intervention–prevention trials, reducing the number of participants and thereby increasing the efficiency and decreasing the cost of such trials. Finally, reduction of insulin resistance, with insulin-sensitising drugs, diet or exercise, could delay the onset of clinical Type 1 diabetes.
Abbreviations
- Ab:
-
antibody
- FPIR:
-
first-phase insulin response
- HOMA-R:
-
homeostasis model assessment of insulin resistance
- IA2:
-
tyrosine phosphatase-like insulinoma antigen 2
- IAA:
-
insulin autoantibodies
- ICA:
-
islet cell antibodies
- LR:
-
likelihood ratio
References
Bingley PJ, Bonifacio E, Williams AJ, Genovese S, Bottazzo GF, Gale EA (1997) Prediction of IDDM in the general population: strategies based on combinations of autoantibody markers. Diabetes 46:1701–1710
Verge CF, Stenger D, Bonifacio E et al. (1998) Combined use of autoantibodies (IA-2 autoantibody, GAD autoantibody, insulin autoantibody, cytoplasmic islet cell antibodies) in type 1 diabetes: Combinatorial Islet Autoantibody Workshop. Diabetes 47:1857–1866
Harrison LC (2001) Risk assessment, prediction and prevention of type 1 diabetes. Pediatr Diabetes 2:71–82
Bingley PJ, Bonifacio E, Ziegler AG, Schatz DA, Atkinson MA, Eisenbarth GS (2001) Proposed guidelines on screening for risk of type 1 diabetes. Diabetes Care 24:398
Kahn SE, Prigeon RL, McCulloch DK et al. (1993) Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Yki-Jarvinen H, Koivisto VA (1986) Natural course of insulin resistance in type I diabetes. N Engl J Med 315:224–230
Smith CP, Archibald HR, Thomas JM et al. (1988) Basal and stimulated insulin levels rise with advancing puberty. Clin Endocrinol (Oxf) 28:7–14
Catalano PM, Tyzbir ED, Roman NM, Amini SB, Sims EA (1991) Longitudinal changes in insulin release and insulin resistance in nonobese pregnant women. Am J Obstet Gynecol 165:1667–1672
Greenbaum CJ (2002) Insulin resistance in type 1 diabetes. Diabetes Metab Res Rev 18:192–200
Buschard K, Buch I, Mølsted-Pedersen L, Hougaard P, Kühl C (1987) Increased incidence of true type 1 diabetes acquired during pregnancy. BMJ 294:275–279
McCulloch DK, Klaff LJ, Kahn SE et al. (1990) Nonprogression of subclinical beta-cell dysfunction among first-degree relatives of IDDM patients. 5-yr follow-up of the Seattle Family Study. Diabetes 39:549–556
Amrani A, Durant S, Throsby M, Coulaud J, Dardenne M, Homo-Delarche F (1998) Glucose homeostasis in the nonobese diabetic mouse at the prediabetic stage. Endocrinology 139:1115–1124
Beales PE, Pozzilli P (2002) Thiazolidinediones for the prevention of diabetes in the non-obese diabetic (NOD) mouse: implications for human type 1 diabetes. Diabetes Metab Res Rev 18:114–117
Colman PG, McNair P, Margetts H et al. (1998) The Melbourne Pre-Diabetes Study: prediction of type 1 diabetes mellitus using antibody and metabolic testing. Med J Aust 169:81–84
American Diabetes Association (2002) Clinical Practice Recommendations 2002. Diabetes Care 25 [Suppl 1]:S1–S147
Vardi P, Dib SA, Tuttleman M et al. (1987) Competitive insulin autoantibody assay. Prospective evaluation of subjects at high risk for development of type I diabetes mellitus. Diabetes 36:1286–1291
Petersen JS, Hejnaes KR, Moody A et al. (1994) Detection of GAD65 antibodies in diabetes and other autoimmune diseases using a simple radioligand assay. Diabetes 43:459–467
Bingley PJ, Colman P, Eisenbarth GS et al. (1992) Standardization of IVGTT to predict IDDM. Diabetes Care 15:1313–1316
McNair PD, Colman PG, Alford FP, Harrison LC (1995) Reproducibility of the first-phase insulin response to intravenous glucose is not improved by retrograde cannulation and arterialization or the use of a lower glucose dose. Diabetes Care 18:1168–1173
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Haffner SM, Miettinen H, Stern MP (1997) The homeostasis model in the San Antonio Heart Study. Diabetes Care 20:1087–1092
Radziuk J (2000) Insulin sensitivity and its measurement: structural commonalities among the methods. J Clin Endocrinol Metab 85:4426–4433
Bonora E, Targher G, Alberiche M et al. (2000) Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 23:57–63
Hermans MP, Levy JC, Morris RJ, Turner RC (1999) Comparison of insulin sensitivity tests across a range of glucose tolerance from normal to diabetes. Diabetologia 42:678–687
Katsuki A, Sumida Y, Gabazza EC et al. (2001) Homeostasis model assessment is a reliable indicator of insulin resistance during follow-up of patients with type 2 diabetes. Diabetes Care 24:362–365
Emoto M, Nishizawa Y, Maekawa K et al. (1999) Homeostasis model assessment as a clinical index of insulin resistance in type 2 diabetic patients treated with sulfonylureas. Diabetes Care 22:818–822
Wallace TM, Matthews DR (2002) The assessment of insulin resistance in man. Diabet Med 19:527–534
Bruining GJ (2000) Association between infant growth before onset of juvenile type-1 diabetes and autoantibodies to IA-2. Netherlands Kolibrie study group of childhood diabetes. Lancet 356:655–656
McCarthy HD, Ellis SM, Cole TJ (2003) Central overweight and obesity in British youth aged 11–16 years: cross sectional surveys of waist circumference. BMJ 326:624
Campbell IL, Harrison LC (1990) A new view of the beta cell as an antigen-presenting cell and immunogenic target. J Autoimmun 3:53–62
Katsuki A, Sumida Y, Murashima S et al. (1998) Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 83:859–862
Hak AE, Pols HA, Stehouwer CD et al. (2001) Markers of inflammation and cellular adhesion molecules in relation to insulin resistance in nondiabetic elderly: the Rotterdam study. J Clin Endocrinol Metab 86:4398–4405
Harrison LC, Flier JS, Roth J, Karlsson FA, Kahn CR (1979) Immunoprecipitation of the insulin receptor: a sensitive assay for receptor antibodies and a specific technique for receptor purification. J Clin Endocrinol Metab 48:59–65
Maedler K, Sergeev P, Ris F et al. (2002) Glucose-induced beta cell production of IL-1beta contributes to glucotoxicity in human pancreatic islets. J Clin Invest 110:851–860
Maedler K, Spinas GA, Lehmann R et al. (2001) Glucose induces beta-cell apoptosis via upregulation of the Fas receptor in human islets. Diabetes 50:1683–1690
Aaen K, Rygaard J, Josefsen K et al. (1990) Dependence of antigen expression on functional state of beta-cells. Diabetes 39:697–701
Bjork E, Kampe O, Karlsson FA et al. (1992) Glucose regulation of the autoantigen GAD65 in human pancreatic islets. J Clin Endocrinol Metab 75:1574–1576
Donath MY, Gross DJ, Cerasi E, Kaiser N (1999) Hyperglycemia-induced beta-cell apoptosis in pancreatic islets of Psammomys obesus during development of diabetes. Diabetes 48:738–744
Acknowledgements
This study was supported by Vic Health and by a Juvenile Diabetes Research Foundation (JDRF) Center Program Grant (to L.C. Harrison). S. Fourlanos is a Postgraduate Scholar of the National Health and Medical Research Council of Australia. P. Narendran was a JDRF Research Fellow at the time of the study. We thank Cheryl Steele and Peter McNair (registered nurses) for clinical support and for performing the IVGTTs, Shane Gellert for islet antibody assays, Gordon Smythe for advice on statistical analysis and Catherine O’Shea for secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00125-004-1621-2
Rights and permissions
About this article
Cite this article
Fourlanos, S., Narendran, P., Byrnes, G.B. et al. Insulin resistance is a risk factor for progression to Type 1 diabetes. Diabetologia 47, 1661–1667 (2004). https://doi.org/10.1007/s00125-004-1507-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1507-3