Abstract
Aims/hypothesis
We sought to characterise the effect of the age-related decline of GFR on hyperfiltration in type 2 diabetes and to identify clinical characteristics associated with hyperfiltration.
Materials and methods
GFR was measured in 662 type 2 diabetic patients by plasma disappearance of 99 m-technetium-diethylene-triamine-penta-acetic acid. The prevalence of hyperfiltration was calculated using both an age-unadjusted GFR threshold of >130 ml min−1 1.73 m−2 and an age-adjusted threshold incorporating a decline of 1 ml min−1 year−1 after the age of 40. The hyperfiltering patients were compared with type 2 diabetic subjects who had a GFR between 90 and 130 ml min−1 1.73 m−2 and were matched for age, sex and disease duration to allow for identification of modifiable factors associated with hyperfiltration.
Results
The prevalence of hyperfiltration was 7.4% when age-unadjusted and 16.6% when age-adjusted definitions were used. The age-unadjusted vs -adjusted prevalence rates for hyperfiltration were 50 vs 50%, 12.9 vs 23.4% and 0.3 vs 9.0% for patients aged <40 years, 40 to 65 years and >65 years, respectively. Both the age-unadjusted and -adjusted hyperfiltration groups had lower mean diastolic blood pressure and lower serum creatinine levels than the control groups. Although the age-unadjusted hyperfiltration group had larger kidneys compared to the control group, this difference was no longer significant when the age-adjusted definition was used. There were no differences in HbA1c, mean arterial pressure, antihypertensive use, insulin therapy, dyslipidaemia, frequency of macro- or microvascular complications, BMI, urinary sodium, urea and albumin excretion between the groups.
Conclusions/interpretation
Hyperfiltration was still more common among younger patients with type 2 diabetes even after adjusting for the expected age-related decline in GFR. Hyperfiltration was associated with a lower mean diastolic blood pressure independent of age.
Similar content being viewed by others
Introduction
Diabetic nephropathy is the single most common cause of end-stage renal failure worldwide. The cumulative incidence of clinical nephropathy in type 2 diabetes varies from around 5 to 10% in Caucasians to 20 to 40% among certain other ethnic groups [1, 2]. Glomerular hyperfiltration is a well characterised phenomenon in the early phase of renal involvement in type 1 diabetes and has been regarded as a putative risk factor in the pathogenesis of clinical nephropathy [3]. Hyperfiltration is thought to be a maladaptive response to glomerular haemodynamic disturbances that eventually lead to development of diabetic nephropathy [4, 5]. At a glomerular level, it is thought that hyperfiltration is caused by increases in the glomerular capillary plasma flow rate and mean glomerular capillary hydraulic pressure, which in turn are due to changes in systemic arterial pressure and/or changes in efferent and afferent arteriolar resistances [5]. In type 1 diabetes, hyperfiltration carries a 53% risk of developing overt nephropathy compared with 5% in normofiltering subjects over a 17-year period [6]. In comparison, information on the prevalence and pathogenic significance of hyperfiltration in type 2 diabetes is inconclusive and controversial, due to (1) difficulties in defining hyperfiltration in this population, (2) the co-existence of non-diabetic renal disease, (3) the diversity of patient characteristics, and (4) the insidious onset of the disease [2, 7–12]. Hyperfiltration in type 2 diabetes has been associated with a greater rate of decline in GFR than in normofiltering and non-diabetic control subjects over a 6-year period [13], but this finding is not universal [2].
The definition of hyperfiltration is further clouded by the ‘physiological’ decline in renal function, which is known to occur during the process of ageing [14]. Previous studies have not incorporated this age-related decline of GFR in to the definition of hyperfiltration, which may potentially ‘mask’ this phenomenon in older subjects. The primary aim of this study was to determine the prevalence of hyperfiltration using both age-unadjusted and -adjusted definitions in a clinic-based cohort of type 2 diabetic patients. We also wished to identify modifiable clinical and biochemical parameters associated with hyperfiltration, compared with a control group of non-hyperfiltering type 2 diabetic subjects who were matched for age, sex and disease duration.
Subjects, materials and methods
Definition of hyperfiltration and normofiltration
In this study, an age-unadjusted threshold for hyperfiltration was defined arbitrarily as a Bröchner–Mortensen (B–M) corrected GFR of >130 ml min−1 1.73 m−2 based on the definitions used in previous studies [2, 6, 7, 9, 11, 12, 15]. To account for the age-related decline in GFR in our diabetic population, we used an age-adjusted definition for hyperfiltration of GFR >130 ml min−1 1.73 m−2 that was reduced progressively by 1 ml min−1 year−1 after the age of 40. (i.e. age-adjusted GFR=measured GFR+[age−40]*1) This is in accordance with the age-related decline of GFR in the normal US population as documented in the Third National Health and Nutrition Examination Survey [16]. The B–M equation corrects for the overestimation of GFR when using an isotopic plasma disappearance method with a single bolus of tracer instead of a steady-state infusion GFR [17, 18]. The threshold for hyperfiltration used in our study is roughly equivalent to 165 ml min−1 1.73 m−2 without B–M correction and therefore represents a much stricter criterion than values used in some other studies [13]. Age-unadjusted control subjects (normo-filterers) were defined as subjects with a GFR between 90 and 130 ml min−1 1.73 m−2. The age-related decline of GFR of 1 ml min−1 year−1 (after the age of 40) was applied to define the age-adjusted control subjects. Subjects with a GFR <60 ml min−1 1.73 m−2 with or without age-adjustment were excluded (Fig. 1). The terms normofilterers and controls are used interchangeably.
Distribution of GFR values in 662 patients with type 2 diabetes, categorised into age-adjusted hyperfilterers (filled circles), age-adjusted normofilterers (open circles), and other groups (x, low GFR; filled squares, unclassified). Age-unadjusted GFR subgroups were defined as follows: (1) hyperfiltration: GFR >130 ml min−1 1.73 m−2; (2) normofiltration: GFR 90–130 ml min−1 1.73 m−2; (3) low GFR, <60 ml min−1 1.73 m−2. Age-adjusted GFR subgroups: (1) hyperfiltration <40 years: GFR >130 ml min−1 1.73 m−2; (2) normofiltration <40 years: GFR 90–130 ml min−1 1.73 m−2; (3) hyperfiltration >40 years: GFR >130 ml min−1 1.73 m−2 +[(age−40)*1]; (4) normofiltration >40 years: GFR 90–130 ml min−1 1.73 m−2 +[(age−40)*1]; (5) low GFR: <60 ml min−1 1.73 m−2 irrespective of age adjustment
Patients
A search of our database located a total of 662 type 2 diabetic patients without a history of non-diabetic renal disease attending the Austin Health Diabetes Clinics and in whom at least one isotopic GFR measurement had been performed between 1994 and 2004. The Austin Health Diabetes Clinics serve a population of 600,000 in north-eastern Melbourne. The majority of referrals to the clinic are from general practitioners and approximately 20% of the patients are referred from other specialty units within the medical centre. The diagnosis of diabetes was based on WHO criteria [19].
Informed consent was obtained from the study participants for unrestricted use of their clinical data for research purposes. The study was approved by the institutional Ethics Committee.
Measurements
GFR measurements are routinely performed on patients as part of a surveillance programme for diabetes complications at least every 2 to 3years. Patients are not specifically selected for GFR estimation on clinical grounds. The objective of the clinic is to measure the GFR in all regular attenders, irrespective of their disease duration, renal function or albuminuria status. The GFR was measured between 09:00 and 12:30 hours by plasma disappearance of a bolus of 99 Tc-diethylene-triamine-penta-acetic acid followed by three venous blood samples taken over 210 min [17]. Patients were hydrated with 500 ml of water, taken orally, prior to testing. Extravasation of tracer at the injection site was checked routinely. Patients were ambulatory throughout the study. Values were adjusted to body surface area and also modified using the B−M correction [18]. When a subject had more than one GFR measurement in the hyperfiltration range, the most recent value was included in the study. The GFR measurements in our study were carried out in a non-fasting state, but we have included 24-h urine urea excretion performed over the 24 h preceding the GFR scan as a marker of protein intake [20].
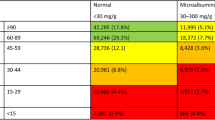
Biochemical and clinical data were matched as closely as possible to the date of the GFR estimation. At each routine follow-up clinic visit, blood samples were obtained in a fasting state for standard indices including plasma creatinine, urea, albumin, glucose, lipid profile and HbA1c. Urinary creatinine, urea and albumin were obtained from a fresh 24-h urine collection. Results not obtained in an outpatient clinic setting (e.g. hospitalised patients or in an emergency setting) were excluded. All urine samples were examined by microscopy and culture for urinary tract infection or haematuria. Albumin concentrations were determined by radioimmunoassay or immunoturbidimetry (Dade-Behring Turbitimer, Marburg, Germany). Patients were classified into normo-, micro- or macro-albuminuria according to their albumin excretion rate (AER) values (AER <20, 20–200 and >200 μg/min, respectively), based on at least two of three consecutive 24-h urine samples collected within 2 years from the date of GFR measurement. Urine and plasma electrolytes were measured on a Hitachi 911 automatic analyser (Roche Diagnostics, Mannheim, Germany). HbA1c was measured by automated high-performance liquid chromatography (Diamat; Biorad, Richmond, CA, USA). Fasting lipids were measured by enzymatic colorimetry. Dyslipidaemia was diagnosed if total cholesterol >5.5 or LDL >4.5 mmol/l or triglycerides >2.0 mmol/l or if treated with lipid-lowering medication.
Blood pressure was measured according to Korotkoff sounds after 5 min in a recumbent position. Diagnosis of retinopathy was based on a formal ophthalmological review and classified as background or proliferative disease. Macrovascular disease was diagnosed by history and examination of peripheral arterial status (claudication, absent foot pulses, ischaemic changes), coronary artery disease (history of angina, myocardial infarction, ischaemic cardiomyopathy, positive stress test or ECG abnormalities) and cerebrovascular disease (history of stroke/transient ischaemic attacks). Kidney size was obtained from ultrasound scans.
Statistical methods
Data for continuous variables are means±SEM except where shown as median (inter-quartile range). Data for categorical variables are proportions. Where given, p values refer to unpaired t-tests for continuous variables and to chi square analysis for categorical variables. We considered p values of <0.05 to be significant.
Results
The GFR percentiles for each decade of age in the 662 patients with type 2 diabetes are shown in Fig. 2. The median GFR was 127 and 65 ml min−1 1.73 m−2 in patients aged <40 and 70–80 years, respectively, demonstrating a linear rate of decline in GFR of 1.8 ml min−1 year−1 after the age of 40 in this population. The distribution of GFR values for the total population and threshold values for the definitions of age-adjusted and -unadjusted hyperfiltration and normofiltration are depicted in Fig. 1.
Age-stratified distribution of GFR in 662 patients with type 2 diabetes. Shaded area: National Kidney Foundation definition of mild renal impairment [21]
Based on the age-unadjusted definitions, there were 49 hyperfilterers (mean age 48±1 years, 63% male, disease duration 6.7±0.6 years, mean GFR 140+1 ml min−1 1.73 m−2) and 215 normofiltering control subjects (mean age 59±1years, 56% male, disease duration 9.7±1 years, mean GFR 1061 ml min−1 1.73 m−2 ) in the total study population. When age-related GFR decline was incorporated into the definition, the total number of hyperfilterers rose to 110 (mean age 57±1 years, 63% male, disease duration 9.0±1years, mean GFR 126+2 ml min−1 1.73 m−2) and the number of control subjects to 346 (mean age 64+1 years, 54% male, disease duration 11.9.0±0.4 years, mean GFR 88±1 ml min−1 1.73 m−2) (Fig. 3). It should be noted that although a GFR range of 60 to 90 ml min−1 1.73 m−2 is classified as early renal impairment by the National Kidney Foundation guidelines [21], 192 subjects from our study population with a GFR in this range were re-classified as ‘normofiltering’ (control group) for the purposes of this study.
The overall age-unadjusted and -adjusted prevalence of hyperfiltration was 7.4 and 16.6%, respectively. After adjustment for age, the prevalence increased from 12.9 to 23.4% in patients aged 40–65 years, and from 0.3 to 9.0% in patients aged 65+ years (Fig. 3).
When comparing the age-adjusted and -unadjusted hyperfiltration groups with their respective matched control groups (Table 1), it is evident that the subjects were well matched with respect to age, sex and disease duration. Both hyperfiltration groups had significantly lower mean diastolic blood pressure, but mean systolic blood pressure, mean arterial pressure and the proportion of patients on antihypertensive therapy including ACE inhibitors and angiotensin receptor blockers were not significantly different. The age-unadjusted hyperfiltration group had larger kidneys and lower plasma creatinine levels compared to the respective control groups. However, when the definition of hyperfiltration was adjusted for age, the difference in kidney size was no longer significant. Glycaemic control, mean BMI, 24-h urinary urea excretion rates, estimated dietary protein intake, median AER, the proportion of patients with dyslipidaemia and on insulin therapy, as well as the frequency of macrovascular and microvascular complications were similar across the groups. Two of the age-unadjusted hyperfiltering subjects had AERs in the macroalbuminuric range, which is unusual as macroalbuminuria is usually associated with impaired renal function. Both these subjects had a history of hypertension and macrovascular disease.
Discussion
The overall prevalence of hyperfiltration in our study was 7.4%, which rose to 16.6% following adjustment for age-related GFR decline. Most authors define hyperfiltration as a GFR greater than two standard deviations above the mean, both for a diabetic and for a non-diabetic population; the reported thresholds for hyperfiltration (using age-unadjusted definitions) range between 125 and 140 ml min−1 1.73 m−2. The reported prevalence of hyperfiltration varies widely from 6 to 75%, with high rates documented in new-onset diabetes and in certain ethnic populations [2, 7–12, 22]. The high rates of hyperfiltration in new-onset diabetes may be explained, at least partly, by the acute metabolic effect of hyperglycaemia, as previous studies have demonstrated an association between hyperglycaemia and hyperfiltration as well as nephromegaly [23, 24]. Improved glycaemic control has been shown to reduce GFR and kidney size [25, 26] Long-term hyperglycaemia has also been correlated with elevated GFR in type 1 diabetes [27]. In contrast, we did not find any difference in glycaemic control between the age-unadjusted and -adjusted hyperfiltration and control groups.
Approximately 80% of our study population was of Caucasian ethnicity. Previous reports suggest that the prevalence of hyperfiltration is higher in certain ethnic groups, such as Pima Indians, African–Americans, Asians and Polynesians, than in Caucasians [1, 2, 8, 10, 28, 29]. However, in these ethnic groups diabetes occurs at an earlier age, and the prevalence rates may be affected by the age-unadjusted definition of hyperfiltration as discussed below. The timing of diagnosis of diabetes in relation to the true onset also affects the prevalence of hyperfiltration, as the hyperfiltration phase may be missed if diagnosis is delayed.
Other reasons for the wide variation of reported prevalence rates of hyperfiltration include a lack of precision in the methods used to estimate GFR. For example, the Cockroft–Gault equation [30] overestimates GFR values, while the calculation used by the Modification of Diet in Renal Disease study [31] underestimates GFR values, particularly in the normal to high range [32, 33]. The precision of the various isotopic methods has also been questioned [34]. Also, the B–M equation, which corrects for the overestimation of GFR when using a plasma decay method, has not been used consistently in previous studies [9].
In this study we attempt to address the effect of age-related decline in GFR on the definition of hyperfiltration. In non-diabetic individuals, the GFR ‘physiologically’ declines at a rate of approximately 1 ml min−1 year−1 after the age of 40–50 years [16, 35, 36], which is the value used in the present study to calculate age-adjusted GFR values. Using data from this study, the rate of decline of GFR in our diabetic population was 1.8 ml min−1 year−1. However, it is arguable whether the estimation of the rate of GFR decline from cross-sectional data is reliable. In a longitudinal study series of renal function in type 2 diabetic patients with a mean age of 62, the overall rate of decline of GFR was −1.34 ml min−1 year−1 [37] over 3.5 years and −1.2 ml min−1 year−1 [38] over 5.5 years, with similar rates in normo- and microalbuminuric subjects, although considerable inter-individual variation was observed. The rate of GFR decline was significantly correlated with a higher baseline systolic blood pressure [37], lower baseline GFR [38], and higher AER and poorer glycaemic control in the group not treated with anti-hypertensives [38]. In another study, the rate of decline of GFR in 32 patients with type 2 diabetes was 1.68 ml min−1 year−1 when measured serially over 5 years [13].
Our study demonstrates that although adjusting the definition of hyperfiltration for age unmasks some hyperfiltering subjects, it is still a phenomenon that occurs predominantly in a younger population. This may be explained by the fact that systolic hypertension, reno-vascular disease, and increased arterial stiffness form a continuum with age in type 2 diabetes and these factors have been previously recognised to have a negative correlation with renal plasma flow [39, 40] and with GFR [7, 41]. Renal vascular resistance has been shown to be correlated with age in normal subjects [39] and blood flow to the renal cortex appears to be inversely related to renal vascular resistance. Also an increase in the filtration fraction has been demonstrated in ageing kidneys, especially in the deeper juxta-medullary glomeruli, and this has been described as an adaptive response for the preservation of renal function [39, 40, 42].
Previous studies have described renal structural changes that may be responsible for reduced total filtration capacity with ageing [43–46]. In summary, autopsy studies of non-diabetic subjects without a history of renal disease have demonstrated a reduction in renal weight and volume by approximately one-third between the fifth and ninth decades. An increase in the prevalence of global glomerulosclerosis, particularly in the outer cortical zone, a reduction in the absolute number of functioning glomeruli with age, and the development of shunts between the afferent and efferent arterioles have also been demonstrated. These findings may also explain why the difference in kidney size between the hyperfiltering and control groups was no longer significant when the definitions were adjusted for age in this study. It is possible that the effect of glomerular hypertrophy and nephromegaly may have been negated by the glomerular drop-out and the reduction of kidney size that occur with ageing, so that there is no net increase in kidney size in older hyperfiltering individuals compared to the subjects in the control group. This question can only be clarified by demonstrating hyperfiltration at a single nephron level in the remaining viable nephrons of the ageing diabetic kidney.
Although systemic hypertension is not a pre-requisite for intra-glomerular hypertension, when present, it is a well-recognised cause of elevated renal plasma flow and raised glomerular hydraulic pressure resulting in hyperfiltration [5]. By contrast, other studies have shown that chronic systemic hypertension is a major cause of irreversible reduction of GFR via loss of renal tissue and glomerular sclerosis [41]. This is further supported by Gragnoli et al. [7], who demonstrated a negative correlation between GFR and systolic blood pressure, the low prevalence of hyperfiltration in that study (6%) being at least partly attributable to the higher prevalence of systolic hypertension in the diabetic group compared to controls. In our patient population, the mean diastolic blood pressure was significantly lower (p=0.03) in the age-unadjusted and -adjusted hyperfiltration groups than in the control groups, a finding that was independent of age. There was also a trend towards a higher mean arterial pressure and a higher mean pulse pressure in the hyperfiltration groups than in normofiltering counterparts, although this difference was not statistically significant (p=0.09). The mean systolic blood pressure and use of renin–angiotensin system blocking agents were similar among the two groups. The reason for the association between hyperfiltration and lower diastolic blood pressure in this study is unclear. In the RENAAL study population of type 2 diabetic subjects, elevated pulse pressure was associated with adverse renal outcomes, although this may have been in the context of elevated systolic blood pressure rather than lower diastolic blood pressure in itself [47]. Another possible explanation is that the lower diastolic blood pressure in the hyperfiltration group may reflect a generalised vascular dilatation in these subjects. Indeed, renal hyperfiltration in diabetes is thought to be a result of differential dilatation of afferent versus efferent arterioles due to the action of various vaso-active substances [5, 48]. Atrial natriuretic peptide, endothelial-derived relaxing factor, prostaglandins, thromboxanes and kinins among others have been proposed to contribute to alterations in intra-renal haemodynamic regulation [48]. It is possible that the systemic arteries in these subjects are also susceptible to the action of these vaso-active factors, resulting in a degree of vasodilation that leads to lower diastolic pressure. However, a definite causal association between lower diastolic blood pressure and hyperfiltration remains elusive on the basis of the results of this study.
Hyperfiltration was independent of BMI in our study, in agreement with other studies [9]. This is in contrast to a study of Pima Indians that indicated a higher BMI in the hyperfiltrating diabetic group than in a non-diabetic control group [29]. In that study, the difference in GFR disappeared when GFR was corrected for BMI, implying that hyperfiltration in diabetes is related to higher BMI. The proportion of patients who were dyslipidaemic was similar in the two groups in the present study. Although elevated lipids are associated with progression of renal disease [49], the role of dyslipidaemia in patients with normal or elevated GFR has not been clarified. The 24-h urea excretion rates, which are a marker of dietary protein intake, were similar in the hyperfiltering and control subjects in our study. This finding is consistent with a previous study [9], which also concluded that the increase in GFR could not be attributed to higher protein intake.
Renal functional reserve has been shown to be well preserved with age in response to an acute protein load in a small number of healthy, non-diabetic individuals [39, 50], suggesting that a hyperfiltration capacity is preserved in the remaining viable glomeruli. Other authors report loss of the renal functional reserve as a manifestation of renal involvement in type 2 diabetes [51]. Therefore, one possible method of overcoming the effect of age on the threshold for hyperfiltration is to define it in terms of loss of functional renal reserve, i.e. failure of GFR to rise >10% after an acute protein load [51]. This definition of hyperfiltration would also incorporate individuals whose pre-morbid GFR is below the 25th percentile for the normal population, and would not reach the standard threshold for hyperfiltration unless the GFR is increased by more than 50%.
Our study has several strengths and limitations. To our knowledge, it is the first to explore (1) the effect of incorporating the age-related decline of GFR into the definition of hyperfiltration, and (2) the effect of that on factors associated with hyperfiltration. The employment of the B–M equation would explain the lower prevalence of hyperfiltration in this study compared to some earlier studies.
One potential limitation is the calendar effect, as more isotopic measurements of GFR have been ordered in recent years than in the early 1990s. However, the total study population of subjects who have had at least one diethylene-triamine-penta-acetic acid measurement of GFR is an unbiased representation of the total clinic population, as explained previously. Another possible limitation is that measurement of GFR by diethylene-triamine-penta-acetic acid may have missed the hyperfiltration phase in some patients, particularly if these patients started attending our centre 10–20 years after the onset of disease. Consequently, some of the ‘normofiltering subjects’ could have exhibited hyperfiltration during an earlier stage of the disease, and this might have resolved itself by the time GFR measurement was performed.
In current clinical practice, the discovery of microalbuminuria is considered to be the earliest predictor of clinical diabetic nephropathy [3]. The pathogenic significance of the events preceding microalbuminuria, particularly the hyperfiltration phase, is still under scrutiny. Our cross-sectional study has demonstrated that hyperfiltration occurs more commonly in younger patients with type 2 diabetes, even when the age-related decline of GFR is incorporated into its definition. The only associations we found with age-adjusted and unadjusted definitions of hyperfiltration were a lower mean diastolic blood pressure and a lower mean serum creatinine. Hyperfiltration appears to occur independently of BMI, glycaemic control, systolic blood pressure, mean arterial pressure, urea excretion as a marker of protein intake, salt excretion, lipid status, insulin therapy and the use of anti-hypertensives including renin–angiotensin system blockers. Also, hyperfiltration was not significantly associated with an increase in albuminuria in our study. The subjects in our study are being followed up prospectively to determine if hyperfiltration is associated with an accelerated deterioration of renal function compared to non-hyperfiltering diabetic subjects. If sufficient evidence for hyperfiltration as a putative risk factor for accelerated renal impairment can be demonstrated, this could help identify a subset of patients likely to benefit from even earlier intervention than currently recommended. Identification of masked hyperfiltration in the elderly may have other clinical implications. For example, it is possible that the fall in GFR that is sometimes observed following the commencement of a renin–angiotensin system blocking agent in the absence of renal artery stenosis may at least be partly explained by the resolution of (masked) hyperfiltration.
Finally, the age-adjusted approach used in our study not only has implications for the definition of hyperfiltration, but also raises the question of whether age-adjusted cut-offs for GFR should be used to define normofiltration and renal impairment, similarly, perhaps, to the classification of bone mineral densities according to T and Z scores.
Abbreviations
- AER:
-
albumin excretion rate
- B–M equation:
-
Bröchner–Mortensen equation
References
Cowie CC, Port FK, Wolfe RA, Savage PJ, Moll PP, Hawthorne VM (1989) Disparities in incidence of diabetic end-stage renal disease according to race and type of diabetes. New Engl J Med 321:1074–1079
Chaiken RL, Eckert-Norton M, Bard M et al (1998) Hyperfiltration in African–American patients with Type 2 diabetes. Diabetes Care 21:2129–2134
Mogensen CE (1986) Early glomerular filtration in insulin-dependent diabetes and late nephropathy. Scand J Clin Lab Invest 46:201–206
Hostetter TH (1992) Diabetic nephropathy: metabolic versus hemodynamic considerations. Diabetes Care 15:1205–1215
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1744–1777
Rudberg S, Persson B, Dahlquist G (1992) Increased glomerular filtration rate as a predictor of diabetic nephropathy—an 8-year prospective study. Kidney Int 41:822–828
Gragnoli G, Signorini AM, Tanganelli I et al (1993) Prevalence of glomerular hyperfiltration and nephromegaly in normo- and microalbuminuric type 2 diabetic patients. Nephron 65:206–211
John L, Mathews P, Oommnen R (1994) Glomerular filtration rate in Indian non-insulin dependent diabetes at various stages of albuminuria. Diabetes Res Clin Pract 23:121–125
Silviero S, Friedman R, Gross J(1993) Glomerular hyperfiltration in NIDDM patients without overt proteinuria. Diabetes Care 16(1):115–119
Bruce R, Rutland M, Cundy T (1994) Glomerular hyperfiltration in young Polynesians with type 2 diabetes. Diab Res Clin Pract 25:155–160
Vedel P, Obel J, Nielsen FS, Bang LE et al (1996) Glomerular hyperfiltration in microalbuminuric NIDD patients. Diabetologia 39:1584–1589
Keller CK, Bergis KH, Fliser D, Ritz E (1996) Renal findings in patients with short-term type 2 diabetes. J Am Soc Nephrol 7:2627–2635
Silviero SP, Friedman R, Azevedo MJ, Canani LH, Gross JL (1996) Five year prospective study of the glomerular filtration rate and albumin excretion rate in normofiltering and hyperfiltering normoalbuminuric NIDDM patients. Diabetes Care 19:171–174
Rius F, Pizarro E, Salinas I, Lucas A, Sanmarti A, Romero R (1995) Age as a determinant of glomerular filtration rate in non-insulin-dependent diabetes mellitus. Nephrol Dial Transplant 10:1644–1647
Sunder-Plassmann G, Horl WH (2003) A critical appraisal for definition of hyperfiltration. Am J Kidney Dis 43:396–397
Coresh J, Astor B, Greene T, Eknoyan G, Levey A (2002) Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third national health and nutrition examination survey. Am J Kidney Dis 41:1–12
Houlihan C, Jenkins M, Osicka T, Scott A, Parkin D, Jerums G (1999) A comparison of the plasma disappearance of iohexol and 99 mTc-DTPA for the measurement of glomerular filtration rate (GFR) in diabetes. Aust NZ J Med 29:693–700
Bröchner-Mortensen, J (1972) A simple method for the determination of glomerular filtration rate. Scand J Clin Lab Invest 30:271–274
World Health Organization (1985) Diabetes mellitus: report of a WHO Study Group. World Health Organ Tech Rep Ser 727:1–113
Kimmel PL, Lew SQ, Bosch JP (1996) Nutrition, ageing and GFR: is age-associated decline inevitable? Nephrol Dial Transplant 11(Suppl 9):85–88
Levy AS, Coresh J, Balk E et al (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification and stratification. Ann Intern Med 139:137–147
Nowack R, Raum E, Blum MD, Ritz E (1992) Renal haemodynamics in recent-onset Type 2 diabetes. Am J Kidney Dis 4:342–347
Vora JP, Dolben J, Dean JD et al (1992) Renal haemodynamics in newly presenting non-insulin dependent diabetes mellitus. Kidney Int 41:829–835
Viberti CG, Wiseman MJ (1986) The kidney size in diabetes: significance of early abnormalities. Clin Endocrinol Metab 15:753–782
Schmitz A, Hansen HH, Christensen T (1989) Kidney function in newly diagnosed Type 2 diabetic patients, before and during treatment. Diabetologia 32:434–439
Vora JP, Dolben J, Williams JD, Peters JR, Owens DR (1993) Impact of initial treatment on the renal function in newly diagnosed type 2 diabetes mellitus. Diabetologia 36:734–740
Soper CP, Barron JL, Hayer SL (1998) Long-term glycaemic control directly correlates with glomerular filtration rate in early type 1 diabetes mellitus before the onset of microalbuminuria. Diabet Med 15:1010–1014
Lee K-U, Park JY, Hwang IR et al (1995) Glomerular hyperfiltration in Koreans with non-insulin dependent diabetes mellitus. Am J Kidney Dis 26:722–726
Myers BD, Nelson RG, Williams GW et al (1991) Glomerular function in Pima Indians with non-insulin dependent diabetes mellitus of recent onset. J Clin Invest 88:524–530
Cockroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999). A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Lin J, Knight E, Hogan M, Singh A (2003) A comparison of prediction equations for estimating glomerular filtration rate in adults without kidney disease. J Am Soc Nephrol 14:2573–2580
Rule AD, Larson TS, Bergstralh EJ et al (2004) Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med 141:929–937
Itoh K (2003) Comparison of methods for determination of glomerular function rate; Tc-99m-DPTA renography, predicted creatinine clearance method and plasma sample method. Ann Nucl Med 17:561–565
Davies DF, Shock NW (1950) Age changes in glomerular filtration rate, effective renal plasma flow and tubular excretory capacity in adult males. J Clin Invest 29:496–507
Linderman RD, Tobin J, Shock NW (1985) Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc 33:278–285
Nielsen S, Schmitz A, Rehling M, Mogensen CE (1993) Systolic blood pressure relates to the rate of decline of glomerular filtration rate in type 2 diabetes. Diabetes Care 16:1427–1432
Nielsen S, Schmitz A, Rehling M, Mogensen CE (1997) The clinica course of renal function in NIDDM patients with normo- and microalbuminuria. J Intern Med:133–141
Fliser D, Zeier M, Nowack R, Ritz E (1993) Renal functional reserve in healthy elderly subjects. J Am Soc Nephrol 3:1371–1377
Hoang K, Tan JC, Derby G et al (2003) Determinants of glomerular hypofiltration in aging humans. Kidney Int 64:1417–1424
Bakris GL (1998) Progression of nephropathy: a focus on arterial pressure level and methods of reduction. Diabetes Res Clin Pract 39(suppl):35–43
Linderman RD (1998) Is the decline in renal function with normal ageing inevitable? Geriatr Nephrol Urol 8:7–9
Linderman RD (1990) Overview: renal physiology and pathophysiology of ageing. Am J Kidney Dis 16:275–282
Kappel B, Olsen S (1980) Cortical interstitial tissue and sclerosed glomeruli in the normal human kidney, related to age and sex. Virchows Arch A Path Anat Histol 387:271–277
Kasiske BL (1987) Relationship between vascular disease and age associated changes in the human kidney. Kidney Int 31:1153–1159
Lamb EJ, O’Riordan SE, Delaney MP (2003) Kidney function in older people: pathology, assessment and management. Clin Chim Acta 334:25–40
Bakris GL, Weir MR, Shanifar S et al for the RENAAL study group (2003) Effects of blood pressure level on progression of diabetic nephropathy: results from the RENAAL study. Arch Intern Med 163:1555–1565
Anderson S, Vora JP (1995) Current concepts of renal haemodynamics in diabetes. J Diabet Complications 9:304–307
Ravid M, Neumann L, Lishner M (1995) Plasma lipids and the progression of nephropathy in diabetes mellitus type II: effect of ACE inhibitors. Kidney Int 47:907–910
Fliser D, Ritz E, Franek E (1995) Renal reserve in the elderly. Semin Nephrol 15:463–467
Guizar J-M, Kornhauser C, Malacara JM, Armador N, Barrera JA, Esparza R (2001) Renal function reserve in patients with recently diagnosed type 2 diabetes mellitus with and without microalbuminuria. Nephron 87:223–230
Acknowledgements
This study was supported by research grants from the Austin Health Medical Research Fund (AHMRF) and National Health and Research Council (NHMRC, Australia).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Premaratne, E., MacIsaac, R.J., Tsalamandris, C. et al. Renal hyperfiltration in type 2 diabetes: effect of age-related decline in glomerular filtration rate. Diabetologia 48, 2486–2493 (2005). https://doi.org/10.1007/s00125-005-0002-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-0002-9