Abstract
Aims/hypothesis
AGE contribute to the pathogenesis of diabetic complications, including dyslipidaemia and atherosclerosis. However, the precise mechanisms remain to be established. In the present study, we examined whether AGE modification of apolipoprotein A-I (apoA-I) affects its functionality, thus altering its cardioprotective profile.
Materials and methods
The ability of AGE-modified apoA-I to facilitate cholesterol and phospholipid efflux, stabilise ATP-binding cassette transporter A1 (ABCA1) and inhibit expression of adhesion molecules in human macrophages and monocytes was studied.
Results
The ability of AGE-modified apoA-I to promote cholesterol efflux from THP-1 macrophages, isolated human monocytes and from ABCA1-transfected HeLa cells was significantly reduced (>70%) compared with unmodified apoA-I. This effect was reversed by preventing AGE formation with aminoguanidine or reversing AGE modification using the cross-link breaker alagebrium chloride. AGE-modification of HDL also reduced its capacity to promote cholesterol efflux. AGE–apoA-I was also less effective than apoA-I in stabilising ABCA1 in THP-1 cells as well as in inhibiting expression of CD11b in human monocytes.
Conclusions/interpretation
AGE modification of apoA-I considerably impairs its cardioprotective, antiatherogenic properties, including the ability to promote cholesterol efflux, stabilise ABCA1 and inhibit the expression of adhesion molecules. These findings provide a rationale for targeting AGE in the management of diabetic dyslipidaemia.
Similar content being viewed by others
Introduction
Both type 1 and type 2 diabetes are associated with increased risk of developing atherosclerosis and coronary artery disease (CAD) [1, 2]. While diabetic dyslipidaemia appears to be an important pro-atherogenic factor [3, 4], changes in the lipid profile are not sufficient to explain the increased cardiovascular risk observed in diabetes. Moreover, diabetes per se has both independent and additive contributions over and above that of dyslipidaemia towards the development and progression of atherosclerotic lesions [5, 6]. This suggests that not only quantitative, but also functional changes in lipid metabolism induced by diabetes may contribute significantly to the accelerated atherosclerosis associated with diabetes. Hence, not only plasma concentrations of lipoproteins, but also their functional properties are affected by glucose-induced modifications and may be critical for diabetes-induced atherosclerosis.
Functional changes in both forward and reverse cholesterol transport may be important in mediating diabetes-associated atherosclerosis. While the role of diabetes-induced changes in the forward cholesterol transport branch of lipoprotein metabolism has been thoroughly investigated [3], information on the effect of diabetes on reverse cholesterol transport (RCT) is limited. Type 2 diabetes is consistently associated with reduced levels of HDL [7], and the composition, and possibly the functionality, of HDL particles are also altered in diabetic patients [7]. The rate-limiting step of RCT is cholesterol efflux, which contributes both to the regulation of plasma HDL levels [8] and to maintaining macrophage cholesterol homeostasis [9]. Cholesterol efflux in diabetic patients can be impaired by a number of mechanisms, including the effects of increased concentration of fatty acids [10] or glucose [11] on ATP-binding cassette, transporter A1 (ABCA1). Further, AGE modification of ABCA1 inhibits its function as well as its abundance in the macrophages of diabetic patients [12]. Another factor likely to contribute to the impairment of cholesterol efflux is the modification of HDL and apolipoprotein A-I (apoA-I) induced by factors associated with diabetes, such as nitration [13]. Simple glycation of HDL apparently does not affect its ability to promote cholesterol efflux [14]; however, non-enzymatic glycosylation of HDL has been reported to impair its ability to bind to the cell surface receptors on human fibroblasts [15] and to support the efflux of intracellular cholesterol [16]. The potential effects of advanced glycation of apoA-I and the majority of the elements of RCT have not been examined previously. In the present study, we assess for the first time the effect of AGE modification of HDL and apoA-I on RCT and other anti-atherogenic properties.
Materials and methods
Cells
THP-1 cells (a human monocyte–macrophage cell line) were cultured in RPMI 1640, 10% fetal bovine serum, 100 units/ml penicillin, 100 μg/ml streptomycin and 2 mmol/l glutamine (all reagents were from JRH Biosciences, Brooklyn, VIC, Australia). Cells were seeded at a density of 106 cells per well in 12-well tissue culture plates and cultured for 48 h. Phorbol myristate acetate (PMA) was added to differentiate the cells at the final concentration of 100 ng/ml. When indicated, cells were treated for 18 h with the liver X receptor (LXR) agonist T0-901317 (Sigma, St Louis, MO, USA) at the final concentration of 1 μmol/l.
HeLa cells were transfected with ABCA1 or ATP-binding cassette transporter G1 (ABCG1) (a kind gift of A. Remaley) using Lipofectamine Plus Reagent (Invitrogen, Mount Waverley, VIC, Australia) according to the manufacturer’s recommendations. Cells were treated for 18 h with 1 μmol/l 5′-azacytidine to prevent methylation of the cytomegalovirus (CMV) promoter [17].
Resting human monocytes were isolated from whole blood using the Dynal negative isolation kit (Invitrogen) [18].
Cholesterol acceptors
HDL was isolated by sequential centrifugation from plasma obtained from healthy volunteers (n = 5) and patients with diabetes and kidney disease (n = 10). Samples were provided with the written consent of all participants and the approval of the Austin Health human ethics committee. HDL for in vitro experiments was isolated from pooled plasma provided by the Red Cross. ApoA-I was isolated as described previously [19]. Reconstituted HDL (rHDL) (apoA-I/POPC 1:80 mol/mol) was prepared as described previously [20].
AGE modification
Lipid-free apoA-I, isolated plasma HDL and human serum albumin (HSA) from healthy volunteers were modified by incubation with ribose (final concentration 0.5 mol/l) at 37°C for 18 h followed by dialysis with PBS, and further incubated for 5 days unless indicated otherwise. Glycated samples were dialysed extensively and sterilised by filtration.
To account for changes introduced by prolonged incubation, control preparations were also treated under identical conditions but without ribose (designated here as ‘treated’ proteins). Carboxymethyllysine (CML) levels were measured by indirect ELISA and expressed as μg CML/mg protein. Because of considerable variation in the AGE levels in human samples, results are expressed as their geometric mean. In vitro modification with methylglyoxal (MGO) has also been suggested to provide a good representation of physiological AGE modification [21, 22]. Purified apoA-I was modified by incubation with the indicated concentration of MGO at 37°C for 18 h. Excess MGO was removed by dialysis before samples were further incubated at 37°C for 72 h. Samples were then dialysed extensively and sterilised by filtration. In additional experiments, human apoA-I was also glycated by incubation with d-glucose (final concentration 0.5 mol/l) in the presence or absence of aminoguanidine (450 nmol/l) at 37°C for the indicated period of time.
Cholesterol and phospholipid efflux
Cellular cholesterol or phospholipids were labelled by incubation in serum-containing medium with [1α,2α(n)-3H]cholesterol (GE Healthcare-Amersham, Rydalmere, NSW, Australia; specific radioactivity 1.81 TBq/mmol, final radioactivity 0.5 MBq/ml) or [methyl-14C]choline (0.2 MBq/ml) for 48 h at 37°C in a CO2 incubator. After labelling, cells were washed and further incubated for 18 h in serum-free medium. Cells were then washed and incubated for 2 h at 37°C in serum-free medium containing either lipid-free apoA-I or rHDL (final concentration 30 μg/ml) or isolated HDL (final concentration 40 μg/ml). The medium was collected and centrifuged to remove cellular debris, and the radioactivity in the supernatant fractions was measured. Cells were harvested and dispersed in 0.5 ml distilled water, and aliquots were counted. For phospholipid efflux, phospholipids were isolated from medium and cells by thin-layer chromatography as described previously [23], and radioactivity was measured. Cholesterol and phospholipids efflux were expressed as the percentage of labelled cholesterol or phospholipid transferred from cells to the medium.
Cholesterol esterification
To assess cholesterol esterification, cells were incubated for 2 h at 37°C with [14C]oleic acid (GE Healthcare-Amersham; specific activity 2.22 GBq/mmol; final radioactivity 0.185 MBq/ml) complexed to BSA (Sigma; essentially fatty-acid-free). Where indicated, cells were preloaded with cholesterol by incubation for 24 h with acetylated LDL (AcLDL) (final concentration 50 μg/ml). Cells were washed and lipids were extracted and analysed by thin-layer chromatography as described previously [24]. Spots of cholesterol and cholesteryl oleate were identified by standards (Sigma), scraped and counted in a beta-counter.
ABCA1 stability
Cells were grown as described above and ABCA1 expression was induced by incubation for 18 h with the LXR agonist T0-901317 (1 μmol/l). Cells were then washed and incubated for 18 h at 37°C in the presence or absence of apoA-I or AGE-apoA-I (final concentration 30 μg/ml). Cells were then lysed by incubation in 5 mmol/l Tris–HCl (pH 7.5) containing protease inhibitor cocktail (Roche, Kew, VIC, Australia) at 4°C and soluble membrane protein fractions were isolated as described in [25]. ABCA1 abundance was then analysed by western blot using monoclonal anti-ABCA1 antibody and quantitated using the Quantity One documentation system (Bio-Rad, Regents Park, NSW, Australia).
Expression of CD11b on human monocytes
Resting human monocytes were isolated from whole blood and resuspended at 106 cells/ml. One hundred microlitres of the suspension was stimulated with PMA (final concentration 100 ng/ml) in the presence or absence of apoA-I, treated apoA-I or AGE-apoA-I (40 μg/ml) and incubated with fluorescein isothiocyanate (FITC)-conjugated antibody against the active epitope of CD11b for 15 min at 37°C. Cells were then fixed with 4% paraformaldehyde. Controls used were unstimulated monocytes and the isotype-matched irrelevant antibody (FITC-anti-mouse IgG). CD11b expression was measured as fluorescence intensity by the use of a FACSCalibur flow cytometer (Beckman, Glagesville, NSW, Australia). Analysis was conducted using the Cell Quest Pro software (BD Biosciences, San Jose, CA, USA).
Confocal microscopy
THP-1 cells were differentiated and cultured for 72 h on sterile collagen-coated glass coverslips. Cells were washed with PBS then incubated with apoA-I or AGE-apoA-I in serum-free media for 18 h at 37°C, washed with PBS and fixed in acetone for 10 min at –20°C. This was followed by incubation for 1 h with purified monoclonal anti-ABCA1 antibody (5 μg/ml), and with secondary Alexa Fluor anti-mouse IgM antibodies (5 μg/ml). Cells were observed using a Zeiss Meta confocal microscope.
Statistics
All experiments were replicated two to four times and representative experiments are shown unless indicated otherwise. Means±SD of quadruplicate determinations are shown. Student’s t test was used to determine the statistical significance of the differences. Correlation was analysed using Spearman rank order correlation.
Results
AGE modification of apoA-I and HDL
To assess the effects of AGE modification on apoA-I and HDL functionality, lipid-free apoA-I, isolated plasma HDL and HSA were modified by incubation with ribose (see Methods). To account for changes introduced by prolonged incubation, the preparations were also treated under identical conditions without ribose (designated here as ‘treated’ proteins). Treatment of apoA-I and HDL in the absence of ribose did not affect their size as assessed by PAGE, while AGE modification slightly increased the size of apoA-I and HDL (Fig. 1a, b). Importantly, AGE modification uniformly affected all apoA-I molecules and HDL particles without formation of separate subpopulations of modified particles. The AGE CML was found both in apoA-I and HDL treated with ribose in physiological concentrations, but was absent from untreated samples and samples incubated in the absence of ribose (Fig. 1a, b).
Characterisation of AGE-modified apoA-I and HDL. a, b ApoA-I and HDL were AGE-modified using incubation with ribose as described in the Materials and methods. T-apoA-I and T-HDL denote treated apoA-I or HDL, which were incubated under conditions identical to those used for AGE modification but in the absence of carbohydrate. Tables in a and b show concentration of CML determined by ELISA as described in Materials and methods. ND, not detected. a 12% SDS-PAGE of unmodified, treated and AGE-modified apoA-I (Coomassie Blue staining). b Native 4–20% PAGE of unmodified, treated and AGE-modified HDL (Coomassie Blue staining). c HDL was isolated from plasma of five healthy subjects (controls) and ten patients with renal deficiency (patients). AGE-apoA-I and AGE-HDL were prepared as described in Materials and methods. AGE-apoA-I (RB), AGE-apoA-I modified with ribose; AGE-apoA-I (GL), AGE-apoA-I modified with glucose (12 weeks incubation). CML in HDL was determined as described in Materials and methods. Geometrical means±SD are shown. *p < 0.01 vs CML in HDL of healthy subjects
To assess the possible level of AGE modification of HDL in diabetic patients, HDL was isolated from plasmas of ten diabetic subjects with kidney disease (a group of patients known to have high levels of circulating AGE); CML levels in plasma protein and isolated HDL were compared with those of five healthy individuals. The levels of CML in patient plasmas were 1.7-fold higher than those in the plasmas of healthy subjects (3.0 ± 1.7 vs 1.8 ± 0.5 μg/mg protein). By contrast, the concentration of CML in HDL fractions was almost tenfold higher in diabetic subjects with kidney disease compared with healthy subjects and similar to the levels of CML observed in apoA-I and HDL modified in vitro (Fig. 1c).
Cholesterol and phospholipid efflux to AGE-modified apoA-I
Cholesterol efflux from THP-1 human macrophages to AGE-modified apoA-I was inhibited by 70% compared with the untreated apoA-I added at the same concentration (Fig. 2a). ApoA-I incubated in the absence of ribose was not significantly altered in its ability to promote cholesterol efflux from that observed in untreated samples (Fig. 2a). Further, we confirmed these changes in cholesterol efflux to apoA-I and AGE-modified apoA-I in experiments using isolated human blood monocytes instead of THP-1 cells. In these studies, cholesterol efflux from human monocytes to AGE-modified apoA-I was also threefold lower than to unmodified apoA-I (Fig. 2b).
Cholesterol and phospholipid efflux from macrophages to apoA-I. ApoA-I was AGE-modified by incubation with ribose as described in Materials and methods. Cholesterol efflux experiments were performed as described in Materials and methods. T-apoA-I denotes treated apoA-I, i.e. apoA-I incubated under conditions identical to those used for AGE modification but in the absence of carbohydrate. a Cholesterol efflux from THP-1 cells activated (closed bars) or not (open bars) with T0-901317 (18 h, final concentration 1 μmol/l) to the unmodified, treated or AGE-modified apoA-I (final concentration 30 μg/ml). b Resting human monocytes were plated into 12-well plates and allowed to adhere and spread on the surface. Cells were then labelled with [14C]cholesterol and tested in cholesterol efflux experiments exactly as described for THP-1 cells (see Methods). c Phospholipid efflux from THP-1 cells activated with T0-901317 to unmodified apoA-I or AGE-apoA-I (final concentration 30 μg/ml). d Cholesterol efflux to apoA-I (left) or AGE-apoA-I (right) either untreated (open bars) or treated with alagebrium chloride (0.1 mg/ml) (hatched bars, ALT) or aminoguanidine (450 nmol/l) (closed bars, AG). *p < 0.01
To investigate whether impairment of cholesterol efflux to AGE-modified apoA-I affects the ABCA1-dependent pathway, ABCA1 expression in the cells was boosted by overnight treatment with the LXR agonist T0-901317. This treatment significantly increased the rate of cholesterol efflux. However, AGE modification of apoA-I with ribose reduced LXR agonist-induced cholesterol efflux by 70% (Fig. 2a). ApoA-I incubated without ribose retained had an ability to support cholesterol efflux from activated cells similar to that of untreated apoA-I (Fig. 2a). To further confirm the involvement of the ABCA1-dependent cholesterol efflux pathway, the effect of AGE modification of apoA-I on phospholipid efflux was tested. The efflux of phospholipid to AGE-apoA-I from THP-1 cells activated with T0-901317 was halved compared with the efflux to unmodified apoA-I (Fig. 2c).
To exclude the possibility of a non-specific effect of AGE moiety on cholesterol efflux, THP-1 cells were pre-incubated for 18 h with AGE-modified HSA. No effect of AGE-modified HSA on cholesterol efflux was observed when HSA was either removed from the incubation mixture before adding apoA-I or when AGE HSA was left in the incubation mixture during the efflux (3.9 ± 0.5 and 3.8 ± 0.2% for unmodified and AGE-modified HSA respectively).
Effects of inhibitors of advanced glycation on cholesterol efflux
The effect of AGE modification of apoA-I on cholesterol efflux was further tested using two compounds that attenuate AGE modification. First, we used the putative AGE crosslink breaker alagebrium chloride (ALT-711) [26]. When AGE-modified apoA-I was pretreated with 0.1 mg/ml alagebrium chloride, its ability to support cholesterol efflux was fully restored (Fig. 2d). Second, we used aminoguanidine, which prevents the formation of AGE [27]. Prolonged incubation of apoA-I with aminoguanidine enhanced the ability of apoA-I to promote cholesterol efflux; however, cholesterol efflux was similar for apoA-I and apoA-I modified in the presence of aminoguanidine (Fig. 2d).
Alternative pathways for AGE modification of apoA-I
Although AGE modification using ribose allows the rapid preparation of AGE-modified protein, the exact composition of AGE may be different from that found in vivo, where non-enzymatic glycosylation is induced by glucose, although both sugars ultimately lead to the formation of AGE, albeit at different rates. To confirm the results seen with ribosylation of apoA-I, we also incubated apoA-I with glucose. This resulted in the formation of detectable amounts of the AGE-modified protein by 4 weeks and high concentrations after incubation for 12 weeks, as assessed by ELISA for CML (Fig. 3a). No CML-modified proteins were formed in the absence of sugar (Fig. 3a). As with ribose, there was also a dose-dependent reduction in the ability of apoA-I to promote cholesterol efflux from T0-901317-activated THP-1 cells (Fig. 3b). A significant negative correlation was observed between the concentration of CML in apoA-I and its ability to promote cholesterol efflux (r = −0.9, p < 0.02). Addition of aminoguanidine to the incubation mixture with glucose reduced the amount of AGE modification by 20% and partly restored the ability of apoA-I to promote cholesterol efflux (Fig. 3b).
Alternative pathways for AGE modification of apoA-I. a Time course of the changes in CML concentration after modification with glucose. ApoA-I was AGE-modified by incubation in the presence or absence of glucose for the indicated periods of time as described in Materials and methods. Closed circles, ApoA-I incubated with glucose; open circles, apoA-I incubated without glucose. b Dependence of the ability of apoA-I (final concentration 30 μg/ml) to promote cholesterol efflux from THP-1 cells on time of incubation with glucose in the presence or absence of aminoguanidine (450 nmol/l). Closed circles, ApoA-I incubated with glucose; open circles, apoA-I incubated with glucose in the presence of aminoguanidine (450 nmol/l). c Dependence of the ability of apoA-I (final concentration 30 μg/ml) AGE-modified by incubation with MGO to promote cholesterol efflux from THP-1 cells. MGO concentration refers to the concentration used to modify apoA-I (described in Materials and methods). d Cholesterol efflux from THP-1 cells to unmodified, treated and AGE-modified HDL (final concentration 40 μg/ml). *p < 0.01
Another physiologically relevant mechanism of AGE modification is through the action of MGO. MGO levels are elevated in diabetes [21, 22], in which they correlate with the extent of AGE modification better than glucose levels. In our experiments, various concentrations of MGO sharply reduced the functionality of apoA-I towards cholesterol efflux (Fig. 3c).
Cholesterol efflux to AGE-modified HDL
Most of the apoA-I in plasma is lipidated and is a constituent of HDL. Therefore the effect of the AGE modification of HDL on its ability to promote cholesterol efflux was also examined. Cholesterol efflux to HDL is likely to be mediated by several pathways, including ABCG1- and SR-B1-dependent pathways. When cholesterol efflux from THP-1 cells to HDL was tested, there was a statistically significant reduction of cholesterol efflux to AGE-modified HDL, whereas the efflux to HDL incubated in the absence of ribose was similar to that in untreated samples (Fig. 3d).
Mechanisms of impairment of cholesterol efflux to AGE-modified apoA-I and HDL
To further investigate the mechanism of the reduced ability of AGE-modified apoA-I to promote cholesterol efflux, we used HeLa cells transiently transfected with ABCA1 or ABCG1. HeLa cells do not express ABC transporters [28] and cholesterol efflux to lipid-free apoA-I in mock-transfected cells was minimal (Fig. 4a). However, there was considerable efflux from HeLa cells to both rHDL (apoA-I/POPC complex) and native HDL. The efflux from HeLa cells to rHDL assembled with AGE-modified apoA-I was 25% lower than rHDL containing unmodified apoA-I (Fig. 4a). The efflux to AGE-modified HDL was fourfold lower than unmodified HDL (Fig. 4a). Transfection of HeLa cells with ABCA1 dramatically increased the efflux to apoA-I, but not to AGE-modified apoA-I (Fig. 4b). Furthermore, there was no difference in cholesterol efflux to apoA-I in ABCG1-transfected cells (Fig. 4c), indicating that advanced glycation of apoA-I specifically affects ABCA1-dependent cholesterol efflux. Transfection of HeLa cells with ABCG1 elevated cholesterol efflux to HDL, but not to rHDL (Fig. 4c). There was 40% reduction of cholesterol efflux to AGE-modified HDL compared with unmodified HDL and 10% reduction in the efflux to AGE-rHDL compared with unmodified rHDL (Fig. 4c). These findings indicate that advanced glycation of HDL affects both the ABCG1-dependent and ABCG1-independent pathways. The experiments with HDL were only done with HDL modified by ribose, as long incubations of HDL with glucose resulted in disintegration of HDL particles independently of the presence of glucose, precluding use of this method to study AGE modification of HDL.
Cholesterol efflux from HeLa cells mock-transfected (a) or transfected with ABCA1 (b) or ABCG1 (c). HeLa cells were transfected with pCMV empty plasmid (a), ABCA1 (b) or ABCG1 (c) as described in Materials and methods. Cholesterol efflux assay to apoA-I or AGE-apoA-I, rHDL or AGE-rHDL and HDL and AGE-HDL was performed as described in Materials and methods. Open bars, ApoA-I, rHDL or HDL; closed bars, AGE-modified apoA-I, rHDL or HDL. *p < 0.01
Intracellular cholesterol content
Differences in the rate of cholesterol efflux are likely to be reflected in the steady-state concentration of intracellular cholesterol. A sensitive measure of cellular cholesterol content is the rate of cholesteryl ester synthesis [29]. We measured the rate of cholesterol ester synthesis in THP-1 cells before and after loading the cells with cholesterol by incubation with AcLDL. As expected, loading cells with cholesterol increased the rate of cholesteryl ester synthesis, whereas addition of apoA-I to the incubation mixture decreased it (Fig. 5). AGE-modified apoA-I was ineffective in decreasing the rate of cholesteryl ester synthesis in unloaded cells and less effective in cholesterol-loaded cells compared with native apoA-I (Fig. 5).
Effect of apoA-I and AGE-modified apoA-I on the rate of cholesterol esterification. THP-1 cells were incubated for 24 h in the absence (left) or presence (right) of AcLDL (50 μg/ml). The rate of cholesteryl ester synthesis was then measured as described in Materials and methods in the absence (open bars) or presence of apoA-I (hatched bars) or AGE-modified apoA-I (closed bars; final concentration 30 μg/ml). *p < 0.01 vs no apoA-I
AGE modification of apoA-I and ABCA1 stability
The contribution of apoA-I to RCT is not limited to it being a cholesterol acceptor. Another important function of apoA-I is its ability to enhance ABCA1 abundance by inhibiting calpain-dependent degradation of ABCA1 [30, 31]. To test whether this function of apoA-I is affected by AGE modification, we boosted ABCA1 expression in differentiated THP-1 cells using the LXR agonist T0-901317. The agonist was then removed and cells were incubated for 18 h in the presence or absence of apoA-I or AGE-apoA-I in serum-free media. The abundance of ABCA1 was measured by western blot followed by densitometry and related to the abundance of β-actin. Most of the ABCA1 disappeared after 18 h incubation in the absence of apoA-I (Fig. 6a). Incubation in the presence of apoA-I preserved ABCA1 while AGE-modified apoA-I was less effective (Fig. 6a). Similar conclusions could be drawn from experiments in which THP-1 cells were immunostained with anti-ABCA1 antibody. While most of the ABCA1 on the plasma membrane was preserved in cells incubated with apoA-I, much less ABCA1 was found on the plasma membrane of cells incubated with AGE-modified apoA-I or in the absence of apoA-I (Fig. 6b–d).
Effect of apoA-I and AGE-apoA-I on ABCA1 stability. THP-1 cells were incubated for 18 h in the presence of LXR agonist T0-901317 (1 μmol/l). The agonist was then washed out and cells were incubated for 18 h in serum-free media in the presence or absence of apoA-I or AGE-apoA-I (final concentration 30 μg/ml). a Quantitation of ABCA1 abundance. Cell membranes were subjected to SDS-PAGE as described in Materials and methods. Abundances of ABCA1 and β-actin were quantitated by densitometry of western blots; ratio of ABCA1/β-actin is presented. *p < 0.01 vs without apoA-I; # p < 0.05 vs apoA-I. b–d Confocal microscopy. b Cells incubated in the absence of apoA-I; c cells incubated in the presence of apoA-I; d cells incubated in the presence of AGE-apoA-I. Bar = 10 μm
AGE modification of apoA-I and expression of CD11b on monocytes
It has been demonstrated in a number of studies that HDL and apoA-I have anti-inflammatory properties inhibiting the expression of various adhesion molecules [32]. We also tested whether the AGE modification of apoA-I impairs its ability to inhibit expression of CD11b in primary human monocytes stimulated by PMA. Consistent with the impairment observed in the other functions of apoA-I, AGE-modified apoA-I was ineffective at inhibiting the expression of CD11b. By contrast, both untreated apoA-I and apoA-I incubated in the absence of ribose inhibited expression of CD11b (Fig. 7).
Effect of apoA-I and AGE apoA-I on CD11b expression on human monocytes. Resting human monocytes were resuspended at 106 cells/ml and 100 μl of this suspension was stimulated with PMA (final concentration 100 ng/ml) in the presence or absence of apoA-I, treated apoA-I (T-apoA-I) or AGE-apoA-I (40 μg/ml). Cells were incubated with the FITC-conjugated antibody against CD11b for 15 min at 37°C and fixed with 4% paraformaldehyde. CD11b expression was measured as fluorescence intensity using flow cytometry. Values shown are percentage increases in the expression of CD11b over non-stimulated monocytes. Means±SEM for four independent experiments are shown. *p < 0.01 vs PMA alone; # p < 0.05 vs PMA+apoA-I
Discussion
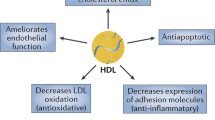
The presence of high levels of AGE in plasma is a characteristic feature of diabetes, with mounting evidence of a significant role of AGE in diabetic complications [33]. High plasma concentrations of AGE have been associated with increased rates of CAD [34] as well as kidney damage [35]. AGE modifications have also been reported to cause changes in lipoprotein metabolism affecting properties of LDL particles [36], expression of lipoprotein lipase [37] and the functionality of scavenger receptors, including SR-B1 [38]. Most of these effects were related to common AGE moieties, such as CML [39], and not related to a specific protein. In addition to the effects of AGE moiety, AGE modification can affect specific functions of specific proteins contributing to the impairment of metabolic regulation. For example, AGE modification of ABCA1 has a dramatic effect on cholesterol efflux [12]. Persistent hyperglycaemia and oxidative stress in diabetes act to hasten the formation of AGE, ensuring not only that long-lived proteins become more heavily modified, but also that short-lived molecules such as apoA-I become targets for AGE modification [40]. In addition to their role in RCT, apoA-I and HDL have other anti-atherogenic functions, including anti-inflammatory [32], antioxidant [41] and antithrombotic actions [42]. Hence, AGE modification of apoA-I may have wide-ranging implications for the development of atherosclerosis, particularly in the setting of diabetes. In this study we investigated the effect of AGE modification of apoA-I on several of its anti-atherogenic functions.
The main finding of this study is that a number of the known anti-atherogenic functions of apoA-I were impaired by a physiologically relevant level of AGE modification of this specific protein. These functions include cholesterol efflux. The cholesterol efflux pathway affected was likely to be mainly, but not exclusively, the ABCA1-dependent pathway. This conclusion is supported by the greater inhibition of cholesterol efflux to AGE-apoA-I compared with AGE–HDL, concomitant inhibition of phospholipid efflux and almost complete inhibition of cholesterol efflux to AGE-apoA-I from ABCA1-transfected HeLa cells, where ABCA1-dependent cholesterol efflux is the only pathway for removing cholesterol to apoA-I. However, inhibition of cholesterol efflux to AGE–HDL indicates that the other cholesterol efflux pathways, including the ABCG1-dependent pathway, are also affected. The changes in cholesterol efflux were specific for AGE-modification of apoA-I as AGE-HSA had no effect on cholesterol efflux. The reduced ability of AGE-apoA-I to support cholesterol efflux was reflected in its reduced capacity to decrease cell cholesterol content as assessed by the rate of cholesterol esterification. The impairment of cholesterol efflux was reversed by preventing or reversing AGE modification of apoA-I. Interestingly, simple glycation of apoA-I does not seem to affect its ability to promote cholesterol efflux [14], emphasising that further modification with the formation of AGE is necessary for impairment of apoA-I function. Our finding is consistent with that of Brubaker et al. [43] showing that reductive methylation of lysine residues impairs the ability of apoA-I to support cholesterol efflux, and with that of Duell et al. [16] showing that non-enzymatic glycosylation of HDL impairs its function. Thus, AGE-modification of apoA-I and HDL results in a significant loss of its ability to support cholesterol efflux, which can be reversed by either inhibiting or reversing AGE-modification. These findings provide a rationale for targeting AGE as part of the management of diabetic dyslipidaemia and cardioprotection.
Other functions of apoA-I impaired by AGE-modification included its ability to stabilise ABCA1 [31] and to inhibit expression of adhesion molecules [32]. The former further impairs RCT, and the latter is a reflection of the anti-inflammatory function of apoA-I. Inflammation is an important element in the pathogenesis of atherosclerosis and the anti-inflammatory properties of apoA-I are likely to contribute to its overall anti-atherosclerotic effect [44].
The clinical relevance of AGE modification to the functions of apoA-I in vivo remains to be tested. Although the concentration of CML found in the in vitro-modified apoA-I used in this study was similar to that found in vivo, it is conceivable that other AGE-modifications may contribute to protein dysfunction, and may be different from that observed in vivo. Moreover, AGE modification is not the only apoA-I modification observed in diabetes that potentially contributes to impaired apoA-I functions. In particular, nitration and chlorination of apoA-I also occur in diabetes, damaging apoA-I functionality [13, 45, 46]. While the relative contribution of AGE modification to the overall effect of diabetes on apoA-I dysfunction is yet to be established, it is clear that interventions to reduce AGE levels in diabetes are anti-atherosclerotic [47].
In conclusion, we demonstrated that AGE modification of apoA-I and HDL results in a significant loss of their ability to support cholesterol efflux, stabilise ABCA1 and inhibit the expression of CD11b. These changes appear to be specific to the AGE modification of apoA-I and can be attenuated by preventing AGE modification. The impaired functioning of AGE-modified apoA-I may contribute significantly to the increased risk of atherosclerosis associated with diabetes.
Abbreviations
- ABCA1:
-
ATP-binding cassette transporter A1
- ABCG1:
-
ATP-binding cassette transporter G1
- AcLDL:
-
Acetylated low density lipoprotein
- apoA-I:
-
Apolipoprotein A-I
- CAD:
-
Coronary artery disease
- CML:
-
Carboxymethyllysine
- FITC:
-
Fluorescein isothiocyanate
- HSA:
-
Human serum albumin
- LXR:
-
Liver X receptor
- MGO:
-
Methylglyoxal
- PMA:
-
Phorbol myristate acetate
- POPC:
-
Palmitoyloleoyl phosphatidylcholine
- RCT:
-
Reverse cholesterol transport
References
Nathan DM, Cleary PA, Backlund JY et al (2005) Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 353:2643–2653
Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339:229–234
Beckman JA, Creager MA, Libby P (2002) Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 287:2570–2581
Goldberg IJ (2004) Why does diabetes increase atherosclerosis? I don’t know! J Clin Invest 114:613–615
Renard CB, Kramer F, Johansson F et al (2004) Diabetes and diabetes-associated lipid abnormalities have distinct effects on initiation and progression of atherosclerotic lesions. J Clin Invest 114:659–668
Kanter JE, Johansson F, LeBoeuf RC, Bornfeldt KE (2007) Do glucose and lipids exert independent effects on atherosclerotic lesion initiation or progression to advanced plaques? Circ Res 100:769–781
Berthezene F (1996) Non-insulin dependent diabetes and reverse cholesterol transport. Atherosclerosis 124 (Suppl):S39–S42
Brewer HB Jr, Remaley AT, Neufeld EB, Basso F, Joyce C (2004) Regulation of plasma high-density lipoprotein levels by the ABCA1 transporter and the emerging role of high-density lipoprotein in the treatment of cardiovascular disease. Arterioscler Thromb Vasc Biol 24:1755–1760
Oram JF, Lawn RM (2001) ABCA1: the gatekeeper for eliminating excess tissue cholesterol. J Lipid Res 42:1173–1179
Wang Y, Oram JF (2002) Unsaturated fatty acids inhibit cholesterol efflux from macrophages by increasing degradation of ATP-binding cassette transporter A1. J Biol Chem 277:5692–5697
Albrecht C, Simon-Vermot I, Elliott JIJ, Higgins CF, Johnston DG, Valabhji J (2004) Leukocyte ABCA1 gene expression is associated with fasting glucose concentration in normoglycemic men. Metabolism 53:17–21
Passarelli M, Tang C, McDonald TO et al (2005) Advanced glycation end product precursors impair ABCA1-dependent cholesterol removal from cells. Diabetes 54:2198–2205
Hermo R, Mier C, Mazzotta M, Tsuji M, Kimura S, Gugliucci A (2005) Circulating levels of nitrated apolipoprotein A-I are increased in type 2 diabetic patients. Clin Chem Lab Med 43:601–606
Rashduni DL, Rifici VA, Schneider SH, Khachadurian AK (1999) Glycation of high-density lipoprotein does not increase its susceptibility to oxidation or diminish its cholesterol efflux capacity. Metabolism 48:139–143
Duell PB, Oram JF, Bierman EL (1990) Nonenzymatic glycosylation of HDL resulting in inhibition of high-affinity binding to cultured human fibroblasts. Diabetes 39:1257–1263
Duell PB, Oram JF, Bierman EL (1991) Nonenzymatic glycosylation of HDL and impaired HDL-receptor-mediated cholesterol efflux. Diabetes 40:377–384
Escher G, Hoang A, Georges S et al (2005) Demethylation using the epigenetic modifier, 5-azacytidine, increases the efficiency of transient transfection of macrophages. J Lipid Res 46:356–365
Woollard KJ, Phillips DC, Griffiths HR (2002) Direct modulatory effect of C-reactive protein on primary human monocyte adhesion to human endothelial cells. Clin Exp Immunol 130:256–262
Morrison JR, Fidge NH, Grego B (1990) Studies on the formation, separation, and characterization of cyanogen bromide fragments of human AI apolipoprotein. Anal Biochem 186:145–152
Sviridov D, Pyle L, Fidge N (1996) Efflux of cellular cholesterol and phospholipid to apolipoprotein A-I mutants. J Biol Chem 271:33277–33283
Baynes JW, Thorpe SR (1999) Role of oxidative stress in diabetic complications: a new perspective on an old paradigm. Diabetes 48:1–9
McLellan AC, Thornalley PJ, Benn J, Sonksen PH (1994) Glyoxalase system in clinical diabetes mellitus and correlation with diabetic complications. Clin Sci (Lond) 87:21–29
Sviridov D, Hoang A, Huang W, Sasaki J (2002) Structure-function studies of apoA-I variants: site-directed mutagenesis and natural mutations. J Lipid Res 43:1283–1292
Sviridov D, Fidge N (1995) Efflux of intracellular vs plasma membrane cholesterol in HepG2 cells: different availability and regulation by apolipoprotein A-I. J Lipid Res 36:1887–1896
Yamauchi Y, Abe-Dohmae S, Yokoyama S (2002) Differential regulation of apolipoprotein A-I/ATP binding cassette transporter A1-mediated cholesterol and phospholipid release. Biochim Biophys Acta 1585:1–10
Forbes JM, Thallas V, Thomas MC et al (2003) The breakdown of preexisting advanced glycation end products is associated with reduced renal fibrosis in experimental diabetes. FASEB J 17:1762–1764
Brownlee M, Vlassara H, Kooney A, Ulrich P, Cerami A (1986) Aminoguanidine prevents diabetes-induced arterial wall protein cross-linking. Science 232:1629–1632
Remaley AT, Stonik JA, Demosky SJ et al (2001) Apolipoprotein specificity for lipid efflux by the human ABCAI transporter. Biochem Biophys Res Commun 280:818–823
Chirinos JA, Zambrano JP, Chakko S et al (2005) Ability of serum to decrease cellular AcylCoA:cholesterol acyl transferase activity predicts cardiovascular outcomes. Circulation 112:2446–2453
Wang N, Chen W, Linsel-Nitschke P et al (2003) A PEST sequence in ABCA1 regulates degradation by calpain protease and stabilization of ABCA1 by apoA-I. J Clin Invest 111:99–107
Martinez LO, Agerholm-Larsen B, Wang N, Chen W, Tall AR (2003) Phosphorylation of a pest sequence in ABCA1 promotes calpain degradation and is reversed by ApoA-I. J Biol Chem 278:37368–37374
Barter PJ, Nicholls S, Rye K-A, Anantharamaiah GM, Navab M, Fogelman AM (2004) Antiinflammatory properties of HDL. Circ Res 95:764–772
Forbes JM, Thallas-Bonke V, Cooper ME, Thomas MC (2004) Advanced glycation: how are we progressing to combat this web of sugar anomalies in diabetic nephropathy. Curr Pharm Des 10:3361–3372
Kilhovd BK, Juutilainen A, Lehto S et al (2005) High serum levels of advanced glycation end products predict increased coronary heart disease mortality in nondiabetic women but not in nondiabetic men: a population-based 18-year follow-up study. Arterioscler Thromb Vasc Biol 25:815–820
Thomas MC, Tsalamandris C, MacIsaac R et al (2004) Low-molecular-weight AGEs are associated with GFR and anemia in patients with type 2 diabetes. Kidney Int 66:1167–1172
Cai W, He JC, Zhu L et al (2004) High levels of dietary advanced glycation end products transform low-density lipoprotein into a potent redox-sensitive mitogen-activated protein kinase stimulant in diabetic patients. Circulation 110:285–291
Beauchamp M-C, Michaud S-E, Li L, Sartippour MR, Renier G (2004) Advanced glycation end products potentiate the stimulatory effect of glucose on macrophage lipoprotein lipase expression. J Lipid Res 45:1749–1757
Ohgami N, Nagai R, Miyazaki A et al (2001) Scavenger receptor class B type I-mediated reverse cholesterol transport is inhibited by advanced glycation end products. J Biol Chem 276:13348–13355
Horiuchi S, Araki N, Morino Y (1991) Immunochemical approach to characterize advanced glycation end products of the Maillard reaction. Evidence for the presence of a common structure. J Biol Chem 266:7329–7332
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Garner B, Witting PK, Waldeck AR, Christison JK, Raftery M, Stocker R (1998) Oxidation of high density lipoproteins. I. Formation of methionine sulfoxide in apolipoproteins AI and AII is an early event that accompanies lipid peroxidation and can be enhanced by α-tocopherol. J Biol Chem 273:6080–6087
Nofer J-R, Walter M, Kehrel B et al (1998) HDL(3)-mediated inhibition of thrombin-induced platelet aggregation and fibrinogen binding occurs via decreased production of phosphoinositide-derived second messengers 1,2-diacylglycerol and inositol 1,4,5-tris-phosphate. Arterioscler Thromb Vasc Biol 18:861–869
Brubaker G, Peng DQ, Somerlot B, Abdollahian DJ, Smith JD (2006) Apolipoprotein A-I lysine modification: effects on helical content, lipid binding and cholesterol acceptor activity. Biochim Biophys Acta 1761:64–72
Moore RE, Navab M, Millar JS et al (2005) Increased atherosclerosis in mice lacking apolipoprotein A-I attributable to both impaired reverse cholesterol transport and increased inflammation. Circ Res 97:763–771
Shao B, Bergt C, Fu X et al (2005) Tyrosine 192 in apolipoprotein A-I is the major site of nitration and chlorination by myeloperoxidase, but only chlorination markedly impairs ABCA1-dependent cholesterol transport. J Biol Chem 280:5983–5993
Shao B, Oda MN, Bergt C et al (2006) Myeloperoxidase impairs ABCA1-dependent cholesterol efflux through methionine oxidation and site-specific tyrosine chlorination of apolipoprotein A-I. J Biol Chem 281:9001–9004
Forbes JM, Yee LT, Thallas V et al (2004) Advanced glycation end product interventions reduce diabetes-accelerated atherosclerosis. Diabetes 53:1813–1823
Acknowledgements
We are grateful to A. Remaley for the ABCA1 and ABCG1 plasmids. This study was supported by a grant from the Diabetes Australia Research Trust (D. Sviridov, R. O’Brien) and from the Juvenile Diabetes Research Foundation (J. M. Forbes, M. T. Coughlan, M. C. Thomas). D. Sviridov and J. P. F. Chin-Dusting are fellows of the National Health and Medical Research Council of Australia.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoang, A., Murphy, A.J., Coughlan, M.T. et al. Advanced glycation of apolipoprotein A-I impairs its anti-atherogenic properties. Diabetologia 50, 1770–1779 (2007). https://doi.org/10.1007/s00125-007-0718-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0718-9