Abstract
Introduction
People with mental disorders experience discrimination as a consequence of stigmatising attitudes that are largely socio-culturally constructed. Thus, there is a need to understand local contexts in order to develop effective programs to change such attitudes. We undertook a mental health literacy survey in rural Maharashtra, India, prior to developing a mental health training program for village health workers (VHWs) in a primary health care setting.
Methods
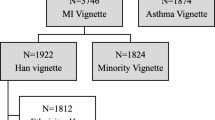
A cross-sectional mental health literacy survey was undertaken in late 2007, which involved interviewer-administration of a questionnaire to 240 systematically sampled community members, and 60 purposively sampled VHWs. Participants were presented with two vignettes describing people experiencing symptoms of mental disorders (depression, psychosis), and were asked about attitudes towards, and desired social distance from, the people in the vignettes (the latter being a proxy measure for stigma). Linear regression modelling was undertaken to identify predictors of social distance.
Results
Although the community was relatively accepting of people with mental disorders, false beliefs and negative attitudes were still evident. Desired social distance was consistently greater for the person depicted in the psychosis vignette compared to the depression vignette. For both vignettes, the main predictor of greater social distance was perceiving the person as dangerous, and the predictors of reduced social distance were being a VHW, and seeing the problem as a sign of personal weakness. For depression, believing the cause to be family tensions also reduced social distance. For psychosis, labelling the disorder as a mind/brain problem, and believing the cause to be lack of control over life or genetic factors increased social distance. The vast majority did not agree that the problems experienced in the vignettes were ‘a real medical illness’.
Conclusion
Promoting bio-medical explanations for mental disorders in this setting may exacerbate discriminatory attitudes. Provision of contextually relevant mental health training for the VHWs so that they are able to communicate, model and shape more positive attitudes is the next step.

Similar content being viewed by others
References
Link BG, Phelan JC (2001) Conceptualising stigma. Annu Rev Sociol 27:363–385
Corrigan PW, Watson AC (2002) Understanding the impact of stigma on people with mental disorder. World Psychiatry 1:16–20
Corrigan PW, Edwards AB, Green A, Diwan SL, Penn DL (2001) Prejudice, social distance, and familiarity with mental disorder. Schizophr Bull 27:219–225
Corrigan P (2004) How stigma interferes with mental health care. Am Psychol 59:614–625
Sayce L (1998) Stigma, discrimination and social exclusion: what’s in a word? J Mental Health 7:331–344
Hinshaw SP, Stier A (2008) Stigma as related to mental disorders. Annu Rev Clin Psychol 4:367–393
Baumann AE (2007) Stigmatization, social distance and exclusion because of mental disorder: the individual with mental disorder as a ‘stranger’. Int Rev Psychiatry 19:131–135
Link BG, Yang LH, Phelan JC, Collins PY (2004) Measuring mental disorder stigma. Schizophr Bull 30:511–541
Angermeyer MC, Matschinger H (2003) Public beliefs about schizophrenia and depression: similarities and differences. Soc Psychiatry Psychiatr Epidemiol 38:526–534
Angermeyer MC, Dietrich S (2006) Public beliefs about and attitudes towards people with mental disorder: a review of population studies. Acta Psychiatr Scand 113:163–179
Griffiths KM, Nakane Y, Christensen H, Yoshioka K, Jorm AF, Nakane H (2006) Stigma in response to mental disorders: a comparison of Australia and Japan. BMC Psychiatry 6:21
Marie D, Miles B (2008) Social distance and perceived dangerousness across four diagnostic categories of mental disorder. Aust NZ J Psychiatry 42:126–133
Martin JK, Pescosolido BA, Tuch SA (2000) Of fear and loathing: the role of ‘disturbing behaviour’, labels, and causal attribution in shaping public attitudes toward people with mental disorder. J Health Soc Behav 41:208–223
Bag B, Yilmaz S, Kirpinar I (2006) Factors influencing social distance from people with schizophrenia. Int J Clin Pract 60:289–294
Grausgruber A, Meise U, Katschnig H, Schony W, Fleischhacker WW (2007) Patterns of social distance towards people suffering from schizophrenia in Austria: a comparison between the general public, relatives and mental health staff. Acta Psychiatr Scand 115:310–319
Jorm AF, Griffiths KM (2008) The public’s stigmatizing attitudes towards people with mental disorders: how important are bio-medical conceptualizations? Acta Psychiatr Scand 118:315–321
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, White K, Kubiak MA (2002) Challenging two mental disorder stigmas: personal responsibility and dangerousness. Schizophr Bull 28:293–309
Angermeyer MC, Matschinger H (2003) The stigma of mental disorder: effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr Scand 108:304–309
Read J, Haslam M, Sayce L, Davies E (2006) Prejudice and schizophrenia: a review of the ‘mental disorder is a disorder like any other’ approach. Acta Psychiatr Scand 114:303–318
Alexander LA, Link BG (2003) The impact of contact on stigmatising attitudes toward people with mental disorder. J Mental Health 12:271–289
Adewuya AO, Makanjuola R (2008) Social distance towards people with mental disorder in southwestern Nigeria. Aust NZ J Psychiatry 42:389–395
Dietrich S, Beck M, Bujantugs B, Kenzine D, Matschinger H, Angermeyer MC (2004) The relationship between public causal beliefs and social distance toward mentally ill people. Aust NZ J Psychiatry 38:348–354
Angermeyer MC, Buyantugs L, Kenzine DV, Matschinger H (2004) Effects of labelling on public attitudes towards people with schizophrenia: are there cultural differences? Acta Psychiatr Scand 109:420–425
Shibre T, Negash A, Kullgren G, Kebede D, Alem A, Fekadu D, Medhin G, Jacobsson L (2001) Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol 36:299–303
Coker EM (2005) Selfhood and social distance: toward a cultural understanding of psychiatric stigma in Egypt. Soc Sci Med 61:920–930
Weiss MG, Ramakrishna J, Somma D (2006) Health-related stigma: rethinking concepts and interventions. Psychol Health Med 11:277–287
Bhugra D (2006) Severe mental disorder across cultures. Acta Psychiatr Scand 113(Suppl 429):17–23
Yang LH (2007) Application of mental disorder stigma theory to Chinese societies: synthesis and new directions. Singap Med J 48:977–985
Raguram R, Weiss MG, Channabasavanna SM, Devins GM (1996) Stigma, depression, and somatisation in South India. Am J Psychiatry 153:1043–1049
Thara R, Srinivasan TN (2000) How stigmatising is schizophrenia in India? Int J Soc Psychiatry 46:135–141
Chowdhury AN, Sanyal D, Bhattacharya A, Dutta SK, De R, Banerjee S, Bhattacharya K, Palit S, Bhattacharya P, Mondal RK, Weiss MG (2001) Prominence of symptoms and level of stigma among depressed patients in Calcutta. J Indian Med Assoc 99:20–23
Weiss MG, Jadhav S, Raguram R, Vounatsou P, Littlewood R (2001) Psychiatric stigma across cultures: local validation in Bangalore and London. Anthropol Med 8:71–87
Charles H, Manoranjitham SD, Jacob KS (2007) Stigma and explanatory models among people with schizophrenia and their relatives in Vellore, South India. Int J Soc Psychiatry 53:325
WHO, WONCA (2008) Integrating mental health into primary care: a global perspective. World Health Organization, World Organization of Family Doctors (WONCA), Geneva
Kermode M, Herrman H, Arole R, White J, Premkumar R, Patel V (2007) Empowerment of women as a strategy for mental health promotion in developing countries: a qualitative study from rural Maharashtra. BMC Public Health 7:225
Jorm A, Oh E (2009) Desire for social distance from people with mental disorders: a review. Aust NZ J Psychiatry 43:183–200
Vijayakumar L (2005) Suicide and mental disorders in Asia. Int Rev Psychiatry 17:109–114
Acknowledgments
We thank the following people for their contributions to this study: Dr. Raj Arole for having the vision to incorporate mental health into primary health care; Mr. Ravi Arole for data management; Dr. Kaustubh Joag for technical advice; Professor Helen Herrman for support and encouragement; Mrs Ratna Kamble, Ms Shainaj Khudbuddin Sayyad and Ms Shobha Kulkarni for data collection; and Dr. Ramaswamy Premkumar for assistance with sampling. This study was made possible through the award to Michelle Kermode of an Early Career Research grant from the University of Melbourne.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kermode, M., Bowen, K., Arole, S. et al. Attitudes to people with mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Soc Psychiat Epidemiol 44, 1087–1096 (2009). https://doi.org/10.1007/s00127-009-0031-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-009-0031-7