Abstract
Objective
To compare the effectiveness of open and closed endotracheal suction in recovering thin and thick secretions in normal and injured lungs during conventional and high frequency ventilation.
Design and setting
Randomised study in a paediatric intensive care model in the animal research laboratory of a tertiary paediatric hospital.
Subjects
16 New Zealand White rabbits.
Interventions
Anaesthetised animals were intubated with a 3.5-mm endotracheal tube. Simulated thin and thick secretions (iopamidol 2 ml, a watery radio-opaque fluid, and fluorescent mucin 1 ml) were instilled in turn 1 cm below the tube tip through a catheter placed via a tracheostomy. Open or closed suction, randomly assigned, was applied for 6 s at −140 mmHg using a 6-F gauge catheter. Following lung injury with repeated saline lavage the procedure was repeated on conventional and high frequency ventilation.
Measurements and results
Iopamidol recovery was determined by digitally subtracting the post-contrast and post-suction radiographic images. Mucin recovery was determined by fluorescence assay of the aspirate. In the normal lung similar amounts were recovered by both suction methods. In the lavaged lung closed suction recovered less iopamidol during conventional (22 ± 7.5%) and high frequency ventilation (11 ± 2.4%) than open suction (36 ± 12% and 22 ± 8.1%, respectively). Mucin recovery was less with closed suction during conventional (32 ± 28 μl) and high frequency ventilation (30 ± 31 μl) than with open suction (382 ± 235 μl and 241 ± 153 μl).
Conclusions
In the injured lung closed suction was less effective than open suction at recovering thin and thick simulated secretions, irrespective of ventilation mode.
Similar content being viewed by others
Introduction
Mechanically ventilated patients require endotracheal suction periodically to prevent partial or complete endotracheal tube (ETT) obstruction, lobar collapse, atelectasis and increased work of breathing [1–3]. However, suctioning is associated with significant complications, including hypoxaemia, cardiovascular instability and changes in cerebral blood volume [4–10], which are partially attributed to disconnection of the ventilator circuit during open suction. Closed suction, performed without breaking the circuit, has been shown to ameliorate complications [3, 5, 11–13] and consequently is commonly used. There are concerns, however, that closed suction is less effective than open in removing secretions [14–19]. These concerns were supported by an in vitro study in which closed suction recovered less material than open suction [20]. Two in vivo studies comparing secretion recovery with open and closed suction in adult patients showed mixed results [21, 22] but are difficult to interpret due to methodological problems [23]. No studies relevant to children or infants have been found. Closed suction has not been studied with high-frequency oscillatory ventilation (HFOV), although its use is recommended [24, 25].
The aim of this study was to compare the effectiveness of open and closed suction, using equipment appropriate for paediatric patients, in recovering thin and thick secretions from the tracheobronchial tree in: (a) the normal lung, (b) the injured lung during conventional ventilation, (c) the injured lung during HFOV. Based on the in vitro findings of Lindgren et al. [20], we hypothesised that closed suction would be less effective at removing secretions in all situations.
Materials and methods
Preparation of tracer materials
Thin secretions were simulated using iopamidol, a watery radio-opaque fluid (Isovue 370, Regional Health Care Products, Rosebery, Australia), diluted 1:1 with 0.9% saline. Thick secretions were simulated using fluorescent mucin, prepared by vortex-mixing 240 mg bovine submaxillary gland mucin (cat. no. M3895, Sigma Chemical, Castle Hill, Australia) and 0.5 mg fluorescein (Minims, North Ryde, Australia) in 4 ml saline. To enable cineradiographic tracking 1.5 ml iopamidol was added. Final concentrations of mucin and fluorescein were approx. 50 mg/ml and 0.11 mg/ml, respectively. The mixture was cooled to 4 °C. Reconstituted mucin has been noted to retain its non-Newtonian properties at concentrations of 20 mg/ml or higher [26].
Preparation of animals
The experiments complied with Australian National Health and Medical Research Council guidelines, and the study protocol was approved by our institution's animal ethics committee. Adult female New Zealand white rabbits (n = 16) were premedicated with 2 mg/kg xylazine intramuscularly, and arterial and venous cannulae were sited. Anaesthesia was induced with 30 mg/kg thiopentone and 10 mg/kg xylazine intravenously and was maintained with a thiopentone infusion at 60–90 mg/kg per hour. The animals were muscle-relaxed with 0.1 mg/kg pancuronium followed by an infusion at 0.24 mg/kg per hour. A 3.5-mm uncuffed ETT was inserted via a tracheostomy to the mid-trachea at the level of the third thoracic vertebral body and secured with nylon ties. Two 15-cm narrow gauge catheters were inserted via the tracheostomy alongside the ETT and advanced to 1 cm beyond its tip for instillation of the iopamidol and mucin. The position of the ETT and dispensing catheters was confirmed with fluoroscopy.
Time-cycled pressure-limited ventilation (TCPLV) was commenced (Infant Star 500, Nellcor Puritan Bennett, Pleasanton Calif., USA) and a pneumotachograph (Florian respiratory monitor, Acutronic Medical Systems, Zug, Switzerland) placed in the circuit to monitor tidal volumes. Initial ventilator settings were: rate 30/min, inspiratory time 0.4 s, positive end-expiratory pressure 4 cmH2O, and peak pressure (PIP) adjusted to maintain tidal volumes at 6 ml/kg. The inspired fraction of oxygen was maintained at 1.0 throughout.
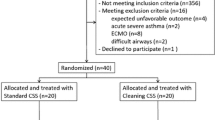
Suction protocol
Each animal was randomised to one of two groups to receive the suctioning schedule detailed in Table 1. Only one episode of suction with each tracer material was performed in each experimental phase, thus avoiding contamination of suction return fluid with material from the previous episode. All residual tracer was removed from the lung after each phase with large volume saline lavage, and its clearance verified by fluoroscopy. Closed suction was performed using a 6-F gauge (external diameter 2 mm) Ballard Trachcare in-line catheter (Kimberly-Clark, Roswell, Ga., USA), and open suction using a 6-F disposable catheter (Mallinckrodt, Rowville, Victoria, Australia). The number and size of the holes is the same in both catheters. In both techniques a pre-measured catheter was inserted, without applying suction, to the ETT tip. When in place, suction was applied at a pressure of −140 mmHg (19 kPa) for 6 s while simultaneously withdrawing the catheter. This suction pressure is used widely for term newborns in Australia [27]. All suction episodes were conducted by the same investigator. A second investigator disconnected the ventilator circuit (for open suction) supported the ETT during the procedure and timed the duration of suction. Baseline characteristics of the animals prior to each experimental phase are shown in Table 2; no differences were noted between the two groups of animals except that those in group A had a higher alveolar-arterial oxygen difference (AaDO2) and mean airway pressure (Paw) before instillation of mucin in phase 1 than those in group B.
Fluoroscopic image acquisition
Image-intensified chest fluoroscopy (Diasonics OEC 9400 mobil C-Arm X-ray system, OEC-Diasonics, Salt Lake City, Utah, USA) was performed throughout each suctioning episode at standardised settings depending on the subject's weight (range 52–57 kV, 1.2–1.7 mA). Images were acquired from 10 s prior to instillation of each tracer material and continued until five inflations (TCPLV) or 10 s (HFOV) after completion of suction. The raw fluoroscopy signals were digitised and stored as uncompressed Microsoft.avi files at 25 frames per second (24 bits, 720 × 576) using Ulead Video Studio 5.0 (Ulead systems, Taipei, Taiwan) (see Electronic Supplementary Material, ESM).
Experimental procedure
Each experiment was conducted in three phases: with a normal lung (phase 1), with a lavaged lung during TCPLV (phase 2), and with a lavaged lung during HFOV (phase 3). In phase 1 the ventilator was switched to continuous positive airways pressure (CPAP) at 4 cmH2O. Diluted iopamidol (2 ml) was instilled into the trachea via one dispensing catheter, and suction applied immediately. Ventilation was recommenced. The ventilator was switched to CPAP as before, and 1 ml fluorescent mucin was instilled via the primed dispensing catheter. The suction procedure was repeated, and the recovered material collected. Any residual mucin in the catheter was recovered by suctioning 4 ml saline through the catheter into the same container. The volume in the container was adjusted to 10 ml using saline.
On completion of phase 1, lung injury was induced by repeated saline lavage until the AaDO2 was 400 mmHg or higher. Suctioning of lavage fluid was performed while simultaneously squeezing the chest and continued until no more fluid was obtained. The suction episodes were then repeated in the lavaged lung (phase 2), at a CPAP of 6 cmH2O. Further saline lavages were performed to remove residual tracer materials. HFOV was commenced (3100A high-frequency oscillator, Sensormedics, Yorba Linda, Calif., USA) at a frequency of 10 Hz, amplitude 1.5 times the PIP on TCPLV and the Paw adjusted to maintain peripheral oxygen saturation above 95%. When the animal was stabilised, the suction episodes were repeated (phase 3); HFOV continued unchanged throughout this phase. At the completion of the experiment the animal was killed.
Measurement of iopamidol recovery
From the digitised fluoroscopy of each suction episode three bitmap still images (300 dpi) were taken at end-expiration: (a) during the last inflation before instillation of iopamidol (baseline image), (b) after iopamidol instillation and immediately before suction (pre-suction image), and (c) following suction and after either five conventional inflations or 10 s of HFOV (post-suction image). These images were phase-matched using frame-by-frame inspection. For each trio of images an identical cropped template was created to outline the lung fields using a pixel grid (Adobe Photoshop version 5.5, Adobe Systems, San Jose, Calif., USA; Fig. 1a–c). Constant background was removed by subtracting the baseline image, resulting in greyscale images representing the amount of contrast instilled (Fig. 1d), and the amount remaining after suction (Fig. 1e). Subtraction of e from d produced an image of the recovered iopamidol (Fig. 1f), in which individual pixels were scored based on their greyscale value (black = 0, white = 765). Iopamidol recovery was defined as the cumulative pixel score of this final image, and was expressed as a percentage of the pre-suction pixel score.
Measurement of iopamidol recovery. a–c Cropped still images taken from digital video recording of a representative episode of open suction (animal no.13) in the normal lung state. a Baseline image taken immediately prior to instillation of iopamidol. b Pre-suction image after instillation of iopamidol. c Post-suction image. d–f Subtraction images showing amount of iopamidol present before (d) and after (e) suction and the amount recovered by suction (f). d Pre-suction image minus baseline image (i.e. b minus a). e Post-suction image minus baseline image (i. e. c minus a). f d minus e. Cumulative pixel score of f (546,210) divided by d (1,689,120), gives value for iopamidol recovery of 32%
Measurement of mucin recovery
Fluorescence in the recovered fluid samples was measured with a fluorimeter (Model LS-3B fluorescence spectrophotometer, Perkin-Elmer, Shelton, Conn., USA), using an excitation wavelength of 490 nm and emission wavelength of 514 nm. Fluorescence was zeroed against normal saline. For each sample mucin recovery was calculated from the measured fluorescence value by reference to a standard containing 50 μl fluorescent mucin in a total volume of 10 ml. In preliminary experiments using serial dilutions of this standard, fluorescence was noted to be linearly related to fluorescent mucin concentration up to 100-fold dilution.
Statistical analysis
Recovery of iopamidol and mucin by open and closed suction in each experimental phase was compared using the unpaired t test with correction for unequal variances. Difference in recovery between experimental phases with each technique was determined using one-way analysis of variance, with Bonferroni's post hoc multiple-comparison tests. For all comparisons p < 0.05 was considered statistically significant. Statistical analysis was performed using Stata (version 8.0, Stata, College Station, Tex, USA).
Results
The recovery of both iopamidol and mucin from each suctioning episode is shown in Fig. 2. There was wide variation in recovery of iopamidol with both suction methods, and in that of mucin with open suction. Iopamidol recovery in the normal lung did not differ significantly between open and closed suction. In the lavaged lung recovery with open suction was significantly greater than with closed during both TCPLV (p = 0.014) and HFOV (p = 0.012). Similar results were obtained for mucin recovery. There was no significant difference in the normal lung, while in the lavaged lung open suction recovered more than closed during TCPLV (p = 0.0075) and HFOV (p = 0.019). The fluoroscopy recordings of open suction episodes showed both tracer materials effluxing into the trachea and ETT on disconnection from ventilation prior to the application of suction (see ESM).
Recovery of tracer materials in each phase of the study. Diamonds open suction; circles closed suction; horizontal bars means; n < 8 in some categories due to missing data. TCPLV Time-cycled pressure-limited ventilation; HFOV high-frequency oscillatory ventilation. a Percentage of iopamidol recovered. Normal lung: recovery with open suction (n = 8) 24 ± 7.8%, closed suction (n = 8) 18 ± 7.3% (p = 0.115). Lavaged lung during TCPLV: recovery with open suction (n = 8) 36 ± 12%, closed suction (n = 8) 22 ± 7.5% (p = 0.014). Lavaged lung during HFOV: recovery with open suction (n = 7) 22 ± 8.1%, closed (n = 6) 11 ± 2.4% (p = 0.012). b Amount of mucin recovered. Normal lung: recovery with open suction (n = 7) 77 ± 61 μl, closed suction (n = 7) 28 ± 24 μl (p = 0.08). Lavaged lung during TCPLV: recovery with open suction (n = 7) 382 ± 235 μl, closed suction (n = 7) 32 ± 28 μl (p = 0.0075). Lavaged lung during HFOV: recovery with open suction (n = 6) 241 ± 153 μl, closed suction (n = 6) 30 ± 31 μl (p = 0.019)
Iopamidol recovery with open suction differed between experimental phases (p = 0.013, analysis of variance), with a greater recovery in the lavaged lung during TCPLV than in either of the other phases. There was also a difference in iopamidol recovery with closed suction (p = 0.017), with less obtained in the lavaged lung during HFOV than in the lavaged lung during TCPLV. Mucin recovery with open suction also differed between the three experimental phases (p = 0.011), with more obtained in the lavaged lung during TCPLV than the normal lung. There was no difference between phases in mucin recovery with closed suction.
In an attempt to explain within-group variations in recovery of tracer materials a post hoc analysis of correlations between recovery and markers of lung injury was performed using linear regression. No significant correlations were found between iopamidol or mucin recovery and AaDO2 or PaCO2 during any phase. Mucin recovery with open suction was positively correlated with PIP in phase 2 (R2 = 0.92, p = 0.0007) but not phase 1. There were no associations between PIP and either iopamidol recovery, or mucin recovery with closed suction. Pooled data from all animals in phase 3 showed a moderate correlation between mucin recovery and Paw in the lavaged lung on HFOV (R2 = 0.44, p = 0.018). The correlation was not statistically significant when open and closed suction groups were analysed separately. Iopamidol recovery was associated with Paw on HFOV in the closed suction group (R2 = 0.80, p = 0.016), while in the open suction group the association was of borderline significance (R2 = 0.56, p = 0.052).
Discussion
This study compared the effectiveness of open and closed suction in recovering simulated thin and thick secretions from the tracheobronchial tree in the normal lung and in the lavaged lung during TCPLV and HFOV. We found closed suction recovered significantly less of both materials in the lavaged lung during both ventilation modes, with a non-significant trend in the normal lung.
These findings support nurses' subjective assessments of the relative ineffectiveness of closed suction [14–19] and complement the in vitro data of Lindgren et al. [20] which demonstrated closed suction to recover significantly less soap gel from an artificial trachea than open suction. In addition to providing a more representative physiological model, our in vivo experiment enabled comparison of secretion recovery in different lung states, a study that to our knowledge has not previously been undertaken. Two studies have compared the effectiveness of open and closed suction in ventilated adults. Witmer et al. [21] studied 25 patients with a wide range of diagnoses and found no difference in the wet weight of secretions obtained by the two methods. In contrast, Lasocki et al. [22] found that open suction recovered significantly more secretions than closed in nine patients with acute lung injury. However, measurement of secretions obtained in the clinical setting may be unreliable due to the accumulation of condensed water (and hence increased wet weight) in closed suction catheters [23]. Moreover, clinical comparisons of different suction methods assume that the same volume of secretion is present at each suctioning episode; the amount of secretion remaining in the airway after suction is unknown. By using known amounts of tracer materials to simulate secretions our study overcame these problems as we were able to measure the proportional recovery of the specific materials uncontaminated by other substances and thus the relative effectiveness of suctioning.
Lindgren et al. [20] proposed two mechanisms whereby open suction recovers more secretions than closed: (a) that during closed suction secretions are pushed away from the catheter tip during inflation, and (b) that gas aspirated from the lung during open suction moves secretions toward the catheter. Our fluoroscopic videos showed that during open suction the tracer materials moved into the trachea and ETT immediately on disconnection from ventilation, before suction was applied. Studies of lung volume changes with open suction have shown that significant loss occurs on disconnection from the ventilator [28–31]. We suggest that this sudden loss of lung volume pushes secretions towards the suction catheter and is an additional mechanism for the increased effectiveness of open suction. We found significant differences between open and closed suction only in the lavaged lung, and there were some indications that secretion recovery was related to the degree of lung injury. Thus we hypothesise that this mechanism is more pronounced in the less compliant, diseased lung.
Recovery of tracer materials varied considerably between animals and between experimental phases. While there were some associations between recovery and the recorded markers of lung injury, these associations were insufficient to explain all the variation. Direct measurement of lung volume change and use of more specific markers of injury could clarify these relationships.
Previously, suctioning effectiveness has been studied either in adult patients [21, 22] or using equipment specific to adults (12- and 14-F suction catheters with 7.0 and 8.0 mm ETTs) [20]. By using 3.5 mm ETTs and 6-F catheters, our study has relevance to newborns. Our findings cannot be assumed to apply to adult patients; however, combined with those of other researchers [20, 22], they suggest that relative ineffectiveness of closed suction may affect patients of all ages.
This study is the first to investigate suction effectiveness during HFOV. We found closed suction recovered less of both materials than open suction. We also found that less iopamidol was recovered than during TCPLV, irrespective of suction technique. However, comparisons between the HFOV and TCPLV phases are limited by differences in the experimental protocol. During TCPLV in the lavaged lung, iopamidol was instilled while maintaining CPAP of 6 cmH2O; during HFOV Paw varied between 10 and 17 cmH2O on instillation. The higher pressure may have caused the watery iopamidol to disperse further into the lung and to be less accessible to removal by suction. There were no significant differences in recovery of mucin between TCPLV and HFOV. Dispersion of the thicker mucin may have been affected less by variations in airway pressure.
One limitation of our study is that closed suction during conventional ventilation was performed during ETT CPAP of 4 and 6 cmH2O. CPAP was used because pilot data showed the tracer materials dispersed widely into the lung during conventional ventilator inflations. In their in vitro experiment Lindgren et al. [20] found a difference in secretion recovery between open and closed suction with a CPAP of 10 but not one of 0 cmH2O. The lower distending pressure used in our study may have contributed to the lack of difference between suction techniques in the normal lung.
Anecdotal reports suggest that ineffective secretion clearance with closed suction is most likely to occur if secretions are thick, and some authors discourage its use in these circumstances [16, 18, 19]. Our finding of greater differences between open and closed suction with the thicker mucin than with the watery iopamidol would seem to support these reports and to reinforce recommendations for strategies (such as adequate patient hydration and humidification of inspired gases) to optimise the consistency of secretions [32, 33]. Nevertheless, our findings indicate that clearance even of thin secretions may be ineffective with closed suction. The effectiveness of open suction, on the other hand, is rarely questioned. We found a number of instances of poor recovery of both iopamidol and mucin with open suction, suggesting that secretion clearance with this method may not always be adequate.
Closed suction is widely used to reduce suctioning side effects. Studies in adults [14, 17, 28, 30, 34, 35], children [29] and neonates [3, 12] show closed suction results in less hypoxaemia and loss of lung volume than open suction. The clinical significance of these differences is unclear [14, 36], and the role of supplemental oxygen or recruitment manoeuvres is still to be determined [22, 37, 38]. Further research into prevention or management of these side effects is warranted. However, the sole reason for performing suction is to remove secretions, yet little is known of the effectiveness of various suction techniques. Our results indicate that if used under identical conditions, and at the settings employed in this study closed suction is less effective than open. Varying the conditions and settings may increase its effectiveness, and requires further investigation. Other suction variables that may contribute to efficacy should also be studied. Such data are essential for clinicians to choose the most appropriate suction method for individual patients.
Conclusions
In the injured lung closed suction appears to be less effective than open suction, irrespective of type of secretions or ventilation technique. We found no significant differences in the normal lung. Recovery of simulated secretions varied widely, particularly with open suction. Further research is required to identify the most effective endotracheal suction technique. Clinicians should be aware of the potential for secretion retention with closed suction.
References
Landa JF, Kwoka MA, Chapman GA, Brito M, Sackner MA (1980) Effects of suctioning on mucociliary transport. Chest 77:202–207
Guglielminotti J, Desmonts JM, Dureuil B (1998) Effects of tracheal suctioning on respiratory resistances in mechanically ventilated patients. Chest 113:1335–1338
Woodgate PG, Flenady V (2003) Tracheal suctioning without disconnection in intubated ventilated neonates (Cochrane Review). In: The Cochrane Library. Wiley, Chichester, UK
Brandstater B, Muallem M (1969) Atelectasis following tracheal suction in infants. Anesthesiology 31:468–473
Cabal L, Devaskar S, Siassi B, Plajstek C, Waffarn F, Blanco C, Hodgman J (1979) New endotracheal tube adaptor reducing cardiopulmonary effects of suctioning. Crit Care Med 7:552–555
Simbruner G, Coradello H, Fodor M, Havelec L, Lubec G, Pollak A (1981) Effect of tracheal suction on oxygenation, circulation, and lung mechanics in newborn infants. Arch Dis Child 56:326–330
Kerem E, Yatsiv I, Goitein KJ (1990) Effect of endotracheal suctioning on arterial blood gases in children. Intensive Care Med 16:95–99
Singh NC, Kissoon N, Frewen T, Tiffin N (1991) Physiological responses to endotracheal and oral suctioning in paediatric patients: the influence of endotracheal tube sizes and suction pressures. Clin Intensive Care 2:345–350
Shah AR, Kurth CD, Gwiazdowski SG, Chance B, Delivoria-Papadopoulos M (1992) Fluctuations in cerebral oxygenation and blood volume during endotracheal suctioning in premature infants. J Pediatr 120:769–774
Skov L, Ryding J, Pryds O, Greisen G (1992) Changes in cerebral oxygenation and cerebral blood volume during endotracheal suctioning in ventilated neonates. Acta Paediatr 81:389–393
Weidner I (2001) Closed endotracheal suction in pediatric and neonatal intensive care nursing. Kinderkrankenschwester 20:251–253
Kalyn A, Blatz S, Feuerstake S, Paes B, Bautista C (2003) Closed suctioning of intubated neonates maintains better physiologic stability: a randomized trial. J Perinatol 23:218–222
Tan AM, Gomez JM, Mathews J, Williams M, Paratz J, Rajadurai VS (2005) Closed versus partially ventilated endotracheal suction in extremely preterm neonates: physiologic consequences. Intensive Crit Care Nurs 21:234–242
Carlon GC, Fox SJ, Ackerman NJ (1987) Evaluation of a closed-tracheal suction system. Crit Care Med 15:522–525
Noll ML, Hix CD, Scott G (1990) Closed tracheal suction systems: effectiveness and nursing implications. AACN Clin Issues 1:318–328
Crimlisk J, Paris R, McGonagle E, Calcutt J, Farber H (1994) The closed tracheal suction system: implications for critical care nursing. Dimens Crit Care Nurs 13:292–300
DePew CL, Noll ML (1994) Inline closed-system suctioning: a research analysis. Dimens Crit Care Nurs 13:73–83
Blackwood B (1998) The practice and perception of intensive care staff using the closed suctioning system. J Adv Nurs 28:1020–1029
Glass C, Grap MJ, Sessler CN (1999) Endotracheal tube narrowing after closed-system suctioning: prevalence and risk factors. Am J Crit Care 8:93–100
Lindgren S, Almgren B, Hogman M, Lethvall S, Houltz E, Lundin S, Stenqvist O (2004) Effectiveness and side effects of closed and open suctioning: an experimental evaluation. Intensive Care Med 30:1630–1637
Witmer MT, Hess D, Simmons M (1991) An evaluation of the effectiveness of secretion removal with the Ballard closed-circuit suction catheter. Respir Care 36:844–848
Lasocki S, Lu Q, Sartorius A, Fouillat D, Remerand F, Rouby J (2006) Open and closed-circuit endotracheal suctioning in acute lung injury: efficiency and effects on gas exchange. Anesthesiology 104:39–47
Steuer JD, Stone KS, Nickel J, Steinfeld Y (2000) Methodologic issues associated with secretion weight as a dependent variable in research using closed-system suction catheters. Nurs Res 49:295–299
Higgins J, Estetter B, Holland D, Smith B, Derdak S (2005) High-frequency oscillatory ventilation in adults: Respiratory therapy issues. Crit Care Med 33:S196–S203
Sweeney A-M, Lyle J, Ferguson ND (2005) Nursing and infection-control issues during high-frequency oscillatory ventilation. Crit Care Med 33:S204–S208
List SJ, Findlay BP, Forstner GG, Forstner JF (1978) Enhancement of the viscosity of mucin by serum albumin. Biochemical Journal 175:565–571
Gordon MJ, Tingay DG, Johnston L, Copnell B (2006) Endotracheal suctioning practices of neonatal and paediatric intensive care nurses (abstract). Aust Crit Care 19:146
Cereda M, Villa F, Colombo E, Greco G, Nacoti M, Pesenti A (2001) Closed system endotracheal suctioning maintains lung volume during volume-controlled mechanical ventilation. Intensive Care Med 27:648–654
Choong K, Chatrkaw P, Frndova H, Cox PN (2003) Comparison of loss in lung volume with open versus in-line catheter endotracheal suctioning. Pediatr Crit Care Med 4:69–73
Maggiore SM, Lellouche F, Pigeot J, Taille S, Deye N, Durrmeyer X, Richard JC, Mancebo J, Lemaire F, Brochard L (2003) Prevention of endotracheal suctioning-induced alveolar derecruitment in acute lung injury. Am J Respir Crit Care Med 167:1215–1224
Tingay DG, Copnell B, Mills JF, Morley CJ, Dargaville PA (2007) Effects of open endotracheal suction on lung volume in infants receiving HFOV. Intensive Care Med 33:689–693
Williams R, Rankin N, Smith T, Galler D, Seakins P (1996) Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit Care Med 24:1920–1929
Blackwood B (1999) Normal saline instillation with endotracheal suctioning: primum non nocere (first do no harm). J Adv Nurs 29:928–934
Harshbarger SA, Hoffman LA, Zullo TG, Pinsky MR (1992) Effects of a closed tracheal suction system on ventilatory and cardiovascular parameters. Am J Crit Care 1:57–61
Lee CK, Ng KS, Tan SG, Ang R (2001) Effect of different endotracheal suctioning systems on cardiorespiratory parameters of ventilated patients. Ann Acad Med Singapore 30:239–244
Fernandez MDM, Piacentini E, Blanch L, Fernandez R (2004) Changes in lung volume with three systems of endotracheal suctioning with and without pre-oxygenation in patients with mild-to-moderate lung failure. Intensive Care Med 30:2210–2215
Paul-Allen J, Ostrow CL (2000) Survey of nursing practices with closed-system suctioning. Am J Crit Care 9:9–19
Demir F, Dramali A (2005) Requirement for 100% oxygen before and after closed suction. J Adv Nurs 51:245–251
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by a project grant from the Murdoch Childrens Research Institute and was supported in part by an Australian National Health and Medical Research Council Medical Postgraduate Research Scholarship (D.G.T.).
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Copnell, B., Tingay, D.G., Kiraly, N.J. et al. A comparison of the effectiveness of open and closed endotracheal suction. Intensive Care Med 33, 1655–1662 (2007). https://doi.org/10.1007/s00134-007-0635-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0635-x