Abstract
Purpose
To determine whether any of several quality improvement interventions with none specifically targeting methicillin-resistant Staphylococcus aureus (MRSA) were associated with a decline in endemic MRSA prevalence in an intensive care unit (ICU) where active screening and contact isolation precautions for known MRSA colonised patients are not practised.
Setting
Medical–surgical ICU with 2,000 admissions/year.
Design
8.5-year retrospective time-series analysis.
Interventions
ICU re-location, antibiotic stewardship utilising computerised decision-support and infectious-diseases physician rounds, dedicated ICU infection control practitioners, alcohol-based hand rub solution (ABHRS).
Method
Regression modelling was used to evaluate trends in S. aureus prevalence density (monthly clinical isolates per 1,000 patient-days), antibiotic consumption, infection control consumables, ABHRS and their temporal relationship with MRSA prevalence.
Results
Methicillin-resistant S. aureus prevalence density decreased by 83% [95% confidence interval (CI) −68% to −91%, p < 0.001]. Rates of MRSA bacteraemia decreased 89% (95% CI −79% to −94%, p = 0.001) with no statistically significant change in methicillin-sensitive S. aureus bacteraemia. Hospital MRSA prevalence density decreased 17% (95% CI −5% to −27%, p = 0.005), suggesting that ICU was not shifting MRSA elsewhere. In ICU, broad-spectrum antibiotic use decreased by 26% (95% CI −12% to −38%, p = 0.008), coinciding with a decrease in MRSA, but time-series analysis did not show a significant association. On multivariate analysis, only ABHRS was significantly associated with a decrease in MRSA, but it was formally introduced late in the study period when MRSA was already in decline.
Conclusion
General quality improvement measures were associated with a decrease in endemic MRSA in a high-risk setting without use of resource-intensive active surveillance and isolation practices.
Similar content being viewed by others
Introduction
The optimal strategy for control of methicillin-resistant Staphylococcus aureus (MRSA) in endemic settings is unresolved. The “search and destroy” approach involving screening, contact isolation precautions and decolonisation used successfully in low-prevalence settings may not be practical in settings of high endemicity. Active surveillance cultures (ASC) aim to identify the asymptomatic reservoir of colonised patients, in order to interrupt person-to-person transmission, thereby preventing new acquisition which is associated with subsequent disease [1]. The intensive care unit (ICU) may serve as a “hub” for MRSA acquisition and dissemination [2], yet studies with ICU-based MRSA control efforts have had mixed results, including lack of benefit from isolation in single rooms or cohorts [3], disappointing results with ICU compared with hospital admission screening [4], success with screening using conventional cultures [5] but limited benefit using rapid molecular tests unless also combined with pre-emptive isolation [6]. Recently, controlled studies in non-ICU areas have not conclusively demonstrated a benefit of ASC in reducing nosocomial MRSA infection or acquisition rates [7, 8]. Accordingly, some professional societies have moderated their stance on the role of ASC for MRSA, suggesting a potential benefit only if basic infection control (IC) measures are failing [9].
Methicillin resistance rates in healthcare-associated S. aureus infection reached 64% in US ICUs in 2003 [10], 40% in European ICUs [11] and over 40% in the major hospitals of Eastern Australia [12]. Use of percentage MRSA as a surveillance metric may, however, mask important declining trends in MRSA incidence if the incidence of methicillin-sensitive S. aureus (MSSA) is decreasing as well [13]. Recently, several US states have reported declines in ICU MRSA central line-associated bloodstream infections (CLABSI) pre-dating mandatory reporting of healthcare-associated infections and ASC for MRSA, but the factors responsible remain unclear [13]. In our institution, ASC, routine contact isolation of MRSA colonised and infected patients and decolonisation therapies have never been adopted. Since 2000, several IC initiatives, with none specifically targeting MRSA, were introduced to our hospital. Pathogen data collected to monitor our antibiotic stewardship program showed a sustained decline in ICU MRSA prevalence over a prolonged period, prompting an investigation into the contributory factors. Using change-point analysis and autoregressive models we evaluated the impact of multiple IC interventions and aggregate antibiotic use on MRSA prevalence within ICU and the wider hospital.
Methods
Study design and setting
We undertook a retrospective time-series analysis assessing the impact of multiple quality improvement interventions, consumption of antibiotics and IC consumables on ICU MRSA prevalence from 1 January 2000 to 30 June 2008. Data prior to 2000 were unavailable.
The Royal Melbourne Hospital (RMH) is a 690-bed adult university-affiliated tertiary hospital with a 24-bed medical–surgical ICU comprising 6 single rooms and 18 open bays. ICU patient characteristics are presented in Table 1. The ICU has approximately 2,000 admissions per year, with a mean (median) length of stay of 4.1 (3.0) days in 2007 and 4.4 (3.0) days in 2000. Surgical patients including trauma, cardiothoracic, neurosurgery and general specialities comprise 70% of ICU admissions. In 2005, RMH became one of two statewide major trauma centres, with an annual increase in trauma admissions from a mean of 9.6% (2000–2004) to 17% in 2005. Throughout the study period, nurse-to-patient ratios were 1:1 and 1:2 for step-down care. A clinical microbiologist, two infectious diseases (ID) physicians and two infection control practitioners (ICPs) oversee ICU infection control. MRSA is endemic, but outbreaks did not occur. MRSA clonality is unknown, as genotyping is not routine. A point-prevalence survey in December 2005 showed that 6.9% of 288 patients (95% CI 4.3–10.5%) were MRSA colonised on ICU discharge.
Infection control procedures
For all patient contact in ICU, staff wear a single-use disposable plastic apron. Screening cultures for MRSA are not routine. MRSA colonised and infected patients, identified through clinical isolates, are cared for among the general ICU population without use of gowns, gloves or single-room isolation or cohorting. Decolonisation is not attempted. Use of alcohol-based hand rub solution (ABHRS) is RMH policy for hand disinfection.
From May 2007, ICU patients underwent screening for MRSA on admission, discharge and twice weekly as part of a separate research study. Results were available on the pathology system but were not directly communicated to ICU health-care workers (HCWs) and were not specifically acted upon.
Microbiology data
Monthly clinical isolates of S. aureus (excluding screening swabs and duplicates within 7 days from sterile and 30 days from non-sterile sites) from ICU and elsewhere in the hospital were electronically extracted from the microbiology database and expressed per 1,000 patient-days (prevalence density). Isolates obtained within the first 48 h of hospital admission were not excluded. S. aureus bloodstream isolates from ICU were separately analysed, as they unequivocally represented infection. Laboratory identification methods did not change over the study period.
Antibiotic consumption
Monthly quantities of antibiotics prescribed in ICU were obtained from pharmacy records and expressed as the number of defined daily doses (DDD) per 1,000 patient-days. These included third/fourth-generation cephalosporins, fluoroquinolones, carbapenems, anti-pseudomonal penicillins (ticarcillin–clavulanate, piperacillin–tazobactam), aminoglycosides, glycopeptides and macrolides. Broad-spectrum antibiotics comprised all antibiotic classes excluding glycopeptides (which specifically target MRSA) and macrolides, because erythromycin, the most frequently prescribed macrolide in our ICU, is used principally as an intestinal pro-kinetic agent.
Infection control consumables
Monthly quantities of IC consumables used in ICU were obtained from the purchasing department. These included medicated soap, gloves, plastic aprons, disposable gowns and alcohol-impregnated wipes expressed as numbers per 1,000 patient-days. Data on plastic aprons were missing from 1 July 2006 to 30 June 2007. Medicated soap and ABHRS usage was expressed as litres per 1,000 patient-days.
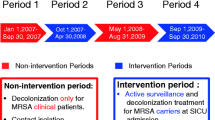
Interventions
An antibiotic stewardship program incorporating a computerised decision-support system (CDSS) to guide antibiotic prescribing, introduced to ICU (January 2001), was associated with significant decreases in total and broad-spectrum antibiotic usage in ICU [14]. A CDSS, implemented in non-ICU areas (January 2005), led to hospital-wide reductions in antibiotic consumption [15]. Mandatory statewide surveillance of ICU infections [CLABSI, ventilator-associated pneumonia (VAP)] began in 2002 [16]. Minocycline-impregnated vascular catheters were used throughout the study period. In April 2004, the ID service commenced twice-weekly ICU ward rounds.
An outbreak of non-multiresistant Acinetobacter (March 2004–November 2005) prompted the appointment in ICU of two full-time ICPs (November 2004), enabling 7-day cover. These senior ICU nurses led a series of interventions (reported elsewhere), achieving outbreak control [17]. Contact precautions (long-sleeved gowns and gloves) were instituted for non-primary HCWs of Acinetobacter colonised patients for 3 months from October 2005.
A 70% ethanol ABHRS, used in ICU from January 2000 to March 2004, was replaced by another product (61.5% ethanol) introduced in July 2003. ABHRS was widely promoted following a hospital-wide campaign in April 2005. ICPs assessed hand hygiene compliance for 16 months thereafter using daily observations over three 4-week intervals [17].
Statistical analysis
Time of onset and magnitude of change in ICU MRSA prevalence density was determined using change-point analysis (the change-point being the time of change in slope of the prevalence density of MRSA over time). Because multiple interventions occurred during the study, we chose a statistical model that allowed only one change-point but made no assumptions about its timing, which was estimated by best fit to the data using nonlinear regression. The model for the change-point analysis was:
where Y is the prevalence density, X is time, a is the intercept, b is the slope prior to the change-point, k, and c is the change in slope. Hence an estimated c < 0 represents a reduction of, while c > 0 represents an increase in, prevalence density. All p values used in the change-point analysis refer to the null hypothesis that c = 0. Data prior to October 2000 were graphically displayed but excluded from analysis as they were from the older, crowded ICU. The percentage decrease in ICU MRSA prevalence density was calculated using modelled values at the change-point and end of the study period. Change-point analysis, using the methodology described above, was used to determine when a change in broad-spectrum antibiotic use occurred. The change in trend of MRSA prevalence density and broad-spectrum antibiotic use was the difference in gradients before and after the change-point.
Linear regression was used to examine trends in consumption of IC consumables, ABHRS, individual antibiotic classes, ICU S. aureus bacteraemias, ICU MSSA prevalence density and hospital MRSA prevalence density over the study period. For only these proportionate change data, the outcome (dependent) variable was log transformed. Percentage change in explanatory variables over the study period was calculated using the following formula:
where X is the time period over which the change is measured and β is the slope of the log-transformed regression line after the change-point.
Because consecutive rates of MRSA are not independent variables, an autoregressive model (Prais–Winsten) accounting for autocorrelation, was chosen for multivariate analysis to assess temporal relationships between explanatory variables and ICU MRSA prevalence density. We selected a first-order autoregressive model using ICU MRSA prevalence density in the previous month as a predictor variable in the model to account for colonisation pressure such that
where α is the coefficient associated with the previous time period measure, β is a vector of coefficients that refer to all of the covariates we tested, X is a matrix with columns being the time periods and rows being the features of each that correspond to the covariates (e.g. numbers of gloves used per 1,000 patient-days) and ε is the error term. All analyses used Stata 10 (Stata Corp., College Station, TX, USA). A p value of ≤0.05 was considered statistically significant.
Results
Trends in the prevalence of MRSA and MSSA
The change in ICU MRSA prevalence density occurred in January 2004 (95% CI for date of change: August 2002–May 2005, p < 0.001), decreasing by 83% (95% CI 68–91% reduction, p < 0.001) at the end of the study period compared with the change-point value (Fig. 1). The gradient was 0.019/month (95% CI −0.14 to 0.17/month) before January 2004 and −0.23/month (95% CI −0.31 to −0.20/month) thereafter, denoting a change of −0.25/month (95% CI −0.33 to −0.17/month, p < 0.001), meaning that MRSA clinical isolates in ICU decreased by 0.25 isolates per 1,000 patient-days per month after the change-point. By log-linear regression, ICU MSSA prevalence density increased 38% (95% CI 1.3–84% increase, p = 0.04) over the study period.
ICU MRSA prevalence density and quality improvement interventions throughout ICU and hospital, 1 January 2000–30 June 2008. MRSA prevalence density decreased 83% (95% CI 68–91% reduction, p < 0.001) with a gradient change of −0.25/month (95% CI −0.33 to −0.17/month, p < 0.001) at January 2004 (95% CI for date of change, August 2002–May 2005)
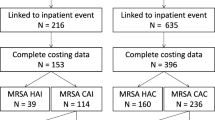
Table 2 shows trends in consumption of infection control consumables, antibiotics, and S. aureus prevalence density. The ICU MRSA bacteraemia rate decreased by 89% from 2001 (95% CI 79–94% decrease, p = 0.001), while the MSSA bacteraemia rate did not significantly change, although confidence intervals are wide (Fig. 2). Whole-hospital MRSA prevalence density also reduced, but much less dramatically (Table 2).
Trends in consumption of infection control consumables, alcohol-based hand rub solution and antibiotics in ICU
By log-linear regression, the use of all IC consumables, with the exception of medicated soap and alcohol-impregnated wipes, increased significantly. ABHRS use increased from January 2000–March 2005 compared with April 2005–June 2008, from a median of 7.7 to 132 l/1,000 patient-days, respectively, following the hand hygiene campaign. Hand hygiene compliance at baseline, 4 and 16 months was 33% (95% CI 30–36%), 49% (95% CI 46–52%) and 39% (95% CI 36–42%), respectively. Consumption of individual classes of antibiotics in ICU decreased significantly over the study period, with the exception of carbapenems (trend not statistically significant) and anti-pseudomonal penicillins, which increased, the latter likely reflecting the preference of intensivists and a change to the febrile neutropenia protocol in January 2005, recommending piperacillin–tazobactam for empiric therapy (Fig. 3). Using change-point analysis, broad-spectrum antibiotic use decreased by 26% (95% CI 12–38% reduction, p = 0.008) from August 2003 (gradient before 2.25/month, 95% CI −0.13 to 4.58/month; gradient after −2.15/month, 95% CI −3.43 to −0.87/month; change −4.40/month, 95% CI for the change in gradient −7.24 to −1.69/month, p = 0.001; 95% CI for date of change February 2003–February 2004, p < 0.001).
ICU antibiotic consumption with change-point analysis of broad-spectrum antibiotic use. Broad-spectrum antibiotics include the sum total of displayed antibiotics. Broad-spectrum antibiotic use decreased 26% (95% CI 12−38% reduction, p = 0.008) from August 2003 (95% CI for date of change, February 2003–February 2004) with a gradient change of −4.40/month (95% CI −7.24 to −1.69/month, p = 0.001)
Impact of infection control consumables and antibiotic consumption on MRSA
Results of an autoregressive model evaluating the impact of all explanatory variables on ICU MRSA prevalence density are shown in Table 3. Univariate analysis demonstrated significant temporal relationships for ABHRS, aminoglycosides, anti-pseudomonal penicillins and broad-spectrum antibiotics; however, multivariate analysis included only ABHRS and broad-spectrum antibiotic use. Individual classes of antibiotics were not analysed because: (a) the ecologic impact of aggregate broad-spectrum antibiotic use was our primary interest, and its analysis precluded the inclusion of component antibiotics; and (b) changes in antibiotic consumption reflected natural variations in prescribing practices without interventions targeting specific antibiotic classes. On multivariate analysis, only ABHRS use was associated with a significant decrease in MRSA prevalence density, i.e. use of one litre of ABHRS/1,000 patient-days reduced MRSA prevalence by 0.04 clinical isolates/1,000 patient-days/month (95% CI −0.024 to −0.064 clinical isolates/1,000 patient-days/month, p < 0.001).
Discussion
Using ecological data we report a sustained decline in endemic MRSA in an ICU following general IC and antibiotic stewardship interventions without the adoption of ASC or contact isolation of MRSA colonised patients. MRSA prevalence density decreased by 83% (95% CI 68–91% decrease, p < 0.001), coinciding with a period of intensified quality improvement activities from early 2004. On multivariate analysis, only ABHRS was significantly associated with a decrease in MRSA prevalence, but in reality MRSA fell in the context of multiple other interventions whose relative contributions could not be determined. A parallel reduction in the MRSA bacteraemia rate of 89% (95% CI 79–94% reduction, p = 0.001) compares favourably with the 75% reduction over 16 months achieved by Huang et al. [18] in an ICU using active MRSA surveillance cultures and contact isolation precautions. Like others [4, 18, 19], we observed no reduction in MSSA bacteraemia (in fact, ICU MSSA prevalence density increased significantly during the study period), suggesting that our interventions, aimed at preventing the emergence and transmission of antibiotic-resistant pathogens, were interrupting the transmission of MRSA. These interventions would not be expected to reduce infections due to endogenous flora such as MSSA, which is less influenced by measures designed to minimise cross-transmission of pathogens such as single rooms [20]. Had we adopted care bundles for the prevention of CLABSI or VAP, MSSA infections may have decreased, as MSSA is the predominant cause of these common ICU infections [21]. Of interest, increasing trauma admissions, a known risk factor for MRSA acquisition in ICU [22], did not lead to an expected increase in MRSA prevalence when RMH became a statewide trauma centre.
It is probable that ABHRS potentiated the decline in MRSA, but it alone is unlikely to explain the whole effect, as it was promoted as part of a hospital-wide campaign late in the study period. Although alcohol-based hand disinfection decreases nosocomial MRSA infection [23], compliance is consistently lowest in ICU areas [24]. Our rates are comparable to other US ICUs [25] and close to a postulated threshold of >40% proposed by modelling studies as necessary to prevent outbreaks of staphylococcal infection [26, 27]. It is conceivable that the hand hygiene audit tool used during the study period underestimated compliance due to its more stringent criteria [17] compared with later versions employed for this purpose [28].
Antibiotic stewardship and IC interventions may be complementary activities in controlling MRSA, but few studies have examined their influence concurrently. Recent time-series analyses have shown a consistent correlation between reduced hospital-wide use of fluoroquinolones, cephalosporins and macrolides and decreased MRSA infection or colonisation [29, 30]. It is encouraging then that significant reductions in fluoroquinolones, cephalosporins, aminoglycosides, glycopeptides and macrolides were observed. Although the autoregressive model did not demonstrate an effect of antibiotic selection pressure on MRSA burden, MRSA fell in the context of significant reductions in broad-spectrum antibiotics (26%, 95% CI 12–38% reduction, p = 0.008), suggesting a possible association. Perhaps the 1-month time lag in the model was too short to show the impact of antibiotics on MRSA when other investigations have reported delays of 3 months or more [29, 30], or the analysis of antibiotics in aggregate may have masked their individual effect on MRSA.
Few studies describe the long-term efficacy of multifaceted MRSA control programs in ICU without the use of ASC. A single centre noted a 73% reduction (p < 0.001) in ICU device-associated MRSA infection over 4 years without adoption of admission screening, but unlike our setting, contact precautions for colonised patients were routine [31]. Likewise, another Australian ICU with high levels of endemic MRSA achieved significant reductions in MRSA colonisation and infection (p < 0.047) over 5.5 years without screening or isolation [24].
Population-based IC measures may have a greater proportional benefit on all nosocomial infections compared with single-organism measures such as ASC for MRSA [32]. Daily chlorhexidine-based washing of ICU patients decreased acquisition of MRSA by 32% (p = 0.046) and vancomycin-resistant enterococcus (VRE) by 50% (p = 0.008) along with VRE bacteraemias (p = 0.008) [33], while a 66% reduction in CLABSI was achieved in US ICUs using evidence-based care bundles and organisational culture change [34].
Active surveillance cultures and contact isolation precautions for MRSA colonised patients are cost beneficial provided MRSA infections are prevented [5], but resource constraints, attendant opportunity costs and limited isolation rooms in our setting have tempered our support for this approach. Perhaps of most concern to our intensivists is the finding that single-room isolation is associated with a halving of HCW contact [35].
One of the limitations of this study is that we were unable to determine the significance of isolates because of lack of clinical information. This was partially mitigated by excluding screening swabs and duplicates and by analysing bacteraemias separately. Though not ideal, the use of all clinical isolates as a surveillance measure has been shown to correlate with MRSA incidence from sterile sites, with the advantages of being more sensitive to changes in MRSA incidence and less susceptible to the stochastic variation inherent in bacteraemia measures [36]. Distinguishing community from nosocomial acquisition was not possible from the dataset used, however MRSA in our setting is overwhelmingly health-care associated [37]. Chance events accounting for the decline in MRSA are possible, but the long study period argues against this. Changing strain properties are unlikely, as more transmissible or persistent strains are likely to be selected over time, thereby increasing MRSA rather than causing the reduction we observed [38]. Our discharge MRSA prevalence of 6.9% is lower than the admission prevalence in other local tertiary ICUs [23, 39], but the survey was performed at a time when MRSA was already in decline.
Decreased detection effort is not a likely confounder, as we used isolates collected for clinical reasons only and laboratory identification methods did not change. Response to the Acinetobacter outbreak reinforced general quality improvement measures and perhaps, for this reason, may also have had an effect on MRSA. No comparator pathogen with similar transmission dynamics to MRSA was available. Acinetobacter was unsuitable due to the outbreak, and clinical isolates of VRE were too few for statistical analysis. With respect to other nosocomial pathogens, carbapenem-susceptible Pseudomonas aeruginosa has increased since the introduction of our CDSS [40]. ASC as part of a research project are unlikely to have been influential, as they commenced late in the study period and were not acted upon. Finally, a decreasing length of stay in ICU over time may lead to a spurious reduction in MRSA prevalence, but the 17% reduction (p = 0.005) in hospital MRSA argues against exportation of a MRSA problem from ICU into the wards.
Turning the tide of endemic MRSA may be achievable without ASC and contact isolation precautions. Multimodal measures including adequate staffing, dedicated ICPs, ABHRS and antibiotic stewardship can be effective over the long term, even when the risk of nosocomial infection is high and the presence of endemic MRSA considerable. The relative efficacies of these measures could not be determined in our study, but in combination they confirm that successful interventions are often multifactorial [23, 34]. If the realistic aim in an endemic setting is to reduce rather than eliminate MRSA then our experience provides a compelling example of how this can be achieved without “search and destroy” IC measures.
References
Davis KA, Stewart JJ, Crouch HK, Florez CE, Hospenthal DR (2004) Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis 39:776–782
Jeyaratnam D, Edgeworth JD, French GL (2006) Enhanced surveillance of methicillin-resistant Staphylococcus aureus bacteraemia in a London teaching hospital. J Hosp Infect 63:365–373
Cepeda JA, Whitehouse T, Cooper B, Hails J, Jones K, Kwaku F, Taylor L, Hayman S, Cookson B, Shaw S, Kibbler C, Singer M, Bellingan G, Wilson AP (2005) Isolation of patients in single rooms or cohorts to reduce spread of MRSA in intensive-care units: prospective two-centre study. Lancet 365:295–304
Robicsek A, Beaumont JL, Paule SM, Hacek DM, Thomson RB Jr, Kaul KL, King P, Peterson LR (2008) Universal surveillance for methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Ann Intern Med 148:409–418
Clancy M, Graepler A, Wilson M, Douglas I, Johnson J, Price CS (2006) Active screening in high-risk units is an effective and cost-avoidant method to reduce the rate of methicillin-resistant Staphylococcus aureus infection in the hospital. Infect Control Hosp Epidemiol 27:1009–1017
Harbarth S, Masuet-Aumatell C, Schrenzel J, Francois P, Akakpo C, Renzi G, Pugin J, Ricou B, Pittet D (2006) Evaluation of rapid screening and pre-emptive contact isolation for detecting and controlling methicillin-resistant Staphylococcus aureus in critical care: an interventional cohort study. Crit Care 10:R25
Harbarth S, Fankhauser C, Schrenzel J, Christenson J, Gervaz P, Bandiera-Clerc C, Renzi G, Vernaz N, Sax H, Pittet D (2008) Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA 299:1149–1157
Jeyaratnam D, Whitty CJ, Phillips K, Liu D, Orezzi C, Ajoku U, French GL (2008) Impact of rapid screening tests on acquisition of meticillin resistant Staphylococcus aureus: cluster randomised crossover trial. BMJ 336:927–930
Calfee DP, Salgado CD, Classen D, Arias KM, Podgorny K, Anderson DJ, Burstin H, Coffin SE, Dubberke ER, Fraser V, Gerding DN, Griffin FA, Gross P, Kaye KS, Klompas M, Lo E, Marschall J, Mermel LA, Nicolle L, Pegues DA, Perl TM, Saint S, Weinstein RA, Wise R, Yokoe DS (2008) Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol 29(Suppl 1):S62–S80
Klevens RM, Edwards JR, Tenover FC, McDonald LC, Horan T, Gaynes R (2006) Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992–2003. Clin Infect Dis 42:389–391
Fluit AC, Wielders CL, Verhoef J, Schmitz FJ (2001) Epidemiology and susceptibility of 3,051 Staphylococcus aureus isolates from 25 university hospitals participating in the European SENTRY study. J Clin Microbiol 39:3727–3732
Nimmo GR, Pearson JC, Collignon PJ, Christiansen KJ, Coombs GW, Bell JM, McLaws ML (2007) Prevalence of MRSA among Staphylococcus aureus isolated from hospital inpatients, 2005: report from the Australian Group for Antimicrobial Resistance. Commun Dis Intell 31:288–296
Burton DC, Edwards JR, Horan TC, Jernigan JA, Fridkin SK (2009) Methicillin-resistant Staphylococcus aureus central line-associated bloodstream infections in US intensive care units, 1997–2007. JAMA 301:727–736
Thursky KA, Buising KL, Bak N, Macgregor L, Street AC, Macintyre CR, Presneill JJ, Cade JF, Brown GV (2006) Reduction of broad-spectrum antibiotic use with computerized decision support in an intensive care unit. Int J Qual Health Care 18:224–231
Buising KL, Thursky KA, Robertson MB, Black JF, Street AC, Richards MJ, Brown GV (2008) Electronic antibiotic stewardship—reduced consumption of broad-spectrum antibiotics using a computerized antimicrobial approval system in a hospital setting. J Antimicrob Chemother 62:608–616
VICNISS Hospital Acquired Infection Surveillance Coordinating Centre. VICNISS surveillance activities in our hospitals. http://www.vicniss.org.au/SurveillanceActivities.aspx. Accessed 12 Dec 2009
Rose L, Rogel K, Redl L, Cade JF (2009) Implementation of a multimodal infection control program during an Acinetobacter outbreak. Intensive Crit Care Nurs 25:57–63
Huang SS, Yokoe DS, Hinrichsen VL, Spurchise LS, Datta R, Miroshnik I, Platt R (2006) Impact of routine intensive care unit surveillance cultures and resultant barrier precautions on hospital-wide methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis 43:971–978
National Audit Office Report (HC 560 2008–2009): trends in rates of healthcare associated infection in England 2004 to 2008. http://web.nao.org.uk/search/search.aspx?Schema=&terms=health+care+associated+infections. Accessed 12 Dec 2009
Bracco D, Dubois MJ, Bouali R, Eggimann P (2007) Single rooms may help to prevent nosocomial bloodstream infection and cross-transmission of methicillin-resistant Staphylococcus aureus in intensive care units. Intensive Care Med 33:836–840
Zhanel GG, DeCorby M, Laing N, Weshnoweski B, Vashisht R, Tailor F, Nichol KA, Wierzbowski A, Baudry PJ, Karlowsky JA, Lagace-Wiens P, Walkty A, McCracken M, Mulvey MR, Johnson J, Hoban DJ (2008) Antimicrobial-resistant pathogens in intensive care units in Canada: results of the Canadian National Intensive Care Unit (CAN-ICU) study, 2005–2006. Antimicrob Agents Chemother 52:1430–1437
Marshall C, Wolfe R, Kossmann T, Wesselingh S, Harrington G, Spelman D (2004) Risk factors for acquisition of methicillin-resistant Staphylococcus aureus (MRSA) by trauma patients in the intensive care unit. J Hosp Infect 57:245–252
Johnson PD, Martin R, Burrell LJ, Grabsch EA, Kirsa SW, O’Keeffe J, Mayall BC, Edmonds D, Barr W, Bolger C, Naidoo H, Grayson ML (2005) Efficacy of an alcohol/chlorhexidine hand hygiene program in a hospital with high rates of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection. Med J Aust 183:509–514
Harrington G, Watson K, Bailey M, Land G, Borrell S, Houston L, Kehoe R, Bass P, Cockroft E, Marshall C, Mijch A, Spelman D (2007) Reduction in hospitalwide incidence of infection or colonization with methicillin-resistant Staphylococcus aureus with use of antimicrobial hand-hygiene gel and statistical process control charts. Infect Control Hosp Epidemiol 28:837–844
McGuckin M, Waterman R, Govednik J (2009) Hand hygiene compliance rates in the United States—a one-year multicenter collaboration using product/volume usage measurement and feedback. Am J Med Qual 24:205–213
Cooper BS, Medley GF, Scott GM (1999) Preliminary analysis of the transmission dynamics of nosocomial infections: stochastic and management effects. J Hosp Infect 43:131–147
McBryde ES, Pettitt AN, McElwain DL (2007) A stochastic mathematical model of methicillin resistant Staphylococcus aureus transmission in an intensive care unit: predicting the impact of interventions. J Theor Biol 245:470–481
Hand Hygiene Australia. Resources for healthcare workers. http://www.hha.org.au/ForHealthcareWorkers.aspx. Accessed 12 Dec 2009
Vernaz N, Sax H, Pittet D, Bonnabry P, Schrenzel J, Harbarth S (2008) Temporal effects of antibiotic use and hand rub consumption on the incidence of MRSA and Clostridium difficile. J Antimicrob Chemother 62:601–607
Kaier K, Hagist C, Frank U, Conrad A, Meyer E (2009) Two time-series analyses of the impact of antibiotic consumption and alcohol-based hand disinfection on the incidences of nosocomial methicillin-resistant Staphylococcus aureus infection and Clostridium difficile infection. Infect Control Hosp Epidemiol 30:346–353
Edmond MB, Ober JF, Bearman G (2008) Active surveillance cultures are not required to control MRSA infections in the critical care setting. Am J Infect Control 36:461–463
Wenzel RP, Bearman G, Edmond MB (2008) Screening for MRSA: a flawed hospital infection control intervention. Infect Control Hosp Epidemiol 29:1012–1018
Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, Speck K, Jernigan JA, Robles JR, Wong ES (2009) The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med 37:1858–1865
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355:2725–2732
Evans HL, Shaffer MM, Hughes MG, Smith RL, Chong TW, Raymond DP, Pelletier SJ, Pruett TL, Sawyer RG (2003) Contact isolation in surgical patients: a barrier to care? Surgery 134:180–188
Walker S, Peto TE, O’Connor L, Crook DW, Wyllie D (2008) Are there better methods of monitoring MRSA control than bacteraemia surveillance? An observational database study. PLoS ONE 3:e2378
Nimmo GR, Coombs GW (2008) Community-associated methicillin-resistant Staphylococcus aureus (MRSA) in Australia. Int J Antimicrob Agents 31:401–410
Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, Duckworth GJ, Lai R, Ebrahim S (2003) Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling. Health Technol Assess 7:1–194
Marshall C, Harrington G, Wolfe R, Fairley CK, Wesselingh S, Spelman D (2003) Acquisition of methicillin-resistant Staphylococcus aureus in a large intensive care unit. Infect Control Hosp Epidemiol 24:322–326
Yong MK, Buising KL, Cheng AC, Thursky KA (2010) Improved susceptibility of Gram-negative bacteria in an intensive care unit following implementation of a computerized antibiotic decision support system. J Antimicrob Chemother 65:1062–1069
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ananda-Rajah, M.R., McBryde, E.S., Buising, K.L. et al. The role of general quality improvement measures in decreasing the burden of endemic MRSA in a medical–surgical intensive care unit. Intensive Care Med 36, 1890–1898 (2010). https://doi.org/10.1007/s00134-010-2019-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2019-x