Abstract
Purpose
To estimate the prevalence, risk factors, prophylactic treatment and impact on mortality for venous thromboembolism (VTE) in patients with moderate to severe traumatic brain injury (TBI) treated in the intensive care unit.
Methods
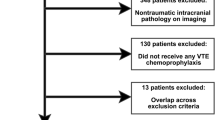
A post hoc analysis of the erythropoietin in traumatic brain injury (EPO-TBI) trial that included twice-weekly lower limb ultrasound screening. Venous thrombotic events were defined as ultrasound-proven proximal deep venous thrombosis (DVT) or clinically detected pulmonary embolism (PE). Results are reported as events, percentages or medians and interquartile range (IQR). Cox regression analysis was used to calculate adjusted hazard ratios (HR) with 95% confidence intervals (CI) for time to VTE and death.
Results
Of 603 patients, 119 (19.7%) developed VTE, mostly comprising DVT (102 patients, 16.9%) with a smaller number of PE events (24 patients, 4.0%). Median time to DVT diagnosis was 6 days (IQR 2–11) and to PE diagnosis 6.5 days (IQR 2–16.5). Mechanical prophylaxis (MP) was used in 91% of patients on day 1, 97% of patients on day 3 and 98% of patients on day 7. Pharmacological prophylaxis was given in 5% of patients on day 1, 30% of patients on day 3 and 57% of patients on day 7. Factors associated with time to VTE were age (HR per year 1.02, 95% CI 1.01–1.03), patient weight (HR per kg 1.01, 95% CI 1–1.02) and TBI severity according to the International Mission for Prognosis and Analysis of Clinical Trials risk of poor outcome (HR per 10% increase 1.12, 95% CI 1.01–1.25). The development of VTE was not associated with mortality (HR 0.92, 95% CI 0.51–1.65).
Conclusions
Despite mechanical and pharmacological prophylaxis, VTE occurs in one out of every five patients with TBI treated in the ICU. Higher age, greater weight and greater severity of TBI increase the risk. The development of VTE was not associated with excess mortality.


Similar content being viewed by others
References
Phelan HA (2013) Venous thromboembolism after traumatic brain injury. Semin Thromb Hemost 39:541–548
Abdel-Aziz H, Dunham CM, Malik RJ, Hileman BM (2015) Timing for deep vein thrombosis chemoprophylaxis in traumatic brain injury: an evidence-based review. Crit Care 19:96
Lier H, Bottiger BW, Hinkelbein J, Krep H, Bernhard M (2011) Coagulation management in multiple trauma: a systematic review. Intensive Care Med 37:572–582
Ho KM, Burrell M, Rao S, Baker R (2010) Incidence and risk factors for fatal pulmonary embolism after major trauma: a nested cohort study. Br J Anaesth 105:596–602
Allen CJ, Murray CR, Meizoso JP, Ginzburg E, Schulman CI, Lineen EB, Namias N, Proctor KG (2016) Surveillance and early management of deep vein thrombosis decreases rate of pulmonary embolism in high-risk trauma patients. J Am Coll Surg 222:65–72
Geerts WH, Code KI, Jay RM, Chen E, Szalai JP (1994) A prospective study of venous thromboembolism after major trauma. N Engl J Med 331:1601–1606
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care, AANS/CNS, Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW (2007) Guidelines for the management of severe traumatic brain injury. V. Deep vein thrombosis prophylaxis. J Neurotrauma 24(Suppl 1):S32–S36
Nichol A, French C, Little L, Haddad S, Presneill J, Arabi Y, Bailey M, Cooper DJ, Duranteau J, Huet O, Mak A, McArthur C, Pettila V, Skrifvars M, Vallance S, Varma D, Wills J, Bellomo R, EPO-TBI Investigators, ANZICS Clinical Trials Group (2015) Erythropoietin in traumatic brain injury (EPO-TBI): a double-blind randomised controlled trial. Lancet 386:2499–2506
Nichol A, French C, Little L, Presneill J, Cooper DJ, Haddad S, Duranteau J, Huet O, Skrifvars M, Arabi Y, Bellomo R, EPO-TBI Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group (2015) Erythropoietin in traumatic brain injury: study protocol for a randomised controlled trial. Trials 16:39
Corwin HL, Gettinger A, Fabian TC, May A, Pearl RG, Heard S, An R, Bowers PJ, Burton P, Klausner MA, Corwin MJ, EPO Critical Care Trials Group (2007) Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med 357:965–976
Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, Epo Severe TBITI, Baldwin A, Rivera Lara L, Saucedo-Crespo H, Ahmed O, Sadasivan S, Ponce L, Cruz-Navarro J, Shahin H, Aisiku IP, Doshi P, Valadka A, Neipert L, Waguspack JM, Rubin ML, Benoit JS, Swank P (2014) Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA 312:36–47
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D, Investigators C (2006) Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 355:2085–2098
Ekeh AP, Dominguez KM, Markert RJ, McCarthy MC (2010) Incidence and risk factors for deep venous thrombosis after moderate and severe brain injury. J Trauma 68:912–915
Ortel TL (2010) Acquired thrombotic risk factors in the critical care setting. Crit Care Med 38:S43–S50
Reiff DA, Haricharan RN, Bullington NM, Griffin RL, McGwin G Jr, Rue LW 3rd (2009) Traumatic brain injury is associated with the development of deep vein thrombosis independent of pharmacological prophylaxis. J Trauma 66:1436–1440
Knudson MM, Ikossi DG, Khaw L, Morabito D, Speetzen LS (2004) Thromboembolism after trauma: an analysis of 1602 episodes from the American College of Surgeons National Trauma Data Bank. Ann Surg 240:490–496 (discussion 496-498)
Presneill J, Little L, Nichol A, French C, Cooper DJ, Haddad S, Duranteau J, Huet O, Skrifvars M, Arabi Y, Bellomo R, EPO-TBI Investigators, ANZICS Clinical Trials Group (2014) Statistical analysis plan for the Erythropoietin in Traumatic Brain Injury trial: a randomised controlled trial of erythropoietin versus placebo in moderate and severe traumatic brain injury. Trials 15:501
PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Cook D, Meade M et al (2011) Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med 364:1305–1314
Garcia-Olivares P, Guerrero JE, Galdos P, Carriedo D, Murillo F, Rivera A (2014) PROF-ETEV study: prophylaxis of venous thromboembolic disease in critical care units in Spain. Intensive Care Med 40:1698–1708
Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW (2008) Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 117:93–102
Tracy RP (2002) Hemostatic and inflammatory markers as risk factors for coronary disease in the elderly. Am J Geriatr Cardiol 11(93–100):107
Kasjanovova D, Adameckova D, Gratzlova J, Hegyi L (1993) Sex-related and age-related differences in platelet function in vitro: influence of hematocrit. Mech Ageing Dev 71:103–109
Gleerup G, Winther K (1995) The effect of ageing on platelet function and fibrinolytic activity. Angiology 46:715–718
Taddei S, Virdis A, Ghiadoni L, Salvetti G, Bernini G, Magagna A, Salvetti A (2001) Age-related reduction of NO availability and oxidative stress in humans. Hypertension 38:274–279 (Dallas, Tex: 1979)
Martinelli I, Bucciarelli P, Mannucci PM (2010) Thrombotic risk factors: basic pathophysiology. Crit Care Med 38:S3–S9
Franchini M, Targher G, Montagnana M, Lippi G (2008) The metabolic syndrome and the risk of arterial and venous thrombosis. Thromb Res 122:727–735
Nunez JM, Becher RD, Rebo GJ, Farrah JP, Borgerding EM, Stirparo JJ, Lauer C, Kilgo P, Miller PR (2015) Prospective evaluation of weight-based prophylactic enoxaparin dosing in critically Ill trauma patients: adequacy of antixa levels is improved. Am Surg 81:605–609
Ko A, Harada MY, Barmparas G, Chung K, Mason R, Yim DA, Dhillon N, Margulies DR, Gewertz BL, Ley EJ (2016) Association between enoxaparin dosage adjusted by anti-factor Xa trough level and clinically evident venous thromboembolism after trauma. JAMA Surg 151:1006–1013
Aryafar H, Kinney TB (2010) Optional inferior vena cava filters in the trauma patient. Semin Intervent Radiol 27:68–80
Beitland S, Sandven I, Kjærvik LK, Sandset PM, Sunde K, Eken T (2015) Thromboprophylaxis with low molecular weight heparin versus unfractionated heparin in intensive care patients: a systematic review with meta-anlaysis and trial sequential analysis. Intensive Care Med 41:1209–1219
Acknowledgements
Markus Skrifvars has received unrestricted grant support from Finska Läkaresällskapet, Medicinska Understödsföreningen Liv och Hälsa and Svenska Kulturfonden.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
Markus Skrifvars reports having received a research grant from GE Healthcare and travel reimbursements and lecture fees from Orion Pharma, COVIDIEN, Astellas Pharma and Axis-Shield. All other authors report that they have no conflicts of interest.
Additional information
Take-home message: Despite mechanical and pharmacological prophylaxis, venous thromboembolism occurs in one of five patients with traumatic brain injury treated in the intensive care unit. Older age, greater weight and traumatic brain injury severity increase this risk.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Skrifvars, M.B., Bailey, M., Presneill, J. et al. Venous thromboembolic events in critically ill traumatic brain injury patients. Intensive Care Med 43, 419–428 (2017). https://doi.org/10.1007/s00134-016-4655-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4655-2