Abstract
Purpose
To evaluate the kinematics/kinetics of the ankle, knee, hip in the sagittal plane in adolescents with recurrent patellar dislocation in comparison to a healthy control.
Methods
Case–control study. Eighty-eight knees (67 patients) with recurrent patellar dislocation (mean age 14.8 years ± 2.8 SD) were compared to 54 healthy knees (27 individuals, 14.9 years ± 2.4 SD). Kinematics/kinetics of ankle, knee, hip, and pelvis were captured using 3D-gait analysis (VICON, 12 cameras, 200 Hz, Plug-in-Gait, two force plates). One cycle (100%) consisted of 51 data-points. The mean of six trials was computed.
Results
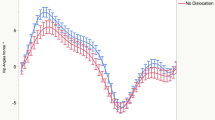
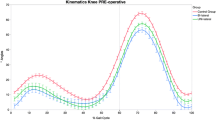
The loading-response increased by 0.02 s ± 0.01SE (10.8%) with dislocations (0.98% of total gait, P < 0.01). The mid-stance-phase decreased equally (P < 0.01). Dislocation decreased knee flexion during the entire gait cycle (P < 0.01), with the largest difference during mid-stance (9.0° ± 7.2 SD vs. 18.5° ± 6.7 SD). Dislocation increased plantar-flexion during loading response 4.1° ± 0.4 SE with (P < 0.01), afterward, the dorsal-extension decreased 3.2° ± 0.3 SE, (P < 0.01). Dislocation decreased hip flexion during all phases (P < 0.01). Maximal difference: 7.5° ± 0.5 SE during mid-stance. 80% of all patients developed this gait pattern.
Internal moments of the ankle increased, of the knee and hip decreased during the first part of stance.
Conclusion
Recurrent patellar dislocation decreases knee flexion during the loading-response and mid-stance phase. A decreased hip flexion and increased plantar-flexion, while adjusting internal moments, indicate a compensation mechanism.
Level of evidence
III.


Similar content being viewed by others
References
Alkjaer T, Simonsen EB, Peter Magnusson SP, Aagaard H, Dyhre-Poulsen P (2002) Differences in the movement pattern of a forward lunge in two types of anterior cruciate ligament deficient patients: copers and non-copers. Clin Biomech (Bristol, Avon) 17:586–593
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15:48–56
Amis AA, Oguz C, Bull AMJ, Senavongse W, Dejour D (2008) The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Jt Surg Br 90:864–869
Arnold AS, Anderson FC, Pandy MG, Delp SL (2005) Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J Biomech 38:2181–2189
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, Imhoff AB, Schöttle PB (2014) Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc 22:2591–2598
Barton CJ, Levinger P, Menz HB, Webster KE (2009) Kinematic gait characteristics associated with patellofemoral pain syndrome: a systematic review. Gait Posture 30:405–416
Berchuck M, Andriacchi TP, Bach BR, Reider B (1990) Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Jt Surg Am 72:871–877
Brunner R, Dreher T, Romkes J, Frigo C (2008) Effects of plantar flexion on pelvis and lower limb kinematics. Gait Posture 28:150–156
Camathias C, Speth BM, Rutz E, Schlemmer T, Papp K, Vavken P, Studer K (2018) Solitary trochleoplasty for treatment of recurrent patellar dislocation. JBJS Essent Surg Tech 8(2):e11
Camathias C, Studer K, Kiapour A, Rutz E, Vavken P (2016) Trochleoplasty as a solitary treatment for recurrent patellar dislocation results in good clinical outcome in adolescents. Am J Sports Med 44:2855–2863
Chmielewski TL, Rudolph KS, Fitzgerald GK, Axe MJ, Snyder-Mackler L (2001) Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech (Bristol, Avon) 16:586–591
Chotel F, Bérard J, Raux S (2014) Patellar instability in children and adolescents. Orthop Traumatol Surg Res 100:S125–S137
Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ (2017) Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med 45:2105–2110
Colvin AC, West RV (2008) Patellar instability. J Bone Jt Surg Am 90:2751–2762
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dunn DM (1952) Anteversion of the neck of the femur; a method of measurement. J Bone Jt Surg Br 34-B:181–186
Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10:215–220
Fithian DC (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Hart JM, Ko J-WK, Konold T, Pietrosimone B, Pietrosimione B (2010) Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech (Bristol, Avon) 25:277–283
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations. The natural history. Am J Sports Med 14:117–120
Hurd WJ, Snyder-Mackler L (2007) Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res 25:1369–1377
Insall J, Goldberg V, Salvati E (1972) Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res 88:67–69
Kadaba MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8:383–392
Kainz H, Graham D, Edwards J, Walsh HPJ, Maine S, Boyd RN, Lloyd DG, Modenese L, Carty CP (2017) Reliability of four models for clinical gait analysis. Gait Posture 54:325–331
Kimmel SA, Schwartz MH (2006) A baseline of dynamic muscle function during gait. Gait Posture 23:211–221
Knoll Z, Kocsis L, Kiss RM (2004) Gait patterns before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12:7–14
Lindström M, Felländer-Tsai L, Wredmark T, Henriksson M (2010) Adaptations of gait and muscle activation in chronic ACL deficiency. Knee Surg Sports Traumatol Arthrosc 18:106–114
Maenpaa H, Lehto MU (1997) Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med 25:213–217
Mentiplay BF, Clark RA (2018) Modified conventional gait model versus cluster tracking: test-retest reliability, agreement and impact of inverse kinematics with joint constraints on kinematic and kinetic data. Gait Posture 64:75–83
Nadeau S, Gravel D, Hébert LJ, Arsenault AB, Lepage Y (1997) Gait study of patients with patellofemoral pain syndrome. Gait Posture 5:21–27
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14:513–515
Perry J, Burnfield JM (2010) Gait analysis. SLACK Incorporated, New Jersey
Redler LH, Wright ML (2018) Surgical management of patellofemoral instability in the skeletally immature patient. J Am Acad Orthop Surg 26:e405–e415
Reed-Jones RJ, Vallis LA (2008) Kinematics and muscular responses to a ramp descent in the ACL deficient knee. Knee 15:117–124
Roberts CS, Rash GS, Honaker JT, Wachowiak MP, Shaw JC (1999) A deficient anterior cruciate ligament does not lead to quadriceps avoidance gait. Gait Posture Elsevier 10:189–199
Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L (1998) 1998 Basmajian Student Award Paper: movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol 8:349–362
Schwartz M, Lakin G (2003) The effect of tibial torsion on the dynamic function of the soleus during gait. Gait Posture 17:113–118
Senavongse W, Amis AA (2005) The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Jt Surg Br 87:577–582
Senavongse W, Farahmand F, Jones J, Andersen H, Bull AMJ (2006) Quantitative measurement of patellofemoral joint stability: force–displacement behavior of the human patella in vitro. J Orthop Res 21:780–786
Stief F, Böhm H, Michel K, Schwirtz A, Döderlein L (2013) Reliability and accuracy in three-dimensional gait analysis: a comparison of two lower body protocols. J Appl Biomech 29:105–111
Torry MR, Decker MJ, Ellis HB, Shelburne KB, Sterett WI, Steadman JR (2004) Mechanisms of compensating for anterior cruciate ligament deficiency during gait. Med Sci Sports Exerc 36:1403–1412
Torry MR, Decker MJ, Viola RW, O'Connor DD, Steadman JR (2000) Intra-articular knee joint effusion induces quadriceps avoidance gait patterns. Clin Biomech (Bristol, Avon) 15:147–159
Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G (2013) Treating patella instability in skeletally immature patients. Arthroscopy 29:1410–1422
Werner S (2014) Anterior knee pain: an update of physical therapy. Knee Surg Sports Traumatol Arthrosc 22:2286–2294
Wexler G, Hurwitz DE, Bush-Joseph CA, Andriacchi TP, Bach BR (1998) Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Relat Res 348:166–175
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors have nothing to disclose that could have direct or potential influence or impart bias on the work.
Funding
No external source of funding was used.
Ethical approval
This research has been performed with the approval of the local ethics committee (ethics committee of Basel, No. 2013/104).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Camathias, C., Ammann, E., Meier, R.L. et al. Recurrent patellar dislocations in adolescents result in decreased knee flexion during the entire gait cycle. Knee Surg Sports Traumatol Arthrosc 28, 2053–2066 (2020). https://doi.org/10.1007/s00167-020-05911-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05911-y