Abstract
Introduction and hypothesis
The aim was to compare objective and subjective cure rates between Uphold™ hysteropexy (HP) and vaginal hysterectomy (VH) with uterosacral suspension.
Methods
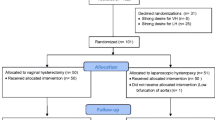
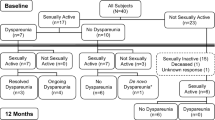
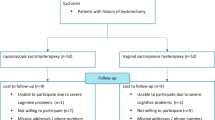
A sample size of 49 in each arm would be required to detect a clinical difference of 20% between the groups. Owing to delayed recruitment, this originally planned randomised controlled trial was changed to a patient preference study after randomising initial 6 participants. Women with symptomatic stage ≥2 uterine descent wishing a surgical solution were included. Routine follow-up was scheduled at 6 weeks, 6 months, 12 months, and annually thereafter. Primary outcome was absence of stage ≥2 apical prolapse. Secondary outcomes included a composite cure of no leading edge beyond the hymen, absence of bulge symptoms and no retreatment; patient-reported outcomes were based on quality-of-life questionnaires (PFDI-20, PFIQ-7, PISQ-12, PGI-I, EQ5D and a health score).
Results
We recruited 50 patients undergoing VH between 2011 and 2013 and 51 patients undergoing HP between 2011 and 2016. Participants were followed up for a median of 25 months (23–96). Five women from the VH (10%) and 7 from the HP (14%) group were lost to follow-up. Combined anatomical and symptomatic outcomes were available for 41 (82%) VH and 39 (76%) in the HP group. There was no difference in objective apical outcomes; the incidence of stage 2 prolapse was 0% in the VH group and 2% in HP group (p = 0.50). We found no difference in the composite cure rate (78% VH vs 85% HP, 0.45) between the groups. There was no significant difference in surgical complications (p = 0.33), assessed using Clavien–Dindo classification. There was a 2% surgery rate for mesh exposure in the HP group.
Conclusions
Uphold™ uterine suspension and VH appear to have similar objective and subjective cure at 25 months, with no significant difference in surgical complications.




Similar content being viewed by others
References
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470 e471–6. https://doi.org/10.1016/j.ajog.2013.08.003.
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD. Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg. 2013;19(2):103–9. https://doi.org/10.1097/SPV.0b013e31827d8667.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803–13. https://doi.org/10.1007/s00192-013-2171-2.
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645–50. https://doi.org/10.1067/mob.2003.75.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):381–4 discussion 384–385.
Van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–5; discussion 355. https://doi.org/10.1007/s00192-003-1084-x.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16. https://doi.org/10.1007/s00192-009-1014-7.
Jia X, Glazener C, Mowatt G, Jenkinson D, Fraser C, Bain C, et al. Systematic review of the efficacy and safety of using mesh in surgery for uterine or vaginal vault prolapse. Int Urogynecol J. 2010;21(11):1413–31. https://doi.org/10.1007/s00192-010-1156-7.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079. https://doi.org/10.1002/14651858.CD012079.
Goldberg RP, Tomezsko JE, Winkler HA, Koduri S, Culligan PJ, Sand PK. Anterior or posterior sacrospinous vaginal vault suspension: long-term anatomic and functional evaluation. Obstet Gynecol. 2001;98(2):199–204.
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61. https://doi.org/10.1007/s00192-012-1780-5.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183(6):1365–73; discussion 1373-4. https://doi.org/10.1067/mob.2000.110910.
Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. Joint report on terminology for surgical procedures to treat pelvic organ prolapse. Int Urogynecol J. 2020;31(3):429–63. https://doi.org/10.1007/s00192-020-04236-1.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI−20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):164–8; discussion 168. https://doi.org/10.1007/s00192-003-1063-2.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8. https://doi.org/10.1007/s00192-009-1069-5.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Int Urogynecol J. 2011;22(1):3–15. https://doi.org/10.1007/s00192-010-1324-9.
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, et al. An International Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Neurourol Urodyn. 2012;31(4):415–21. https://doi.org/10.1002/nau.22238.
Haylen BT, Maher C, Deprest J. IUGA/ICS terminology and classification of complications of prosthesis and graft insertion—rereading will revalidate. Am J Obstet Gynecol. 2013;208(1):e15. https://doi.org/10.1016/j.ajog.2012.08.004.
Nager CW, Visco AG, Richter HE, Rardin CR, Rogers RG, Harvie HS, et al. Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054–65. https://doi.org/10.1001/jama.2019.12812.
Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111(1):50–6.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92. https://doi.org/10.1097/01.MLR.0000062554.74615.4C.
Pellino G, Ramage L, Simillis C, Warren O, Kontovounisios C, Tan E, et al. Evaluation of sexual dysfunction in female patients presenting with faecal incontinence or defecation disorder. Int J Colorectal Dis. 2017;32(5):667–74. https://doi.org/10.1007/s00384-017-2795-7.
Liao SC, Huang WC, Su TH, Lau HH. Changes in female sexual function after vaginal mesh repair versus native tissue repair for pelvic organ prolapse: a meta-analysis of randomized controlled trials. J Sex Med. 2019;16(5):633–9. https://doi.org/10.1016/j.jsxm.2019.02.016.
Lo TS, Pue LB, Tan YL, Hsieh WC, Kao CC, Uy-Patrimonio MC. Anterior-apical single-incision mesh surgery (uphold): 1-year outcomes on lower urinary tract symptoms, anatomy and ultrasonography. Int Urogynecol J. 2019;30(7):1163–72. https://doi.org/10.1007/s00192-018-3691-6.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–146.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8. https://doi.org/10.1007/s00192-014-2564-x.
Rahkola-Soisalo P, Mikkola TS, Altman D, Falconer C, Nordic TVMG. Pelvic organ prolapse repair using the uphold vaginal support system: 5-year follow-up. Female Pelvic Med Reconstr Surg. 2019;25(3):200–5. https://doi.org/10.1097/SPV.0000000000000530.
Moorman PG, Myers ER, Schildkraut JM, Iversen ES, Wang F, Warren N. Effect of hysterectomy with ovarian preservation on ovarian function. Obstet Gynecol. 2011;118(6):1271–9. https://doi.org/10.1097/AOG.0b013e318236fd12.
Therapeutic Goods Administration (2019) Transvaginal (urogynaecological) surgical mesh. https://www.tga.gov.au/hubs/transvaginal-mesh.
U.S. Food & Drug Administration (2019) Urogynecologic surgical mesh implants. https://www.fda.gov/medical-devices/implants-and-prosthetics/urogynecologic-surgical-mesh-implants.
Authors’ participation
M. Kulkarni: follow-up, database, manuscript preparation; N. Young: study design, recruitment, follow-up, database, manuscript preparation; J. Lee: study design, recruitment, follow-up, database, manuscript preparation; A. Rosamilia: study design, recruitment, follow-up, database, manuscript preparation.
Funding
This study was an investigator-initiated and -led study with financial support from Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund a research nurse salary and other costs related to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Kulkarni: none; N. Young: none; J. Lee: this study was an investigator-initiated and -led study with financial support by Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund research nurse salary and other costs related to the study; A. Rosamilia: this study was an investigator-initiated and -led study with financial support by Boston Scientific. These funds were transferred to Monash University fund at arm’s length from the investigators and used to fund research nurse salary and other costs related to the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Kulkarni, M., Young, N., Lee, J. et al. Hysterectomy with uterosacral suspension or Uphold™ hysteropexy in women with apical prolapse: a parallel cohort study. Int Urogynecol J 31, 2137–2146 (2020). https://doi.org/10.1007/s00192-020-04328-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04328-y