Abstract
Summary
The cost-effectiveness of Fracture Liaison Services (FLSs) for prevention of secondary fracture in osteoporosis patients in the United Kingdom (UK), and the cost associated with their widespread adoption, were evaluated. An estimated 18 fractures were prevented and £21,000 saved per 1,000 patients. Setup across the UK would cost an estimated £9.7 million.
Introduction
Only 11% to 28% of patients with a fragility fracture receive osteoporosis treatment in the UK. FLSs provide an efficient means to identify patients and are endorsed by the Department of Health but have not been widely adopted. The objective of this study was to evaluate the cost-effectiveness of FLSs in the UK and the cost associated with their widespread adoption.
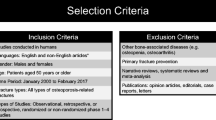
Methods
A cost-effectiveness and budget-impact model was developed, utilising detailed audit data collected by the West Glasgow FLS.
Results
For a hypothetical cohort of 1,000 fragility-fracture patients (740 requiring treatment), 686 received treatment in the FLS compared with 193 in usual care. Assessments and osteoporosis treatments cost an additional £83,598 and £206,544, respectively, in the FLS; 18 fractures (including 11 hip fractures) were prevented, giving an overall saving of £21,000. Setup costs for widespread adoption of FLSs across the UK were estimated at £9.7 million.
Conclusions
FLSs are cost-effective for the prevention of further fractures in fragility-fracture patients. The cost of widespread adoption of FLS across the UK is small in comparison with other service provision and would be expected to result in important benefits in fractures avoided and reduced hospital bed occupancy.


Similar content being viewed by others
Notes
In an audit of the Glasgow Direct Access DXA Service, GPs instituted the recommended treatment in 96% of cases and another treatment in most remaining cases. In a survey of patients recommended treatment by the Glasgow FLS 6 to 12 months after initiation of therapy, of the 66% of those who responded, 86% to 88% indicated they were taking the recommended treatment.
References
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The FLS: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
National Institute for Health and Clinical Excellence. (2008a) Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women. Guidance and Assessment Report No. 160. http://www.nice.org.uk/nicemedia/pdf/Assessment_report_osteo.pdf. Accessed 14 September 2009
National Institute for Health and Clinical Excellence. (2008b) Alendronate, etidronate, risedronate, raloxifene, strontium ranelate and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women. Guidance and Assessment Report No. 161. http://www.nice.org.uk/nicemedia/pdf/Osteo%20_AR.pdf. Accessed 14 September 2009
Royal College of Physicians. (1999) Osteoporosis: clinical guidelines for prevention and treatment. http://www.rcplondon.ac.uk/Pubs/brochure.aspx?e=136. Accessed 24 September 2009
Scottish Intercollegiate Guidelines Network. (2003) Guideline 71: management of osteoporosis. http://www.sign.ac.uk/pdf/sign71.pdf. Accessed 24 September 2009
McLellan AR, Reid DM, Forbes K, Reid R, Campbell C, Gregori A, Raby N, Simpson A (2004) Effectiveness of strategies for the secondary prevention of osteoporotic fractures in Scotland, an audit funded by NHS Quality Improvement Scotland (Project CEPS 99/03). http://www.nhshealthquality.org/nhsqis/2755.html. Accessed 2 November 2009
Hippisley-Cox J, Bayly J, Potter J, et al. (2007) Evaluation of standards of care for osteoporosis and falls in primary care. QRESEARCH and NHS: the Information Centre for health and social care. http://www.ic.nhs.uk/webfiles/publications/GPosteoporisiscare/Evaluation%20of%20Standards%20of%20Care%20for%20Osteoporosis%20and%20Falls%20in%20Primary%20Care%20Report.pdf. Accessed 24 September 2009
Royal College of Physicians, The Clinical Effectiveness and Evaluation Unit, Clinical Standards Department. (2009) National audit of the organisation of services for falls and bone health of older people. http://www.rcplondon.ac.uk/clinical-standards/ceeu/Current-work/Falls/Documents/National-Falls-and-Bone-Health-Public-Audit-Report-March-2009.pdf. Accessed 14 September 2009
Fraser M, McLellan AR (2004) A fracture liaison service for patients with osteoporotic fractures. Prof Nurse 19(5):286–290
Department of Health (2009c). Falls and fractures, effective interventions in health and social care. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_103146. Accessed 16 December 2009
Royal College of Physicians, The Clinical Effectiveness and Evaluation Unit of the Royal College of Physicians. (2007) National clinical audit of falls and bone health in older people. http://www.rcplondon.ac.uk/clinical-standards/ceeu/Documents/fbhop-nationalreport.pdf. Accessed 14 September 2009
Majumdar SR, Johnson JA, Lier DA et al (2007) Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 18(3):261–270
Majumdar SR, Lier DA, Beaupre LA et al (2009) Osteoporosis case manager for patients with hip fractures: results of a cost-effectiveness analysis conducted alongside a randomized trial. Arch Intern Med 169(1):25–31
Sander B, Elliot-Gibson V, Beaton D, Bogoch ER, Maetzel A (2008) A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. J Bone Joint Surg 90:1197–1205
Dell R, Greene D, Schelkun SR, Williams K (2008) Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg 90(suppl 4):188–194
Department of Health. (2009a) DH/SC,LG & CP Directorate/Older People and Dementia Fracture Prevention Services: an economic evaluation. 25 November 2009. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_110099.pdf Accessed 22 February 2010
IMS BPI/HPAI. July 2009.
National Institute for Health and Clinical Excellence. (2008c) Guide to the methods of technology appraisal. http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf. Accessed 14 September 2009
National Collaborating Centre for Nursing & Supportive Care. (2008) Osteoporosis: evidence review. Systematic reviews of clinical effectiveness prepared for the guideline “Osteoporosis: assessment of fracture risk and the prevention of osteoporotic fractures in individuals at high risk”. http://www.nice.org.uk/guidance/index.jsp?action=folder&o=42361. Accessed 24 November 2009
Bucher HC, Guyatt GH, Griffith LE, Walter SD (1997) The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 50:683–691
Robinson CM, Royds M, Abraham A, McQueen MM, Court-Brown CM, Christie J (2002) Refractures in patients at least forty-five years old. a prospective analysis of twenty-two thousand and sixty patients. J Bone Joint Surg Am 84-A(9):1528–1533
Bailey K, Ellis C, Majeed A. (2002) Trends in the treatment of osteoporosis and types of drug treatments prescribed in general practice in England and Wales, 1994 to 1998. Health Statistics Quarterly. http://www.statistics.gov.uk/downloads/theme_health/HSQ16.pdf. Accessed 14 September 2009
Kanis JA, Brazier J, Stevenson M, et al. (2002) Treatment of established osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 6(29)
Office for National Statistics (2008) Mortality rates 2001, deaths 2001: rates per 1000 population by age-group and sex in the UK. Taken from Table 6 published in Mortality Statistics, General, 2001 (series DH1 No. 34). http://www.statistics.gov.uk/statbase. Accessed 14 September 2009
Stevenson M, Lloyd JM, De NE (2005) A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Systematic review. Health Technol Assess 9:1–160
Peasgood T, Herrmann K, Kanis JA, Brazier JE (2009) An updated systematic review of health state utility values for osteoporosis related conditions. Osteoporos Int 20(6):853–868
National Institute for Health and Clinical Excellence. (2008d) Osteoporosis—primary prevention: costing template. http://guidance.nice.org.uk/TA160/CostTemplate/xls/English. Accessed 13 November 2009
NHS Cancer Screening Programmes. (2010) About cervical screening. http://www.cancerscreening.nhs.uk/cervical/about-cervical-screening.html#cost. Accessed 15 November 2010
Curtis L. (2009) Unit costs of health and social care 2008. Personal Social Services Research Unit, the University of Kent. http://www.pssru.ac.uk/pdf/uc/uc2008/uc2008.pdf. Accessed 10 March 2009
Department of Health. (2009b) National Reference Costs 2007–08. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_098945. Accessed 12 August 2009
Monthly Index of Medical Specialities, Haymarket Medical Media, London (2010) http://www.mims.co.uk/home/. Accessed 20 January 2010
Stevenson MD, Davis SE, Kanis JA (2006) The hospitalisation costs and out-patient costs of fragility fractures. Womens Health Med 3(4):149–151
Acknowledgements
Funding for this work was provided by Novartis Pharmaceuticals UK Ltd. The authors would like to acknowledge Dr. Christopher Andrews of Novartis Pharmaceuticals UK Ltd for statistical analysis of the West Glasgow refracture data.
Conflicts of interest
AR McLellan has received honoraria (Speaker’s Fees) from Novartis & has participated in advisory boards supported by Novartis. D Roberts and F Adekunle are employees of Novartis Pharmaceuticals UK Ltd and hold shares in the company. Novartis Pharmaceuticals UK Ltd provided funding to RTI Health Solutions to perform the research reported in the manuscript. Novartis Pharmaceuticals UK Ltd is the manufacturer of zoledronic acid 5 mg (also known as zoledronate), one of the osteoporosis treatments mentioned in the manuscript. Novartis Pharmaceuticals UK Ltd provided statistical support for the analysis of anonymised patient level data from the West Glasgow FLS that was provided by Dr AR McLellan.
Author information
Authors and Affiliations
Corresponding author
Additional information
A related editorial can be found at doi:10.1007/s00198-011-1643-9; other related articles at doi:10.1007/s00198-010-1544-y, doi:10.1007/s00198-011-1638-6, and doi:10.1007/s00198-011-1642-x.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online resource
(PDF 187 kb)
Rights and permissions
About this article
Cite this article
McLellan, A.R., Wolowacz, S.E., Zimovetz, E.A. et al. Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22, 2083–2098 (2011). https://doi.org/10.1007/s00198-011-1534-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1534-0