Abstract
Summary
The study aimed to quantify the long-term effects of stroke on tibial bone morphology and hip bone density. Only the trabecular bone mineral density and bone strength index in the hemiparetic tibial distal epiphysis showed a significant decline among individuals who had sustained a stroke 12–24 months ago.
Introduction
This study aims to determine the changes in bone density and morphology in lower limb long bones during a 1-year follow-up period and their relationship to muscle function in chronic stroke patients.
Methods
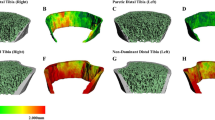
Twenty-eight chronic stroke patients (12–166 months after the acute stroke event at initial assessment) and 27 controls underwent bilateral scanning of the hip and tibia using dual-energy X-ray absorptiometry and peripheral quantitative computed tomography, respectively. Each subject was re-assessed 1 year after the initial assessment.
Results
Twenty stroke cases and 23 controls completed all assessments. At the end of the follow-up, the paretic tibial distal epiphysis suffered significant decline in trabecular bone density (−1.8 ± 0.6 %, p = 0.006) and bone strength index (−2.7 ± 0.6 %, p < 0.001). More severe decline in the former was associated with poorer leg muscle strength (ρ = 0.447, p = 0.048) and motor recovery (ρ = 0.489, p = 0.029) measured at initial assessment. The loss in trabecular bone density remained significant among those whose stroke onset was 12–24 months ago (p < 0.001), but not among those whose stroke onset was beyond 24 months ago (p > 0.05) at the time of initial assessment. The changes of outcomes in the tibial diaphysis, except for cortical bone mineral content on the non-paretic side (−1.3 ± 0.3 %, p = 0.003), and hip bone density were well within the margin of error for precision.
Conclusions
There is evidence of continuous trabecular bone loss in the paretic tibial distal epiphysis among chronic stroke patients, but it tends to plateau after 2 years of stroke onset. The steady state may have been reached earlier in the hip and tibial diaphysis.

Similar content being viewed by others
References
Dennis MS (2002) Fractures after stroke: frequency, types, and associations. Stroke 33:728–734. doi:10.1161/hs0302.103621
Kanis J, Oden A, Johnell O (2001) Acute and long-term increase in fracture risk after hospitalization for stroke. Stroke 32:702–706. doi:10.1161/01.STR.32.3.702
Ramnemark A, Nyberg L, Borssen B et al (1998) Fractures after stroke. Osteoporos Int 630:92–95
Chiu KY, Pun WK, Luk KD, Chow SP (1992) A prospective study on hip fractures in patients with previous cerebrovascular accidents. Injury 23:297–299
Hyndman D, Ashburn A, Stack E (2002) Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil 83:165–170
Ramnemark A, Nyberg L, Lorentzon R et al (1999) Progressive hemiosteoporosis on the paretic side and increased bone mineral density in the nonparetic arm the first year after severe stroke. Osteoporos Int 9:269–275. doi:10.1007/s001980050147
Lazoura O, Groumas N, Antoniadou E et al (2008) Bone mineral density alterations in upper and lower extremities 12 months after stroke measured by peripheral quantitative computed tomography and DXA. J Clin Densitom 11:511–517. doi:10.1016/j.jocd.2008.05.097
Hamdy R, Moore S, Cancellaro B (1995) Long-term effects of strokes on bone mass. Am J Phys Med Rehabil 74:351–356
Ramnemark A, Nyberg L, Lorentzon R et al (1999) Hemiosteoporosis after severe stroke, independent of changes in body composition and weight. Stroke 30:755–760. doi:10.1161/01.STR.30.4.755
De Brito CMM, Garcia ACF, Takayama L et al (2013) Bone loss in chronic hemiplegia: a longitudinal cohort study. J Clin Densitom 16:160–167. doi:10.1016/j.jocd.2012.02.011
Jørgensen L, Jacobsen BK, Wilsgaard T, Magnus JH (2000) Walking after stroke: does it matter? Changes in bone mineral density within the first 12 months after stroke. A longitudinal study. Osteoporos Int 11:381–387. doi:10.1007/s001980070103
Jørgensen L, Jacobsen B (2001) Changes in muscle mass, fat mass, and bone mineral content in the legs after stroke: a 1 year prospective study. Bone 28:655–659
Worthen LC, Kim CM, Kautz SA et al (2005) Key characteristics of walking correlate with bone density in individuals with chronic stroke. J Rehabil Res Dev 42:761. doi:10.1682/JRRD.2005.02.0036
MacIntyre NJ, Rombough R, Brouwer B (2010) Relationships between calf muscle density and muscle strength, mobility and bone status in the stroke survivors with subacute and chronic lower limb hemiparesis. J Musculoskelet Neuronal Interact 10:249–255
Pang MYC, Ashe MC, Eng JJ (2010) Compromised bone strength index in the hemiparetic distal tibia epiphysis among chronic stroke patients: the association with cardiovascular function, muscle atrophy, mobility, and spasticity. Osteoporos Int 21:997–1007. doi:10.1007/s00198-009-1038-3
Talla R, Galea M, Lythgo N et al (2011) Contralateral comparison of bone geometry, BMD and muscle function in the lower leg and forearm after stroke. J Musculoskelet Neuronal Interact 11:306–313
Pang MYC, Ashe MC, Eng JJ (2008) Tibial bone geometry in chronic stroke patients: influence of sex, cardiovascular health, and muscle mass. J Bone Miner Res 23:1023–1030. doi:10.1359/jbmr.080224
Poole KES, Vedi S, Debiram I et al (2009) Bone structure and remodelling in stroke patients: early effects of zoledronate. Bone 44:629–633. doi:10.1016/j.bone.2008.11.017
Sato Y, Kuno H, Kaji M et al (1998) Increased bone resorption during the first year after stroke. Stroke 29:1373–1377. doi:10.1161/01.STR.29.7.1373
Eng JJ, Chu KS, Dawson AS et al (2002) Functional walk tests in individuals with stroke: relation to perceived exertion and myocardial exertion. Stroke 33:756–761
Washburn RA, Smith KW, Jette AM, Janney CA (1993) The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 46:153–162. doi:10.1016/0895-4356(93)90053-4
Kontulainen S, Sievänen H, Kannus P et al (2002) Effect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controls. J Bone Miner Res 17:2281–2289. doi:10.1359/jbmr.2002.17.12.2281
Macdonald H, Kontulainen S, Petit M et al (2006) Bone strength and its determinants in pre- and early pubertal boys and girls. Bone 39:598–608. doi:10.1016/j.bone.2006.02.057
Leonard M, Shore R (2003) Radiologic evaluation of bone mineral in children. In: Favus M (ed) Primer on the metabolic bone disease and disorders of mineral metabolism, 5th edn. American Society for Bone and Mineral Research, Washington, pp 173–189
Stratec Medizintechnik Gmbh (2004) XCT 2000 Manual Software Version 5.50
Ashe MC, Fehling P, Eng JJ et al (2006) Bone geometric response to chronic disuse following stroke: a pQCT study. J Musculoskelet Neuronal Interact 6:226–233
Pang M, Ashe M, Eng J et al (2006) A 19-week exercise program for people with chronic stroke enhances bone geometry at the tibia: a peripheral quantitative computed tomography study. Osteoporos Int 17:1615–1625. doi:10.1007/s00198-006-0168-0
Baim S, Wilson CR, Lewiecki EM et al (2005) Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 8:371–378
Gowland C, Stratford P, Ward M et al (1993) Measuring physical impairment and disability with the Chedoke-McMaster Stroke Assessment. Stroke 24:58–63. doi:10.1161/01.STR.24.1.58
Pandyan AD, Johnson GR, Price CI et al (1999) A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin Rehabil 13:373–383
Yang FZH, Pang MYC (2015) Influence of chronic stroke impairments on bone strength index of the tibial distal epiphysis and diaphysis. Osteoporos Int 26:469–480. doi:10.1007/s00198-014-2864-5
Ahlborg HG, Johnell O, Turner CH et al (2003) Bone loss and bone size after menopause. N Engl J Med 349:327–334. doi:10.1056/NEJMoa022464
Seeman E (2003) Periosteal bone formation—a neglected determinant of bone strength. N Engl J Med 349:320–323. doi:10.1056/NEJMp038101
Pang MYC, Ashe MC, Eng JJ (2007) Muscle weakness, spasticity and disuse contribute to demineralization and geometric changes in the radius following chronic stroke. Osteoporos Int 18:1243–1252. doi:10.1007/s00198-007-0372-6
Pang MYC, Zhang M, Li LSW, Jones AYM (2013) Changes in bone density and geometry of the radius in chronic stroke and related factors: a one-year prospective study. J Musculoskelet Neuronal Interact 13:77–88
Pang MYC, Yang FZH, Jones AYM (2013) Vascular elasticity and grip strength are associated with bone health of the hemiparetic radius in people with chronic stroke: implications for rehabilitation. Phys Ther 93:774–785. doi:10.2522/ptj.20120378
Nakayama H, Jørgensen HS, Raaschou HO, Olsen TS (1994) Compensation in recovery of upper extremity function after stroke: the Copenhagen Stroke Study. Arch Phys Med Rehabil 75:852–857
Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS (1995) Recovery of walking function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil 76:27–32
Pang MYC, Eng JJ, Dawson AS et al (2005) A community-based fitness and mobility exercise program for older adults with chronic stroke: a randomized, controlled trial. J Am Geriatr Soc 53:1667–1674. doi:10.1111/j.1532-5415.2005.53521.x
Borschmann K, Pang MYC, Bernhardt J, Iuliano-Burns S (2012) Stepping towards prevention of bone loss after stroke: a systematic review of the skeletal effects of physical activity after stroke. Int J Stroke 7:330–335. doi:10.1111/j.1747-4949.2011.00645.x
Fleuren JFM, Voerman GE, Erren-Wolters CV et al (2010) Stop using the Ashworth Scale for the assessment of spasticity. J Neurol Neurosurg Psychiatry 81:46–52. doi:10.1136/jnnp.2009.177071
Hsu A-L, Tang P-F, Jan M-H (2003) Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch Phys Med Rehabil 84:1185–1193
Damilakis J, Adams JE, Guglielmi G, Link TM (2010) Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol 20:2707–2714. doi:10.1007/s00330-010-1845-0
Liu XS, Cohen A, Shane E et al (2010) Bone density, geometry, microstructure, and stiffness: relationships between peripheral and central skeletal sites assessed by DXA, HR-pQCT, and cQCT in premenopausal women. J Bone Min Res 25:2229–2238. doi:10.1002/jbmr.111
Acknowledgments
We thank the International Osteoporosis Foundation for their constructive criticisms and assistance in the writing of the parts of the manuscript. F.M.H. Lam was granted a full-time research studentship by the Hong Kong Polytechnic University. F.M.H. Lam was granted a Young Investigator Award from the International Osteoporosis Foundation to present the preliminary results of this study at the 3rd Asia-Pacific Osteoporosis Meeting, Kuala Lumpur, Malaysia, 2012. M.Y.C. Pang was granted a General Research Fund by the Research Grants Council.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Subjects’ characteristics of the subgroups of stroke cases(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Lam, F.M.H., Bui, M., Yang, F.Z.H. et al. Chronic effects of stroke on hip bone density and tibial morphology: a longitudinal study. Osteoporos Int 27, 591–603 (2016). https://doi.org/10.1007/s00198-015-3307-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3307-7