Abstract
Summary
A meta-analysis was conducted to evaluate the prevalence of osteopenia/osteoporosis in human immunodeficiency virus (HIV)-infected individuals. The prevalence of osteopenia/osteoporosis in HIV-infected and antiretroviral therapy (ART)-treated individuals was significantly higher than respective controls. Evidence regarding bone loss within first year of HIV infection or ART initiation was preliminary.
Purpose
The aim of the study is to systematically review published literature on the prevalence of osteopenia/osteoporosis and its associated risk factors in HIV-infected individuals.
Methods
A literature search was conducted from 1989 to 2015 in six databases. Full text, English articles on HIV-infected individuals ≥ 18 years, which used dual X-ray absorptiometry to measure BMD, were included. Studies were excluded if the prevalence of osteopenia/osteoporosis was without a comparison group, and the BMD/T-score were not reported.
Results
Twenty-one cross sectional and eight longitudinal studies were included. The prevalence of osteopenia/osteoporosis was significantly higher in both HIV-infected [odds ratio (OR) = 2.4 (95%Cl: 2.0, 2.8) at lumbar spine, 2.6 (95%Cl: 2.2, 3.0) at hip] and ART-treated individuals [OR = 2.8 (95%Cl: 2.0, 3.8) at lumbar spine, 3.4 (95%Cl: 2.5, 4.7) at hip] when compared to controls. PI-treated individuals had an OR of 1.3 (95%Cl: 1.0, 1.7) of developing osteopenia/osteoporosis compared to controls. A higher proportion of tenofovir-treated individuals (52.6%) had lower BMD compared to controls (42.7%), but did not reach statistical significance (p = 0.248). No significant difference was found in the percent change of BMD at the lumbar spine, femoral neck, or total hip from baseline to follow-up between HIV-infected, PI-treated, tenofovir-treated, and controls. Older age, history of bone fracture, low BMI, low body weight, being Hispanic or Caucasian, low testosterone level, smoking, low CD4 cell count, lipodystrophy, low fat mass, and low lean body mass were associated with low BMD.
Conclusions
The prevalence of osteopenia/osteoporosis in HIV-infected and antiretroviral therapy (ART)-treated individuals was two times more compared to controls. However, evidence concerning bone loss within the first year of HIV infection and ART initiation was preliminary.
Similar content being viewed by others
Introduction
The commencement of antiretroviral therapy (ART) in human immunodeficiency virus (HIV)-infected individuals has significantly reduced their morbidity and mortality [1]. However, HIV infection and the use of ART have been associated with a higher incidence of aging complications, such as osteoporosis [2]. According to the World Health Organization, osteoporosis is diagnosed when T-score is ≤ − 2.5; and osteopenia is diagnosed when T-score is between − 1 and − 2.5. The causes of osteopenia/osteoporosis in HIV-infected individuals are multifactorial, and may be due to a complex interaction between HIV infection, traditional osteoporosis risk factors, and ART factors [3]. If osteoporosis is left untreated, it can lead to fragility fractures.
A meta-analysis by Brown and Qadish, 2006, found that the odds ratio (OR) for HIV-infected individuals to develop osteopenia/osteoporosis was 6.4 times greater than HIV-uninfected individuals, whilst the OR for ART-treated individuals was 2.5 times when compared to ART-naïve individuals [4]. In protease inhibitor (PI)-treated individuals, the OR to develop osteopenia/osteoporosis was 1.5 times greater than PI-untreated individuals [4]. Since then, an additional 13 cross-sectional and 6 longitudinal studies have been published from 2005 till 2015. Therefore, the aim of our meta-analysis was to review published literature on the prevalence of osteopenia/osteoporosis and percent change of bone mineral density (BMD) in HIV-infected, ART-treated, PI-treated, and tenofovir-treated individuals. Factors associated with osteopenia/osteoporosis were also examined.
Materials and methods
Study selection and search strategy
This meta-analysis was registered with PROSPERO (CRD: 42016047294) and conducted according to PRISMA Guidelines (Supplementary material 1: PRISMA checklist). A search was conducted using six databases: MEDLINE, CINAHL, EMBASE, Science Direct, Cochrane, and Web of Science from 1989 till May 2015. A combination of Medical Subject Heading (MESH) and free text terms were used to define the search (“HIV”[MeSH Terms] OR “HIV”[Text Word] OR “Human Immunodeficiency Virus”[Text Word]) AND (“Antiretroviral Therapy, Highly Active”[MeSH Terms] OR “HAART therapy”[Text Word] OR “HIV Protease Inhibitors”[Pharmacological Action] OR ‘tenofovir’) AND (“Osteoporosis”[MeSH Terms] OR “Osteoporosis”[Text Word] OR “Bone Diseases, Metabolic”[MeSH Terms] OR “Bone Density”[MeSH Terms] OR “Bone Density”[Text Word] OR “osteopenia*”[Text Word]) AND (epidemiologic studies”[MeSH Terms] OR “epidemiology”[MeSH Terms] OR “epidemiology”[Text Word]) OR “prevalence”[MeSH Terms] OR “prevalence”[Text Word] OR “incidence”[MeSH Terms] OR “incidence”[Text Word]). The results of the above search strategies were combined to yield a pool of preliminary studies. Reference mining and related citations of potential references were also examined. Duplicated studies with the same title and author were excluded.
Cross-sectional or longitudinal studies published in English, original research articles that used dual-energy X-ray absorptiometry (DXA) to measure BMD on the lumbar spine, femoral neck, or total hip, and compared at least two groups (e.g., HIV-infected versus HIV-uninfected, ART-treated versus ART-naive, PI-treated versus non PI-treated, tenofovir-treated versus non tenofovir-treated individuals), aged ≥ 18 years old, and used a validated conversion equation if BMD were measured using different DXA machines, were included. Longitudinal studies were only included if change in BMD were reported > 12 months from baseline as change in BMD has to be more than the least significant change of the DXA machine (This can only occur 1–2 years from the previous DXA scan) [5]. Studies were excluded if the outcomes of interest (BMD or T-score) were not reported and if the study was only published as an editorial, commentary, brief report, expert opinion, case study, or conference abstracts. Articles that studied HIV and chronic viral hepatitis (Hepatitis B or Hepatitis C co-infection) were also excluded, as a review was recently published in 2014 [6].
Quality assessment and data extraction
The quality of each study was assessed independently by two teams of researchers using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies 2014, developed by the National Institutes of Health, USA [7]. Data were extracted and recorded in a standardized extraction form. When disagreements occurred between the two teams, both teams met and referred back to the original text to clarify the issue that was raised. Once the evidence was highlighted, the two teams then reached a consensus via discussion.
If authors only reported osteopenia/osteoporosis as continuous variables, they were contacted and asked to provide information on the proportion of participants with osteopenia/osteoporosis. Studies were excluded if authors did not provide the required data. The prevalence of osteopenia/osteoporosis included information from cross-sectional and longitudinal studies at baseline. In longitudinal studies, the percent change of BMD from baseline to follow-up was examined.
Outcome and analysis
The primary outcome of this meta-analysis was the prevalence of osteopenia/osteoporosis and percent change of BMD. A fixed effects model was implemented to examine the heterogeneity between studies. Funnel plots were used to investigate for potential publication bias along with Begg’s test. Analyses were conducted using Review Manager (RevMan) Version 5 (Copenhagen, Denmark).
The quality of each study was assessed using the United States Preventative Services Task Force (USPSTF) guideline. A “good” study meets all criteria for that study design; a “fair” study does not meet all criteria but is judged to have no fatal flaw that invalidates its results; and a “poor” study contains a fatal flaw [8]. Strength of evidence regarding the association between risk factors and BMD was analyzed according to Supplementary material 2.
Results
A total of 21 cross-sectional and 8 longitudinal studies met our inclusion criteria (Fig. 1). No publication bias was observed in the funnel plots (Supplementary material 3).
HIV-infected versus HIV-uninfected individuals
Seventeen studies [cross-sectional (n = 14); longitudinal (n = 3)] compared HIV-infected versus HIV-uninfected individuals (Tables 1 and 2) [1, 9,10,11,12,13,14,15,16,17,18,19,20,21,22, 30, 31]. Seven studies only included men [1, 9, 11, 15, 20, 22, 30], four studies only included women [10, 14, 21, 31], while six studies included both men and women [12, 13, 16,17,18,19]. The majority of participants were male (range: 30–86%) [12, 16]. All studies were matched for gender except for three studies [16, 18, 19]. Age and BMI were well matched between HIV-infected versus HIV-uninfected individuals. Three studies recruited only Caucasians [9, 11, 17], nine studies recruited participants of mixed ethnicity [1, 10, 12, 14,15,16, 19, 30, 31], while five studies did not specify the ethnicity group [13, 18, 20,21,22].
Odds ratio of osteopenia/osteoporosis in HIV-infected individuals versus HIV-uninfected individuals
Fourteen cross-sectional studies and one observational longitudinal study were included in this analysis (Table 1a) [1, 9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Two longitudinal studies were excluded as the proportion of osteopenia/osteoporosis at baseline was not reported [30, 31]. The odds of developing osteopenia/osteoporosis at the lumbar spine and hip was OR = 2.4 (95%Cl 2.0, 2.8), p < 0.001 and OR = 2.6 (95%Cl 2.2, 3.0), p < 0.001, respectively (Fig. 2). The overall assessment of heterogeneity between studies for osteopenia/osteoporosis at lumbar spine and hip was I 2 = 83% (Q = 80.7, p < 0.001), and I 2 = 85% (Q = 92.7, p < 0.001), respectively.
Percent change in BMD from baseline to follow-up in HIV-infected individuals versus HIV-uninfected individuals
Two observational longitudinal studies were included in this analysis (Table 2a) [30, 31]. Duration of follow-up ranged from 24 to 72 months [30, 31]. Bone loss only occurred at the total hip from baseline to 12 months [31] and 72 months [30]. However, when a meta-analysis was performed from baseline to 24–72 months, no significant difference was seen at the lumbar spine [OR = 4.4 (95%Cl 0.8, 26.2), p = 0.22] and total hip [OR = 0.6 (95%Cl 0.1, 4.6), p = 0.61] in HIV-infected and HIV-uninfected individuals (Supplementary material 4). The overall assessment of heterogeneity between studies for percent change in BMD analysis at lumbar spine and hip was I 2 = 34% (Q = 1.5, p = 0.16,) and I 2 = 0% (Q = 0.3, p = 0.62,), respectively.
Antiretroviral-treated versus non antiretroviral-treated individuals
Nine studies [cross-sectional (n = 8); longitudinal (n = 1)] compared ART-treated versus non ART-treated individuals (Table 1) [9, 13, 18, 23,24,25,26,27,28]. Five studies only included men [9, 24,25,26, 28], one study only included women [27], while two studies included both men and women [13, 18]. The majority of participants were male (range: 70–91%) [13, 18]. Two studies were not matched for gender [13, 18]. One study recruited only Caucasians [9], while another study recruited both Caucasians and Blacks [27].
Odds ratio of osteopenia/osteoporosis in antiretroviral-treated versus antiretroviral-naive individuals
Eight cross-sectional studies and one observational longitudinal study were included in this analysis (Table 1b) [9, 13, 18, 23,24,25,26,27,28]. The odds of developing osteopenia/osteoporosis at the lumbar spine and hip was OR = 2.8 (95%Cl 2.0, 3.8), p = 0.004 and OR = 3.4 (95%Cl 2.5, 4.7), p = 0.0002, respectively (Fig. 3). The overall assessment of heterogeneity between studies for osteopenia/osteoporosis at lumbar spine and hip was I 2 = 64% (Q = 22.2, p < 0.001) and I 2 = 74% (Q = 30.4, p < 0.001), respectively.
A meta-analysis on the percent change in BMD from baseline to follow-up for ART-treated individuals could not be calculated as there was only one observational longitudinal study [18].
Protease inhibitor-treated versus non protease inhibitor-treated individuals
Eleven studies [cross-sectional (n = 7); longitudinal (n = 4)] compared PI-treated versus non PI-treated individuals (Tables 1 and 2) [13, 18, 20, 24, 25, 27,28,29, 32,33,34]. Of the four longitudinal studies, only one was a randomized controlled trial (RCT) [33]. Four studies only included men [20, 24, 25, 28], one study only included women [27], while six studies included both men and women [13, 18, 29, 32,33,34]. The majority of participants were male (range: 63–96%) [18, 29]. All studies were matched for gender except for five studies [13, 18, 29, 32, 33]. Age and BMI were well matched between PI-treated and non-PI-treated individuals.
Odds ratio of osteopenia/osteoporosis in protease inhibitor-treated versus non protease inhibitor-treated individuals
Seven cross-sectional studies and one observational longitudinal study were included in this analysis (Table 1c) [13, 18, 20, 24, 25, 27,28,29]. Three longitudinal studies were excluded as the proportion of osteopenia/osteoporosis at baseline was not reported [32,33,34]. The odds of developing osteopenia/osteoporosis at the lumbar spine and hip was OR = 1.3 (95%Cl 1.0, 1.8), p = 0.20 and OR = 1.3 (95%Cl 1.0, 1.7), p = 0.17, respectively (Supplementary material 5). The overall assessment of heterogeneity between studies for osteopenia/osteoporosis at lumbar spine and hip was I 2 = 29% (Q = 9.8, p = 0.05) and I 2 = 33% (Q = 10.4, p = 0.07), respectively.
Percent change in BMD from baseline to follow-up in protease inhibitor-treated versus non protease inhibitor-treated individuals
Four longitudinal studies [observational (n = 3); RCT (n = 1)] were included in this analysis (Table 2b) [18, 32,33,34]. The duration of follow-up ranged from 14 to 33 months [18, 33]. Bone loss occurred at both lumbar spine from baseline to 6 [33], 9, 21 [32], and 33 months [33] and at the femur from baseline to 11 [33], 14 [18], and 33 months [33]. However, there was no significant difference between the percent change in BMD at the lumbar spine [OR = 1.1 (95% Cl 0.5, 2.7)], p = 0.70 and femoral neck [OR = 1.2 (95% Cl 0.4, 3.8)], p = 0.53 from baseline to 14–33 months in PI-treated versus non PI-treated individuals (Supplementary material 6). The overall assessment of heterogeneity between studies for percent change in BMD analysis at lumbar spine and hip was I 2 = 0% (Q = 1.5, p = 0.82) and I 2 = 0% (Q = 0.4, p = 0.77), respectively.
Tenofovir-treated versus non tenofovir-treated individuals
Three studies [cross-sectional (n = 1); longitudinal (n = 2] compared tenofovir-treated versus non tenofovir-treated individuals (Tables 1 and 2) [29, 35, 36]. Only one longitudinal study was a RCT [36]. All three studies included both men and women [29, 35, 36]. The majority of the participants were male (ranged 74–99%) [29, 35], and all studies were not matched for gender [29, 35, 36].
Proportion of osteopenia/osteoporosis in tenofovir-treated versus non tenofovir-treated individuals
Only one cross-sectional study was included in this analysis (Table 1d) [29]. Hence, it was not possible to calculate the OR. A higher proportion of tenofovir-treated individuals 30 (52.6%) had osteopenia/osteoporosis compared to non tenofovir-treated individuals 35 (42.7%), but this result was not statistically significant (p = 0.248).
Percent change in BMD from baseline to follow-up at in tenofovir-treated versus non tenofovir-treated individuals
Two longitudinal studies [observational (n = 1); RCT (n = 1)] were included in this analysis (Table 2c) [35, 36]. The duration of follow-up ranged from 22 to 33 months [35, 36]. Bone loss occurred at the lumbar spine and total hip from baseline to 11, 22 [36], and 33 months [35]. However, when a meta-analysis was performed, no significant difference was found between the percent change in BMD at the lumbar spine [OR = 1.0 (95% Cl, 0.2, 5.8)], p = 0.38 and total hip [OR = 1.8 (95% Cl, 0.4, 8.7)], p = 0.71 from baseline to follow-up at 22–33 months in tenofovir-treated versus non tenofovir-treated individuals (Supplementary material 7). The overall assessment of heterogeneity between studies for percent change in BMD analysis at lumbar spine and hip was I 2 = 0% (Q = 0.8, p = 1.00) and I 2 = 0% (Q = 0.14, p = 0.4), respectively.
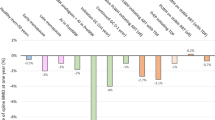
Risk factors for low BMD
Fifteen studies assessed the risk factors associated with low BMD (Table 3) [1, 9,10,11, 14, 16, 17, 23,24,25,26,27, 29, 31, 33]. Thirteen studies were rated as fair quality as they did not perform a sample size calculation [1, 9,10,11, 14, 16, 23,24,25, 27, 29, 31, 33]. Two studies were rated as poor quality as they did not perform any multivariate analysis [17, 26]. Ten risk factors (age, history of bone fracture, BMI, body weight, ethnicity, testosterone level, smoking, lipodystrophy, CD4 cell count, fat mass, and lean body mass) had fair evidence of an association with low BMD, two risk factors (HIV viral load and lactic acid level) had insufficient evidence, while three risk factors (steroid use, opiate use, and vitamin D level) had inconsistent evidence.
Discussion
Our findings from the 21 cross-sectional and 8 longitudinal studies found that odds of developing osteopenia/osteoporosis in HIV-infected and ART-treated individuals were approximately two times more when compared to their respective controls. No significant difference was found in the odds of developing osteopenia/osteoporosis in PI-treated and tenofovir-treated when compared to their respective controls. Older age, history of bone fracture, low BMI, low body weight, being Hispanic or Caucasian, low testosterone level, smoking, low CD4 cell count, lipodystrophy, low fat mass, and low lean body mass were associated with low BMD.
The pathogenesis of bone loss in HIV-infected individual is a complex and multifactorial process. This is probably due to an interaction within the T cells, osteoclast, and osteoblast, which is more apparent in HIV-infected individuals, as well as those on ART [3]. HIV infection increases inflammatory cytokines, which has been thought to increase bone turnover through osteoclast stimulation and bone resorption [37]. Our study found that the odds of developing osteopenia/osteoporosis in HIV-infected individuals were two times lower than a previous meta-analysis [4]. This difference could be due to the additional seven cross-sectional studies [1, 10, 11, 15, 16, 19, 22]. Additionally, we excluded three studies as two studies were brief reports [38, 54] and the other included participants with hepatitis C co-infection [39].
The introduction of ART has increased the life expectancy of HIV-infected individuals [40], but the mechanism of action of ART on bone loss remains controversial [4, 24]. ART-treated individuals were found to have a two times increased risk of developing osteopenia/osteoporosis, which was similar to previous findings [4]. ART has been reported to affect osteoclast and osteoblast activity in vitro [41] and in animals [42]. However, this finding could not be replicated in humans [43]. NRTIs (like abacavir and zidovudine) were found to suppress osteoblast activity [41] and promote osteoclastogenesis/osteoclast activity in animal studies [42].
The proportion of PI-treated and tenofovir-treated individuals with osteopenia/osteoporosis were higher when compare to their respective controls. However, these results did not reach statistical significance, which was similar to previous findings [4]. PIs (like ritonavir) were reported to suppress osteoclastogenesis/osteoclast function in vitro and in vivo studies [44]. Tenofovir was reported to cause proximal renal tubular dysfunction that could result in excessive renal phosphate loss, which then impairs bone mineralization and increased bone turnover leading to bone loss [45].
Our study found that there was no significant difference in the percent change of BMD at the lumbar spine, femoral neck or total hip from baseline to follow-up at 14–33 months between HIV-infected, PI-treated, and tenofovir-treated versus their controls, respectively. Our meta-analysis suggests that bone loss may occur within the first year of HIV infection or ART initiation. Our results were similar to previous studies which reported that 2–6% of bone loss occurred over the first 2 years of ART initiation [3]. However, evidence concerning short-term bone loss may not be as strong as the range of bone loss reported was small (0.1–5.0%) as our findings were based on a small number of studies [46]. This shows that the pattern of bone loss in HIV-infected individuals may be acute and accelerated, while in older people, their bone loss occurs gradually over time as they age [47].
Ideally, results from RCT and observational studies should be analyzed separately as observational studies which recruited ART-treated individuals are more likely to have active disease or complications that may impact on outcome, whereas RCTs match for baseline conditions for both treated individuals and controls. However, it was not possible for us to perform any sub-group analysis based on study design as there were only two RCTs included.
We recommend that HIV-infected and ART–treated individuals should be screened for osteopenia/osteoporosis during the first year of HIV-infection or ART initiation, regardless of age or gender. In HIV-infected individuals aged < 40 years old, DXA scan is recommended as a screening tool for osteopenia/osteoporosis since the Fracture Risk Assessment Tool (FRAX®) can only be used in those aged ≥ 40 years. FRAX should be used to screen for osteopenia/osteoporosis in those ≥ 40 years, as it is the most cost effective method. DXA scan is recommended in HIV-infected: individuals aged ≥ 40 years old who have a FRAX score ≥ 10%; men aged ≥ 50 years, post-menopausal women, individuals with a history of fragility fracture, individuals receiving chronic glucocorticoid treatment, and individuals who are at higher risk of falls as previous recommended [48].
Traditional osteoporosis risk factors play an important role in HIV-infected individuals [49]. However, HIV-infected individuals have additional risk factors such as low fat mass, low lean body mass, lipodystrophy, and low CD4 cells count which contributes to bone loss. Studies found that changes of body composition from HIV infection and complications of ART mimic the normal aging process of older individuals [50]. As a result, HIV-infected individuals are more susceptible to have lower lean body mass and lower fat mass/abnormal body fat redistribution which can lead to bone loss [50]. Both lean body mass and fat mass are independent and significant predictors of BMD [51]. Low lean body mass leads to reduce muscle strength, which can affect bone mass and structure [51]. Lipodystrophy is a medical condition that is characterized by fat loss and/or redistribution of body fat [52]. This disorder is frequently observed in HIV-infected individuals on long term ART [52]. To date, the underlying etiology of low CD4 cell count and bone loss remains unclear. However, it has been suggested that the immune system may play a potential role in skeletal maintenance [53]. Evidence shows HIV-infected individuals with low baseline CD4+ cell count (< 50 cells/mm3) have approximately 3% greater bone loss than HIV-infected individuals with > 500 cells/mm3 [53].
One of the limitations of our study was that we were not able to determine the effect of the individual types of antiretroviral medications on osteopenia/osteoporosis. Secondly, we excluded studies that were published as an editorial, commentary, brief report, expert opinion, case study, or conference abstracts as these reports were not sufficiently detailed enough for us to assess quality and data extract. Lastly, we were not able to utilize Z-score to diagnose osteoporosis in individuals < 50 years, as the majority of the studies included did not present their results as Z-score. The strength of our study was that we performed our search on six databases.
Conclusions
The prevalence of osteopenia/osteoporosis in HIV-infected and ART-treated individuals was approximately two times more compared to controls. Evidence concerning bone loss within the first year of HIV infection and ART initiation was preliminary. Older age, history of bone fracture, low BMI, low body weight, being Hispanic or Caucasian, low testosterone level, smoking, low CD4 cell count, lipodystrophy, low fat mass, and low lean body mass were associated with low BMD.
References
Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Lo Y, Klein RS (2007) Decreased bone mineral density and increased fracture risk in aging men with or at risk for HIV infection. AIDS 21(5):617–623. https://doi.org/10.1097/QAD.0b013e3280148c05
Onen NF et al (2010) Aging and HIV infection: a comparison between older HIV-infected persons and the general population. HIV Clin Trials 11(2):100–109. https://doi.org/10.1310/hct1102-100
McComsey GA, Tebas P, Shane E, Yin MT, Overton ET, Huang JS, Aldrovandi GM, Cardoso SW, Santana JL, Brown TT (2010) Bone disease in HIV infection: a practical review and recommendations for HIV care providers. Clin Infect Dis 51(8):937–946. https://doi.org/10.1086/656412
Brown TT, Qaqish RB (2006) Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 20(17):2165–2174. https://doi.org/10.1097/QAD.0b013e32801022eb
Foundation, N.O. Bone density exam or testing. 2017; Available from: https://www.nof.org/patients/diagnosis-information/bone-density-examtesting/
Dong HV, Cortés YI, Shiau S, Yin MT (2014) Osteoporosis and fractures in HIV/hepatitis C virus coinfection: a systematic review and meta-analysis. AIDS 28(14):2119–2131. https://doi.org/10.1097/QAD.0000000000000363
National Institutes of Health, Quality assessment tool for observational cohort and cross-sectional studies National Institutes of Health, 2014
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D (2001) Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 20(3 Suppl):21–35. https://doi.org/10.1016/S0749-3797(01)00261-6
Amiel C, Ostertag A, Slama L, Baudoin C, N'Guyen T, Lajeunie E, Neit-Ngeilh L, Rozenbaum W, de Vernejoul MC (2004) BMD is reduced in HIV-infected men irrespective of treatment. J Bone Miner Res 19(3):402–409. https://doi.org/10.1359/JBMR.0301246
Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Santoro N, Schoenbaum EE (2006) HIV infection and bone mineral density in middle-aged women. Clin Infect Dis 42(7):1014–1020. https://doi.org/10.1086/501015
Bolland MJ, Grey AB, Horne AM, Briggs SE, Thomas MG, Ellis-Pegler RB, Woodhouse AF, Gamble GD, Reid IR (2006) Bone mineral density is not reduced in HIV-infected Caucasian men treated with highly active antiretroviral therapy. Clin Endocrinol 65(2):191–197. https://doi.org/10.1111/j.1365-2265.2006.02572.x
Brown TT, Ruppe MD, Kassner R, Kumar P, Kehoe T, Dobs AS, Timpone J (2004) Reduced bone mineral density in human immunodeficiency virus-infected patients and its association with increased central adiposity and postload hyperglycemia. J Clinical Endocrinology Metabolism 89(3):1200–1206. https://doi.org/10.1210/jc.2003-031506
Bruera D, Luna N, David DO, Bergoglio LM, Zamudio J (2003) Decreased bone mineral density in HIV-infected patients is independent of antiretroviral therapy. AIDS 17(13):1917–1923. https://doi.org/10.1097/00002030-200309050-00010
Dolan SE, Huang JS, Killilea KM, Sullivan MP, Aliabadi N, Grinspoon S (2004) Reduced bone density in HIV-infected women. AIDS 18(3):475–483. https://doi.org/10.1097/00002030-200402200-00014
Grijsen ML, Vrouenraets SME, Wit FWNM, Stolte IG, Prins M, Lips P, Reiss P, Prins JM (2013) Low bone mineral density, regardless of HIV status, in men who have sex with men. J Infect Dis 207(3):386–391. https://doi.org/10.1093/infdis/jis687
Jones S, Restrepo D, Kasowitz A, Korenstein D, Wallenstein S, Schneider A, Keller MJ (2008) Risk factors for decreased bone density and effects of HIV on bone in the elderly. Osteoporos Int 19(7):913–918. https://doi.org/10.1007/s00198-007-0524-8
Loiseau-Pérès S, Delaunay C, Poupon S, Lespessailles E, Ballouche N, Arsac P, Benhamou CL (2002) Osteopenia in patients infected by the human immunodeficiency virus. A case control study. Joint Bone Spine 69(5):482–485. https://doi.org/10.1016/S1297-319X(02)00433-5
Madeddu G, Spanu A, Solinas P, Calia GM, Lovigu C, Chessa F, Mannazzu M, Falchi A, Mura MS, Madeddu G (2004) Bone mass loss and vitamin D metabolism impairment in HIV patients receiving highly active antiretroviral therapy. Quarterly J Nuclear Medicine Molecular Imaging 48(1):39–48
Negredo E, Domingo P, Ferrer E, Estrada V, Curran A, Navarro A, Isernia V, Rosales J, Pérez-Álvarez N, Puig J, Bonjoch A, Echeverría P, Podzamczer D, Clotet B (2014) Peak bone mass in young HIV-infected patients compared with healthy controls. Jaids-J Acquired Immune Deficiency Syndromes 65(2):207–212. https://doi.org/10.1097/01.qai.0000435598.20104.d6
Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, Yarasheski KE (2000) Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS 14(4):F63–F67. https://doi.org/10.1097/00002030-200003100-00005
Teichmann J, Stephan E, Lange U, Discher T, Friese G, Lohmeyer J, Stracke H, Bretzel RG (2003) Osteopenia in HIV-infected women prior to highly active antiretroviral therapy. J Infect 46(4):221–227. https://doi.org/10.1053/jinf.2002.1109
Teichmann J, Lange U, Discher T, Lohmeyer J, Stracke H, Bretzel RG (2009) Bone mineral density in human immunodeficiency virus-1 infected men with hypogonadism prior to highly-active-antiretroviral-therapy (HAART). Eur J Med Res 14(2):59–64. https://doi.org/10.1186/2047-783X-14-2-59
Aydın OA, Karaosmanoglu HK, Karahasanoglu R, Tahmaz M, Nazlıcan O (2013) Prevalence and risk factors of osteopenia/osteoporosis in Turkish HIV/AIDS patients. Braz J Infect Dis 17(6):707–711. https://doi.org/10.1016/j.bjid.2013.05.009
Carr A, Miller J, Eisman JA, Cooper DA (2001) Osteopenia in HIV-infected men: association with asymptomatic lactic acidemia and lower weight pre-antiretroviral therapy. AIDS 15(6):703–709. https://doi.org/10.1097/00002030-200104130-00005
de Menezes Barbosa EG et al (2013) Impact of antiretroviral therapy on bone metabolism markers in HIV-seropositive patients. Bone 57(1):62–67. https://doi.org/10.1016/j.bone.2013.07.019
Garcia Aparicio AM et al (2006) Abnormalities in the bone mineral metabolism in HIV-infected patients. Clin Rheumatol 25(4):537–539. https://doi.org/10.1007/s10067-005-0028-x
Libois A, Clumeck N, Kabeya K, Gerard M, de Wit S, Poll B, Tondeur M, Rozenberg S (2010) Risk factors of osteopenia in HIV-infected women: no role of antiretroviral therapy. Maturitas 65(1):51–54. https://doi.org/10.1016/j.maturitas.2009.10.009
Tomazic J et al (2007) Prevalence and risk factors for osteopenia/osteoporosis in an HIV-infected male population. Wien Klin Wochenschr 119(21–22):639–646. https://doi.org/10.1007/s00508-007-0844-x
Calmy A, Fux CA, Norris R, Vallier N, Delhumeau C, Samaras K, Hesse K, Hirschel B, Cooper DA, Carr A (2009) Low bone mineral density, renal dysfunction, and fracture risk in HIV infection: a cross-sectional study. J Infect Dis 200(11):1746–1754. https://doi.org/10.1086/644785
Bolland MJ, Grey A, Horne AM, Briggs SE, Thomas MG, Ellis-Pegler RB, Gamble GD, Reid IR (2012) Stable bone mineral density over 6 years in HIV-infected men treated with highly active antiretroviral therapy (HAART). Clin Endocrinol 76(5):643–648. https://doi.org/10.1111/j.1365-2265.2011.04274.x
Dolan SE, Kanter JR, Grinspoon S (2006) Longitudinal analysis of bone density in human immunodeficiency virus-infected women. J Clin Endocrinol Metab 91(8):2938–2945. https://doi.org/10.1210/jc.2006-0127
Bonnet E et al (2013) Early loss of bone mineral density is correlated with a gain of fat mass in patients starting a protease inhibitor containing regimen: the prospective Lipotrip study. BMC Infect Dis 13(293):1–10
Hansen AB, Obel N, Nielsen H, Pedersen C, Gerstoft J (2011) Bone mineral density changes in protease inhibitor-sparing vs. nucleoside reverse transcriptase inhibitor-sparing highly active antiretroviral therapy: data from a randomized trial. HIV Medicine 12(3):157–165. https://doi.org/10.1111/j.1468-1293.2010.00864.x
Mondy K, Yarasheski K, Powderly WG, Whyte M, Claxton S, DeMarco D, Hoffmann M, Tebas P (2003) Longitudinal evolution of bone mineral density and bone markers in human immunodeficiency virus-infected individuals. Clin Infect Dis 36(4):482–490. https://doi.org/10.1086/367569
Gallant JE, Staszewski S, Pozniak AL, DeJesus E, Suleiman JM, Miller MD, Coakley DF, Lu B, Toole JJ, Cheng AK, 903 Study Group et al (2004) Efficacy and safety of tenofovir DF vs stavudine in combination therapy in antiretroviral-naive patients: a 3-year randomized trial. J Am Med Assoc 292(2):191–201. https://doi.org/10.1001/jama.292.2.191
Haskelberg H et al (2012) Changes in bone turnover and bone loss in HIV-infected patients changing treatment to tenofovir-emtricitabine or abacavir-lamivudine. PLoS One 7(6):1–9
Fakruddin JM, Laurence J (2003) HIV envelope gp120-mediated regulation of osteoclastogenesis via receptor activator of nuclear factor kappa B ligand (RANKL) secretion and its modulation by certain HIV protease inhibitors through interferon-gamma/RANKL cross-talk. J Biol Chem 278(48):48251–48258. https://doi.org/10.1074/jbc.M304676200
Knobel H, Guelar A, Vallecillo G, Nogués X, Díez A (2001) Osteopenia in HIV-infected patients: is it the disease or is it the treatment? AIDS 15(6):807–808. https://doi.org/10.1097/00002030-200104130-00022
Yin M, Dobkin J, Brudney K, Becker C, Zadel JL, Manandhar M, Addesso V, Shane E (2005) Bone mass and mineral metabolism in HIV plus postmenopausal women. Osteoporos Int 16(11):1345–1352. https://doi.org/10.1007/s00198-005-1845-0
Nakagawa F, May M, Phillips A (2013) Life expectancy living with HIV: recent estimates and future implications. Curr Opin Infect Dis 26(1):17–25. https://doi.org/10.1097/QCO.0b013e32835ba6b1
Taylor A, Rogers M HIV treatments and the skeleton: do NRTIs directly effect bone cells? Bone 46:S56
Pan G, Wu X, McKenna MA, Feng X, Nagy TR, McDonald JM (2004) AZT enhances osteoclastogenesis and bone loss. AIDS Res Hum Retrovir 20(6):608–620. https://doi.org/10.1089/0889222041217482
Ofotokun I, Weitzmann MN (2011) HIV and bone metabolism. Discov Med 11(60):385–393
Wang MW et al (2004) The HIV protease inhibitor ritonavir blocks osteoclastogenesis and function by impairing RANKL-induced signaling. J Clin Invest 114(2):206–213. https://doi.org/10.1172/JCI15797
Walker Harris V, Brown TT (2012) Bone loss in the HIV-infected patient: evidence, clinical implications, and treatment strategies. J Infect Dis 205(Suppl 3):S391–S398. https://doi.org/10.1093/infdis/jis199
Davey J, Turner RM, Clarke MJ, Higgins JPT (2011) Characteristics of meta-analyses and their component studies in the Cochrane database of systematic reviews: a cross-sectional, descriptive analysis. BMC Med Res Methodol 11(1):160. https://doi.org/10.1186/1471-2288-11-160
Clarke BL, Khosla S (2010) Physiology of bone loss. Radiol Clin N Am 48(3):483–495. https://doi.org/10.1016/j.rcl.2010.02.014
Brown TT, Hoy J, Borderi M, Guaraldi G, Renjifo B, Vescini F, Yin MT, Powderly WG (2015) Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis 60(8):1242–1251. https://doi.org/10.1093/cid/civ010
Chiţu-Tișu C-E, Barbu EC, Lazăr M, Ion DA, Bădărău IA (2016) Low bone mineral density and associated risk factors in HIV-infected patients. Germs 6(2):50–59. 10.11599/germs.2016.1089
Erlandson KM, Allshouse AA, Jankowski CM, MaWhinney S, Kohrt WM, Campbell TB (2013) Functional impairment is associated with low bone and muscle mass among persons aging with HIV-infection. J Acquired Immune Deficiency Syndromes (1999) 63(2):209–215. https://doi.org/10.1097/QAI.0b013e318289bb7e
Shapses SA, Sukumar D (2012) Bone metabolism in obesity and weight loss. Annu Rev Nutr 32(1):287–309. https://doi.org/10.1146/annurev.nutr.012809.104655
Fiorenza CG, Chou SH, Mantzoros CS (2011) Lipodystrophy: pathophysiology and advances in treatment. Nat Rev Endocrinol 7(3):137–150. https://doi.org/10.1038/nrendo.2010.199
Grant PM, Kitch D, McComsey GA, Dube MP, Haubrich R, Huang J, Riddler S, Tebas P, Zolopa AR, Collier AC, Brown TT (2013) Low baseline CD4+ count is associated with greater bone mineral density loss after antiretroviral therapy initiation. Clin Infect Dis 57(10):1483–1488. https://doi.org/10.1093/cid/cit538
Huang JS, Mulkern RV, Grinspoon S (2002) Reduced intravertebral bone marrow fat in HIV-infected men. AIDS 16(9):1265–1269. https://doi.org/10.1097/00002030-200206140-00009
Acknowledgements
We would like to thank Ranita Bt. Hisham Shunmugam (medical librarian) for her assistance in designing comprehensive search strategies for this meta-analysis.
Funding
Funding for this study was obtained from the University of Malaya High Impact Research Grants for Malaysian Elderly Longitudinal Research group, MELOR (UM0000099/HIR.C3), Malaysia: HIV & Ageing group, MHIVA (H-20001-00-E000091 and Postgraduate Research Grant (PG197-2015B).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Goh, S.S.L., Lai, P.S.M., Tan, A.T.B. et al. Reduced bone mineral density in human immunodeficiency virus-infected individuals: a meta-analysis of its prevalence and risk factors. Osteoporos Int 29, 595–613 (2018). https://doi.org/10.1007/s00198-017-4305-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4305-8