Abstract
Summary
Bone remodeling markers (BRMs) are suppressed following the consumption of a meal. Our findings indicate that a single session of continuous moderate-intensity exercise, but not low-volume high-intensity interval exercise, performed 1 h after a meal attenuates the postprandial suppression of BRMs.
Introduction
Acute exercise transiently increases BRMs including osteocalcin (tOC) and the undercarboxylated form of osteocalcin (ucOC), a hormone that is implicated in glucose regulation. The effects of acute exercise and exercise-intensity on postprandial levels of tOC and ucOC are unknown.
Methods
Twenty-seven adults that were overweight or obese (age 30 ± 1 years; BMI 30 ± 1 kg∙m−2; mean ± SEM) were randomly allocated to perform a single session of low-volume high-intensity interval exercise (LV-HIIE; nine females, five males) or continuous moderate-intensity exercise (CMIE; eightfemales, five males) 1 h after consumption of a standard breakfast. Serum tOC, ucOC, and ucOC/tOC were measured at baseline, 1 h, and 3 h after breakfast consumption on a rest day (no exercise) and the exercise day (exercise 1 h after breakfast).
Results
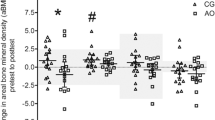
Compared to baseline, serum tOC and ucOC were suppressed 3 h after breakfast on the rest day (− 10 ± 1% and − 6 ± 2%, respectively; p < 0.05), whereas ucOC/tOC was elevated (2.5 ± 1%; p = 0.08). Compared to the rest day, CMIE attenuated the postprandial-induced suppression of tOC (rest day − 10 ± 2% versus CMIE − 5 ± 2%, p < 0.05) and ucOC (rest day − 6 ± 4% versus CMIE 11 ± 2%, p < 0.05), and increased postprandial ucOC/tOC (rest day 3 ± 2% versus CMIE 15 ± 1%, p < 0.05). In contrast, LV-HIIE did not alter postprandial tOC, ucOC, or ucOC/tOC (all p > 0.1).
Conclusions
Acute CMIE, but not LV-HIIE, attenuates the postprandial-induced suppression of tOC and ucOC. CMIE may be an effective tool to control the circulating levels of BRMs following meal consumption in overweight/obese adults.




Similar content being viewed by others
References
Parfitt AM, Travers R, Rauch F, Glorieux FH (2000) Structural and cellular changes during bone growth in healthy children. Bone 27(4):487–494
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130(3):456–469. https://doi.org/10.1016/j.cell.2007.05.047
Levinger I, Brennan-Speranza TC, Zulli A, Parker L, Lin X, Lewis JR, Yeap BB (2017) Multifaceted interaction of bone, muscle, lifestyle interventions and metabolic and cardiovascular disease: role of osteocalcin. Osteoporos Int 28(8):2265–2273. https://doi.org/10.1007/s00198-017-3994-3
Brennan-Speranza TC, Conigrave AD (2015) Osteocalcin: an osteoblast-derived polypeptide hormone that modulates whole body energy metabolism. Calcif Tissue Int 96(1):1–10. https://doi.org/10.1007/s00223-014-9931-y
Fernandez-Real JM, Izquierdo M, Ortega F, Gorostiaga E, Gomez-Ambrosi J, Moreno-Navarrete JM, Fruhbeck G, Martinez C, Idoate F, Salvador J, Forga L, Ricart W, Ibanez J (2009) The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab 94(1):237–245. https://doi.org/10.1210/jc.2008-0270
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Kurioka S, Yano S, Sugimoto T (2009) Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab 94(1):45–49. https://doi.org/10.1210/jc.2008-1455
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S, Sugimoto T (2011) Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass in type 2 diabetes mellitus. Osteoporos Int 22(1):187–194. https://doi.org/10.1007/s00198-010-1184-7
Zhou B, Li H, Liu J, Xu L, Guo Q, Zang W, Sun H, Wu S (2016) Autophagic dysfunction is improved by intermittent administration of osteocalcin in obese mice. Int J Obes 40(5):833–843. https://doi.org/10.1038/ijo.2016.1
Paldanius PM, Ivaska KK, Hovi P, Andersson S, Vaananen HK, Kajantie E, Makitie O (2012) The effect of oral glucose tolerance test on serum osteocalcin and bone turnover markers in young adults. Calcif Tissue Int 90(2):90–95. https://doi.org/10.1007/s00223-011-9551-8
Lopes LS, Schwartz RP, Ferraz-de-Souza B, da Silva ME, Correa PH, Nery M (2015) The role of enteric hormone GLP-2 in the response of bone markers to a mixed meal in postmenopausal women with type 2 diabetes mellitus. Diabetol Metab Syndr 7:13. https://doi.org/10.1186/s13098-015-0006-7
Levinger I, Seeman E, Jerums G, McConell GK, Rybchyn MS, Cassar S, Byrnes E, Selig S, Mason RS, Ebeling PR, Brennan-Speranza TC (2016) Glucose-loading reduces bone remodeling in women and osteoblast function in vitro. Physiol Rep 4(3):e12700. https://doi.org/10.14814/phy2.12700
Iglesias P, Arrieta F, Pinera M, Botella-Carretero JI, Balsa JA, Zamarron I, Menacho M, Diez JJ, Munoz T, Vazquez C (2011) Serum concentrations of osteocalcin, procollagen type 1 N-terminal propeptide and beta-CrossLaps in obese subjects with varying degrees of glucose tolerance. Clin Endocrinol 75(2):184–188. https://doi.org/10.1111/j.1365-2265.2011.04035.x
Jiao H, Xiao E, Graves DT (2015) Diabetes and its effect on bone and fracture healing. Curr Osteoporos Rep 13(5):327–335. https://doi.org/10.1007/s11914-015-0286-8
Levinger I, Jerums G, Stepto NK, Parker L, Serpiello FR, McConell GK, Anderson M, Hare DL, Byrnes E, Ebeling PR, Seeman E (2014) The effect of acute exercise on undercarboxylated osteocalcin and insulin sensitivity in obese men. J Bone Miner Res 29(12):2571–2576. https://doi.org/10.1002/jbmr.2285
Levinger I, Zebaze R, Jerums G, Hare DL, Selig S, Seeman E (2011) The effect of acute exercise on undercarboxylated osteocalcin in obese men. Osteoporos Int 22(5):1621–1626. https://doi.org/10.1007/s00198-010-1370-7
Parker L, Lin X, Garnham A, McConell G, Stepto NK, Hare DL, Byrnes E, Ebeling PR, Seeman E, Brennan-Speranza TC, Levinger I (2018) Glucocorticoid-induced insulin resistance in men is associated with suppressed undercarboxylated osteocalcin. J Bone Miner Res 0 (ja). doi:https://doi.org/10.1002/jbmr.3574
Levinger I, Brennan-Speranza TC, Jerums G, Stepto NK, Serpiello FR, McConell GK, Anderson M, Hare DL, Byrnes E, Ebeling PR, Seeman E (2015) The effect of hyperinsulinaemic-euglycaemic clamp and exercise on bone remodeling markers in obese men. Bonekey Rep 4:731. https://doi.org/10.1038/bonekey.2015.100
Gibala MJ, Little JP, Macdonald MJ, Hawley JA (2012) Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol 590(5):1077–1084. https://doi.org/10.1113/jphysiol.2011.224725
Parker L, Shaw CS, Banting L, Levinger I, Hill KM, McAinch AJ, Stepto NK (2016) Acute low-volume high-intensity interval exercise and continuous moderate-intensity exercise elicit a similar improvement in 24-h glycemic control in overweight and obese adults. Front Physiol 7(661):661. https://doi.org/10.3389/fphys.2016.00661
Ryder JR, Ball SD (2012) Three-dimensional body scanning as a novel technique for body composition assessment: a preliminary investigation. J Exerc Physiol Online 15(1):1
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO (1990) A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 51(2):241–247. https://doi.org/10.1093/ajcn/51.2.241
Council NHaMR (2014) Acceptable macronutrient distribution ranges for macronutrients to reduce chronic disease risk whilst still ensuring adequate micronutrient status. https://www.nrv.gov.au/chronic-disease/summary. 2016
Gundberg CM, Nieman SD, Abrams S, Rosen H (1998) Vitamin K status and bone health: an analysis of methods for determination of undercarboxylated osteocalcin. J Clin Endocrinol Metab 83(9):3258–3266. https://doi.org/10.1210/jcem.83.9.5126
Clowes JA, Hannon RA, Yap TS, Hoyle NR, Blumsohn A, Eastell R (2002) Effect of feeding on bone turnover markers and its impact on biological variability of measurements. Bone 30(6):886–890
Marliss EB, Vranic M (2002) Intense exercise has unique, effects on both insulin release and its roles in glucoregulation—implications for diabetes. Diabetes 51:S271–S283. https://doi.org/10.2337/diabetes.51.2007.S271
Parker L, Trewin A, Levinger I, Shaw CS, Stepto NK (2017) The effect of exercise-intensity on skeletal muscle stress kinase and insulin protein signaling. PLoS One 12(2):e0171613. https://doi.org/10.1371/journal.pone.0171613
Clowes JA, Robinson RT, Heller SR, Eastell R, Blumsohn A (2002) Acute changes of bone turnover and PTH induced by insulin and glucose: euglycemic and hypoglycemic hyperinsulinemic clamp studies. J Clin Endocrinol Metab 87(7):3324–3329. https://doi.org/10.1210/jcem.87.7.8660
Poole DC, Jones AM (2017) Measurement of the maximum oxygen uptake Vo2max: Vo2peak is no longer acceptable. J Appl Physiol (1985) 122(4):997–1002. https://doi.org/10.1152/japplphysiol.01063.2016
Acknowledgements
Thank you to Prof. John Hawley, Prof. Helena Teede, Dr. Christos Stathis, Dr. Karen Hill, Dr. Lauren Banting, Prof. Andrew McAinch, and Dr. Matthew Cooke, for your contribution to the research. Thank you to all the participants who were involved in the research.
Funding
A/Prof Levinger was supported by Future Leader Fellowship (ID: 100040) from the National Heart Foundation of Australia. Dr. Parker was supported by an Alfred Deakin Postdoctoral Fellowship. This work is supported by the Australian Government Collaborative Research Network (CRN) awarded to the authors LP, CSS, NKS, and IL.
Author information
Authors and Affiliations
Contributions
LP, CSS, NKS, and IL contributed to the study design and acquirement of ethical approval. LP and CSS contributed to data collection. EB performed biochemical analysis of serum osteocalcin and uncarboxylated osteocalcin. LP statistically analyzed the data and drafted the initial manuscript. The remaining authors critically revised the manuscript. All authors approved the final version of the manuscript. LP is the guarantor of the manuscript and takes full responsibility for the work as a whole, including the study design, access to data, and the decision to submit and publish the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Nigel K. Stepto and Itamar Levinger are co-senior author.
Electronic supplementary material
ESM 1
(DOCX 15.2 kb)
Rights and permissions
About this article
Cite this article
Parker, L., Shaw, C.S., Byrnes, E. et al. Acute continuous moderate-intensity exercise, but not low-volume high-intensity interval exercise, attenuates postprandial suppression of circulating osteocalcin in young overweight and obese adults. Osteoporos Int 30, 403–410 (2019). https://doi.org/10.1007/s00198-018-4719-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4719-y