Abstract
Summary
Knowledge about risk factors of mortality after hip fracture might encourage prevention and further improvements in care. This study identified patient risk factors as well as hospital and regional characteristics associated with a decreased risk. Variation of mortality was largest on patient level and modest on hospital and regional level.
Introduction
Among numerous studies analyzing mortality as worst consequence after hip fracture, the majority focused on patient level and fewer on hospital and regional level. Comprehensive knowledge about contributing factors on all levels might help to reveal relevant inequalities, which would encourage prevention and further improvements in care. This study aimed at investigating variation of mortality after hip fracture on patient, hospital, and regional level in Germany.
Methods
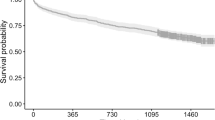
We performed a retrospective cohort study on hip fracture patients aged 65 and older using statutory health insurance claims data from Jan 2009 through Dec. 2012 and additional information from the Federal Statistical Office Germany. Regions were classified based on two-digit postal code. We applied a multilevel Cox proportional hazard model with random intercepts on hospital and regional level to investigate the risk factors for mortality within 6 and 12 months after hip fracture.
Results
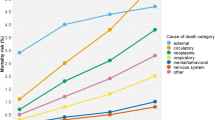
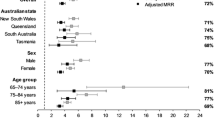
The dataset contained information on 123,119 hip fracture patients in 1014 hospitals in 95 German regions. Within 6/12 months, 20.9%/27.6% of the patients died. On patient level, male sex, increasing age, increased pre-fracture care level, and increasing comorbidity were associated with an increased hazard of mortality. Hospitals with increasing hip fracture volume or with orthogeriatric co-management and regions with increased population density were associated with a decreased hazard. Variation was largest on patient level and rather modest on hospital and regional level.
Conclusions
The identification of patient-related risk factors enables prognosticating mortality after hip fracture. After adjusting for those, variation seemed to be attributable rather to hospitals than to regions.



Similar content being viewed by others
References
Kanis JA, Odén A, McCloskey E, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Weller I, Wai EK, Jaglal S, Kreder HJ (2005) The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg 87:361–366
Bottle A, Aylin P (2006) Mortality associated with delay in operation after hip fracture: observational study. Br Med J 332:947–951
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43:676–685
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing 43:464–471
Sheehan K, Sobolev B, Chudyk A, Stephens T, Guy P (2016) Patient and system factors of mortality after hip fracture: a scoping review. BMC Musculoskelet Disord 17:166
Malik AT, Panni UY, Masri BA, Noordin S (2018) The impact of surgeon volume and hospital volume on postoperative mortality and morbidity after hip fractures: a systematic review. Int J Surg 54:316–327
Augurzky B, Hentschker C, Pilny A, Wübker A (2017) Krankenhausreport 2017. In Barmer (ed) Schriftenreihe zur Gesundheitsanalyse. Barmer, Siegburg
Zeltzer J, Mitchell RJ, Toson B, Harris IA, Ahmad L, Close J (2014) Orthogeriatric services associated with lower 30-day mortality for older patients who undergo surgery for hip fracture. Med J Aust 201:409–411
Forni S, Pieralli F, Sergi A, Lorini C, Bonaccorsi G, Vannucci A (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66:13–17
Kristensen PK, Thillemann TM, Søballe K, Johnsen SP (2015) Can improved quality of care explain the success of orthogeriatric units? A population-based cohort study. Age Ageing 45:66–71
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39:1157–1163
Romley JA, Jena AB, Goldman DP (2011) Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med 154:160–167
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL (2003) The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med 138:288–298
Medin E, Goude F, Melberg HO, Tediosi F, Belicza E, Peltola M (2015) European regional differences in all-cause mortality and length of stay for patients with hip fracture. Health Econ 24(Suppl 2):53–64
Rogowski J, Jain AK, Escarce JJ (2007) Hospital competition, managed care, and mortality after hospitalization for medical conditions in California. Health Serv Res 42:682–705
Hakkinen U, Rosenqvist G, Iversen T, Rehnberg C, Seppala TT (2015) Outcome, use of resources and their relationship in the treatment of AMI. Stroke and Hip Fracture at European Hospitals Health Economics 24(Suppl 2):116–139
Federal Statistical Office Germany (2011) Verzeichnis der Krankenhäuser und Vorsorge- oder Rehabilitationseinrichtungen in Deutschland. Krankenhausverzeichnis. Statistische Ämter des Bundes und der Länder, Wiesbaden
Federal Statistical Office Germany (2012) Daten aus dem Gemeindeverzeichnis. Postleitregionen mit regionaler Zugehörigkeit nach Fläche und Bevölkerung. Gebietsstand: 31.12.2011. Statistische Ämter des Bundes und der Länder, Wiesbaden
Deutsches Institut für Medizinische Dokumentation und Information (2017) Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme. 10. Revision. German Modification. Deutschen Institut für Medizinische Dokumentation und Information (DIMDI) im Auftrag des Bundesministeriums für Gesundheit (BMG), Köln
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47:626–633
Cox D (1972) Regression models and life-tables (with discussion). J R Stat Soc 34:187–220
Hess KR (1995) Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat Med 14:1707–1723
Schoenfeld D (1980) Chi-squared goodness-of-fit tests for the proportional hazards regression model. Biometrika 67:145–153
Therneau TM, Grambsch PM (2013) Modeling survival data: extending the Cox model. Springer Science & Business Media, New York
Neuhaus JM, Kalbfleisch JD (1998) Between-and within-cluster covariate effects in the analysis of clustered data Biometrics 638-645
Sjölander A, Lichtenstein P, Larsson H, Pawitan Y (2013) Between–within models for survival analysis. Stat Med 32:3067–3076
Austin PC, Wagner P, Merlo J (2017) The median hazard ratio: a useful measure of variance and general contextual effects in multilevel survival analysis. Stat Med 36:928–938
Hox JJ, Moerbeek M, van de Schoot R (2010) Multilevel analysis: techniques and applications. Routledge
Sundmacher L, Gaskins MD, Hofmann K, Busse R (2012) Spatial distribution of avoidable cancer deaths in Germany. J Public Health 20:279–288
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) (2015) S2e-Leitlinie 012/001: Schenkelhalsfraktur des Erwachsenen. https://www.awmf.org/uploads/tx_szleitlinien/012-001l_S2e_Schenkelhalsfraktur_2015-10_01.pdf Accessed 10.01.2019 2019
Lagerros YT, Hantikainen E, Michaëlsson K, Ye W, Adami H-O, Bellocco R (2017) Physical activity and the risk of hip fracture in the elderly: a prospective cohort study. Eur J Epidemiol 32:983–991
Acknowledgments
We thank Christian Günster and Jürgen-Bernhard Adler from WIdO for their support in providing the data.
Funding
This study was funded by the German Federal Ministry of Education and Research (grant 01EC1404E) within the project “Prevention and Rehabilitation of Osteoporotic Fractures in Disadvantaged Populations 2” (PROFinD2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standards and informed consent
The study was approved by the ethics committee of the Ulm University (application number 178/15). For this type of study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schulz, C., König, HH., Rapp, K. et al. Analysis of mortality after hip fracture on patient, hospital, and regional level in Germany. Osteoporos Int 31, 897–904 (2020). https://doi.org/10.1007/s00198-019-05250-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05250-w