Abstract
Rationale
Schizophrenia has been linked to dysregulation of dopamine and glutamate transmitter systems. Attempts to model aspects of schizophrenia in animals have made use of treatments that primarily affect dopaminergic (e.g., amphetamine, Amp) and glutamatergic (e.g., phencyclidine, PCP) function. In addition to exerting short-term acute effects, these agents also induce long-term effects, as seen, for example, in neurochemical and behavioural sensitization.
Objectives
The goal of this work was to compare Amp- and PCP-sensitized states on two measures of information processing that are impaired in schizophrenia, prepulse inhibition (PPI) of the acoustic startle reflex and latent inhibition (LI).
Methods
Rats received injections of Amp, PCP or saline 3 days per week for 3 weeks. The Amp dose increased from 1 to 3 mg/kg, at the rate of 1 mg/kg each week. The PCP dose was 3 mg/kg throughout. After various periods of withdrawal rats were tested for PPI and LI.
Results
Repeated intermittent treatment with Amp or PCP resulted in augmented locomotor responses to challenge with each drug, providing an operational index that sensitization had occurred. Rats sensitized to Amp showed disrupted PPI when tested drug free at 3, 21 and 60 days of withdrawal. Amp-sensitized rats also showed abolition of the LI effect. Rats sensitized to PCP did not show deficits in any of these behaviours when tested drug free.
Conclusions
Because disrupted PPI and LI have both been reported in schizophrenic patients, these results suggest that the Amp-sensitized state may represent a useful model for investigating the neural bases of information processing deficits in schizophrenia.
Similar content being viewed by others
Introduction
The most enduring hypothesis of the neurobiological basis of schizophrenia is that this disorder involves aberrant functioning of dopamine (DA)-containing neural pathways. Specifically, the DA hypothesis of schizophrenia proposes that the psychotic symptoms of the disorder result from hyperactivity of the mesolimbic dopaminergic system (see review by Abi-Dargham and Moore 2003). Although most authorities agree that the DA dysregulation is perhaps the final common pathway, several authors propose a primary role for an alteration in glutamatergic transmission (Carlsson and Carlsson 1990; Javitt and Zukin 1991; Olney and Farber 1995; Coyle 1996). Thus, two kinds of animal models have evolved to study psychosis: amphetamine-based models that are thought to model the final-common-pathway pathophysiology of dopaminergic abnormality and the phencyclidine (PCP, or other NMDA receptor antagonist)-related models that are thought to model the glutamate pathology (Jentsch and Roth 1999; Tsai and Coyle 2002; Laruelle 2000; Castner and Goldman-Rakic 2003; Laruelle et al. 2003).
In humans, chronic intermittent use of amphetamine (Amp) can result in a de novo psychosis (Sato et al. 1992) and administration of Amp to patients with residual symptoms leads to a psychotic exacerbation (Angrist et al. 1985). Whereas originally it was thought that Amp psychosis only reflects the positive symptoms of the illness, a very large-scale naturalistic study of psychostimulant-induced psychosis shows that patients display both positive and negative symptoms—and there is emerging evidence of cognitive abnormalities as well (Srisurapanont et al. 2003).
In animals, repeated intermittent injection of Amp results in augmented neurochemical and behavioural responses to subsequent challenges with Amp (e.g., Robinson and Becker 1986). This process of Amp sensitization has been suggested to be a potentially useful model for some aspects of schizophrenia, and indeed sensitization of dopaminergic function has been proposed to be a core pathophysiological process that leads to schizophrenia (Akiyama et al. 1994; Laruelle 2000; Lieberman et al. 1997; Ujike 2002). In support of these suggestions we recently reported that rats sensitized to Amp using a regimen of intermittent, escalating doses coupled with several weeks of withdrawal, showed both neurochemical and behavioural characteristics that are seen in some schizophrenic individuals (Tenn et al. 2003). Firstly, sensitized rats showed a greater displacement of [3H]raclopride binding after amphetamine challenge than did control rats. Secondly, Amp-sensitized rats showed reduced prepulse inhibition (PPI) of the acoustic startle reflex, a response that is thought to reflect sensorimotor gating, and that is deficient in some schizophrenic individuals (Braff et al. 1992, 2001).
A behaviour that has been used to model cognitive impairments in schizophrenia is latent inhibition. Latent inhibition (LI) is the process whereby preexposure to a stimulus retards conditioning to that stimulus when it is subsequently paired with reinforcement (Lubow 1997). Disrupted LI occurs in some schizophrenic individuals (Baruch et al. 1988) and is also disrupted by acute injections of Amp in rats (Solomon et al. 1981; Solomon and Staton 1982; Warburton et al. 1994; Weiner et al. 1988). Some previous reports indicated that Amp-sensitized rats show reduced LI when tested drug free (Murphy et al. 2001b; Russig et al. 2002). However, this group has also reported enhanced LI resulting from Amp sensitization (Murphy et al. 2001a). The reasons for these opposite effects of Amp sensitization on LI are not clear but may relate to differences in the dosing regimen of Amp between the various studies. Indeed, numerous studies of Amp sensitization indicate that a greater sensitised response accrues from schedules involving intermittent injections given every few days, rather than continuously or even daily (Kolta et al. 1985; Nelson and Ellison 1978; Post 1980; Robinson 1984; Robinson and Becker 1986).
Like Amp, NMDA receptor antagonists, such as PCP or ketamine can worsen psychotic symptoms in patients with schizophrenia and can also induce psychosis in nonschizophrenic individuals (Javitt and Zukin 1991; Lahti et al. 1995). Like Amp, repeated administration of PCP also induces sensitization to the motor stimulant effects of subsequent challenges with PCP (Greenberg and Segal 1985; Johnson et al. 1998; Phillips et al. 2001; Scalzo and Holson 1992; Xu and Domino 1994). Jentsch and colleagues have reported that subchronic treatment with PCP, which presumably leads to a PCP-sensitized state, results in behavioural and neurochemical changes that reflect reduced activity of DA in the prefrontal cortex and enhanced subcortical DA activity (Jentsch et al. 1997, 1998a,b; Jentsch and Roth 1999). This has led to the proposal that withdrawal from repeated PCP treatment may model some of the deficits observed in schizophrenia.
Given this background, the overall aim of these studies was to compare the Amp-sensitized state and the PCP-sensitized state as putative animal models of some of the information processing deficits seen in schizophrenia. Sensitization regimens were chosen that yielded evidence of Amp- or PCP-induced sensitization as measured by augmented locomotor activation in response to the respective drug challenge. Having established suitable drug treatment regimens, we examined the impact of sensitizing with Amp and PCP on PPI of the acoustic startle reflex, and on LI measured in active avoidance and conditioned taste aversion (CTA) procedures.
Materials and methods
Animals
Adult male Sprague–Dawley rats, weighing 200–225 g at the start of the experiment, were used. They were housed two per cage with free access to food and water. The housing room was maintained at a constant temperature of 20±2°C on a 12:12 reverse light/dark cycle. Lights were off at 8:00 a.m.
Amp/PCP treatment
Rats were randomly assigned to one of three groups with each rat receiving an intraperitoneal injection of d-amphetamine sulphate (Amp; Sigma RBI), phencyclidine hydrochloride (PCP; Health and Welfare Canada) or 0.9% saline (Sal; 1 ml/kg). Injections were given three times per week on Mondays, Wednesdays and Fridays for 3 weeks for a total of nine injections. The Amp dose was increased weekly from 1 mg/kg in the first week to 3 mg/kg in the third. PCP-pretreated rats received 3 mg/kg for each injection.
Apparatus
Prepulse inhibition
Testing was conducted in six startle chambers (SR Lab, San Diego Instruments, San Diego, CA). Each chamber consisted of a Plexiglas cylinder (8.2 cm in diameter and 20 cm long) mounted on a platform. A piezoelectric accelerometer, attached to the bottom of the platform, detected and transduced the motion within the cylinder; a computer interfaced with the startle apparatus then recorded the signals. Each startle chamber was mounted in a ventilated enclosure with a speaker located 24 cm above the cylinder that provided the auditory stimuli.
Locomotor activity
The activity boxes were standard clear Plexiglas housing cages (27×48×20 cm). A row of six photocell detectors was placed along the long axis of the cage, positioned 3 cm above the floor. A computer was used to detect and record the number of photobeam interruptions. Rats were given two habituation sessions before drug treatment and three sessions during withdrawal. For these habituation sessions the rats were placed in the activity boxes for a period of 90 min.
Two-way avoidance
Rats were trained and tested in two-way active avoidance boxes (Med Associates) set in a sound- and light-attenuating ventilated shell. Each box measured 64×21×30 cm wide; the boxes were divided into two compartments of equal size by a partition with an opening 9 cm wide and 8 cm high. The opening was 6 cm above the grid floor. The grid floor consisted of 40 stainless steel rods with a diameter of 0.48 cm, spaced 1.5 cm apart through which scrambled foot shock was delivered by a constant-current shock generator and scrambler (Model ENV-412). The position of the rat was detected by activation of microswitches affixed to the grid floor. Illumination was provided by a house light. White noise was produced by a speaker mounted on the ceiling of the ventilated shell above the centre of the shuttle box.
Experimental procedures
Experiment 1: effect of Amp and PCP on PPI and locomotor activity
Forty-eight rats were used; 16 were assigned to receive Sal injections, 16 were assigned to the escalating dose regimen of Amp, and 16 received treatment with PCP (see Table 1). Testing for PPI began by placing rats in the startle apparatus for a 10-min acclimatization period; a 65-dB background of white noise was present throughout. After this period, subjects were presented with a series of five startle pulse (110 db) alone trials. This series of stimuli was followed by 64 randomized trials consisting of no pulse (0 dB, no additional stimuli other than the background noise were presented), a startle pulse (110 db, 40 ms) or three prepulse intensities (70, 75, and 80 db, 20 ms) presented alone or 100 ms preceding a startle pulse. Finally, another series of five startle pulse alone trials were presented. The time between trials ranged from 10 to 20 s. The startle response was measured every 1 ms for a 100-ms period from the onset of the startle stimulus. The percent PPI was calculated by the following formula: % PPI=100−(P+S/S)×100, where P+S is the mean response amplitude for prepulse plus startle pulse trials and S is the mean response amplitude for the startle pulse alone trials. All rats were tested four times. The first test examined the effects of an injection of Amp, PCP or saline on PPI. This test was administered on the last day of the sensitization regimen and began 15 min after the injection. Thus, PPI was measured after treatment with Sal, 3 mg/kg Amp or 3 mg/kg PCP. The remaining three tests assessed changes in PPI as a function of the length of withdrawal period after the sensitizing regimens of Amp and PCP. These tests were conducted on days 3, 21 and 60 of withdrawal.
A test for locomotor activity was carried out on withdrawal day 25. The rats were allowed to habituate to the activity boxes for 30 min. Each of the three groups (Sal-, PCP- and Amp-pretreated rats) were further divided into two subgroups and challenged with either Amp (0.5 mg/kg i.p.) or PCP (1.5 mg/kg i.p.) and the activity was measured for 1 h. A second locomotor activity test was conducted on withdrawal day 65; the rats were counterbalanced for the drug challenge (i.e., the rats that received PCP on day 25 were administered Amp on day 65 and vice versa) and their activity recorded.
Experiment 2: effect of Amp and PCP on latent inhibition of conditioned avoidance response and conditioned taste aversion
Forty-eight rats were used; 16 received saline injections, 16 were assigned to the escalating dose regimen of Amp and 16 received treatment with PCP (see Table 2). The effect of Amp and PCP withdrawal on LI of conditioned avoidance response was examined on withdrawal days 28–34. The method was similar to that of Russig et al. (2002). The procedure was conducted over 3 days. On days 1 and 2, 8 rats from each group were preexposed to both a white noise (80 dB) and the apparatus (preexposed; PE) and the other 8 to only the apparatus (non-preexposed; NPE). The PE rats received 50 presentations of the white noise with a duration of 10 s and a mean intertrial interval of 50 s (range, 10–90 s). The NPE rats were placed in the apparatus with the house light on with no other stimuli present. The total number of crossings during the sessions was recorded. On the third day, each rat was placed into the apparatus and received 100 avoidance test trials. Each trial started with 10 s of white noise followed by 2 s of continuous (0.8 mA) shock with the white noise remaining on with the shock. If the rat entered the other side of the chamber within the 10-s period, the noise was terminated and no shock was delivered (an avoidance response). If the rat moved to the other side during the shock period, this terminated both the shock and the noise (an escape response). If the rat failed to cross during the time of the shock, the noise and shock were terminated after 12 s (a failed response).
The effect of Amp and PCP withdrawal on LI of a conditioned taste aversion was examined on withdrawal days 48–58 with half of the rats trained and tested on days 48–52, and half on days 54–58. The procedure was similar to that of Ellenbroek et al. (1997). Rats were water deprived overnight before the beginning of the experiment. For 5 days, rats were individually placed into a test cage that had two “Bio-Serve Liquid diet” tubes for 1 h. On days 1 to 3, eight rats from each group were given access to tubes containing 5% sucrose solution (PE) and the other eight were given access tap water (NPE). On the fourth day (conditioning), each rat had access to Liquid diet tubes containing the sucrose solution for 1 h. Immediately, after the 60-min period, the rats received an injection of lithium chloride (0.15 M in 4 ml/kg of dH2O, i.p.). On the 5th day (test day) rats received two Liquid diet tubes, one of the tubes containing sucrose solution and the other containing tap water. The tubes were weighed before and after the 1-h drinking period to determine the amount of liquid consumed. Sucrose preference was assessed by calculating the percentage of sucrose consumed on test day relative to the total liquid consumed on that day.
Results
Experiment 1: effects of Amp and PCP on locomotor activity and PPI
Locomotor activity
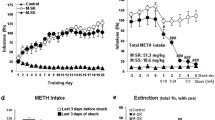
After 25 days of drug withdrawal, rats were tested for their locomotor response to a challenge of either 0.5 mg/kg Amp or 1.5 mg/kg PCP (Fig. 1). A three-way ANOVA using group, drug challenge, and time as factors revealed a main effect of drug challenge [F(1,42)=27.49, p<0.001], a main effect of group [F(2,42)=131.26, p<0.001] and a drug challenge×group interaction [F(2,42)=44.72, p<0.001]. Compared with Sal controls rats pretreated with Amp showed a significant increase in locomotor activity in response to a challenge with Amp (p<0.001). However, PCP-sensitized rats showed no difference in activity from controls when challenged with Amp (p>0.05). When challenged with PCP, both Amp-sensitized and PCP-sensitized rats showed an elevation of activity compared with saline controls (p<0.001). This “asymmetrical” cross-sensitization was still evident after 65 days of drug withdrawal (data not shown).
The effects of PCP and Amp on locomotor activity in rats previously sensitized to phencyclidine (PCP), amphetamine (Amp) or saline (Sal). a Total activity counts are shown after an acute challenge of PCP (1.5 mg/kg) or Amp (0.5 mg/kg) after 25 days withdrawal. b Data (from a) shown as activity counts during the 60 min after the drug challenges. Values are mean±SEM for eight rats per group. *Significantly different from Sal animals challenged with PCP. #Significantly different from Sal animals challenged with Amp
Effects of an acute injection of Amp or PCP on the acoustic startle response and PPI
The startle magnitudes after an acute treatment with 3 mg/kg PCP or 3 mg/kg Amp were analysed by two-way ANOVA (treatment×prepulse intensity). There was an effect of treatment [F(2,45)=4.84, p<0.05), an effect of prepulse intensity [F(3,135)=550.84, p<0.001] and a significant treatment×prepulse intensity interaction [F(6,10)=10.45, p<0.001]. Post hoc comparisons (Tukey’s test) showed no differences in the response to the 110-dB startle stimulus (pulse alone) between any of the treatment groups. Acute treatment with PCP or Amp significantly reduced the startle response during the 70- and 75-dB prepulse–pulse stimulus trials (p<0.001, Fig. 2a). Analysis of PPI scores revealed a main effect of treatment [F(2,45)=37.2, p<0.001], a main effect of prepulse stimulus [F(2,90)=526.2, p<0.001] and a significant treatment×prepulse stimulus interaction [F(4,90)=13.8, p<0.001]. Post hoc comparisons showed that an injection of PCP or Amp reduced PPI levels at the 70- and 75-dB prepulse intensities (p<0.001, Fig. 2b).
Effects of saline (Sal), phencyclidine (PCP) or amphetamine (Amp) on startle response magnitude (a) and PPI of acoustic startle (b). PCP (3 mg/kg) and Amp (3 mg/kg) were injected 15 min before the test was carried out. These injections represent the last treatment of the sensitization regimens. Values are mean±SEM for 16 rats per group. *p<0.01, significantly different from Sal group at the 70- and 75-dB prepulse stimuli
Effects of 3, 21 and 60 days Amp and PCP withdrawal on the acoustic startle response and PPI
Analysis of the startle responses made by the rats after 3 days of withdrawal revealed an effect of prepulse intensity [F(3,135=708.0, p<0.001] and a treatment×prepulse intensity interaction [F(6,135)=2.29, p<0.05]. Post hoc comparisons showed that neither PCP nor Amp altered startle amplitude on the 110-dB pulse-alone trials. During the 70-dB prepulse stimulus trials, only rats in the Amp group had a significantly higher startle response as compared with the other two groups (p<0.001, Fig. 3a). Analysis of PPI scores showed a main effect of treatment [F(2,45)=5.84, p<0.01], a main effect of prepulse intensity [F(2,90)=409.8, p<0.001] and a treatment×prepulse intensity interaction [F(4,90)=3.09, p<0.05]. PCP-sensitized rats showed no disruption of PPI at any prepulse intensity; however, Amp pretreatment significantly reduced PPI at the 70-dB prepulse intensity (p<0.001).
Effects of sensitizing regimens of phencyclidine (PCP), amphetamine (Amp) or saline (Sal) on startle response magnitude (left) and PPI of acoustic startle (right). Testing was conducted on (a) day 3, (b) day 21 and (c) day 60 of drug withdrawal. Values are mean±SEM for 16 rats per group. *p<0.01, significantly different from saline group at the 70-dB stimuli
Analysis of the startle responses after 21 days of withdrawal showed no effect of treatment but a main effect of prepulse intensity [F(3,135=715.6, p<0.001] and a treatment×prepulse intensity interaction [F(6,135)=2.69, p<0.05]. Post hoc comparisons revealed that PCP- and Amp-treated rats did not show altered startle amplitude on the 110-dB pulse-alone trials. However, Amp-sensitized rats showed significantly higher startle response during the 70-dB prepulse–pulse trials (p<0.001, Fig. 3b). Analyses of the PPI scores showed a treatment effect [F(2,45)=6.82, p<0.01], prepulse stimulus intensity effect [F(2,90)=595.7, p<0.001] and a significant treatment×prepulse stimulus intensity interaction [F(4,90)=4.70, p<0.01]. PPI scores were significantly reduced in the Amp-sensitized rats at the 70-dB intensity (p<0.001). PCP pretreatment did not alter PPI at any prepulse intensity.
Analysis of the startle responses at 60 days of withdrawal showed an effect of prepulse intensity [F(3,135=881.7, p<0.001] and a treatment×prepulse intensity interaction [F(6,135)=2.63, p<0.05]. Post hoc comparison confirmed that Amp and PCP treatment did not alter startle response to the 110-dB stimulus; the Amp-sensitized rats showed greater startle responses compared with the control group during the 70-dB prepulse–pulse trials (p<0.01, Fig. 3c). Analyses of the PPI scores showed a treatment effect [F(2,45)=6.51, p<0.01], a prepulse intensity effect [F(2,90)=886.6, p<0.001] and a significant treatment×prepulse stimulus intensity interaction [F(4,90)=6.52, p<0.01]. Again the PPI scores were reduced in the Amp-sensitized rats and this effect was observed only at the 70-dB prepulse stimulus intensity (p<0.001).
Experiment 2: effects of Amp and PCP withdrawal on LI
Conditioned avoidance response
A 3×2×2 (pretreatment×day×preexposure) ANOVA of the number of crossings made on the two preexposure days revealed only an effect of day [F(1,42)=19.5, p<0.001]. This reflects the fact that rats made significantly more crossings on day 1 as compared with day 2 (see Table 3). Post hoc comparison showed that the Amp PE group made fewer crossings than all other groups on day 1 of the preexposure sessions (p<0.01). There was no difference in crossings between the six groups on the second preexposure day (p>0.05).
The mean percentage avoidance responses made during each block of ten trials on the test day for the PE and NPE groups in the three pretreatment conditions are shown in Fig. 4a. A 3×2×10 (group×preexposure×trial blocks) ANOVA was used to analyze the avoidance responses. In general, NPE groups made significantly more avoidance responses than PE groups [F(1,42)=128.9, p<0.001], and responding increased over blocks [F(9,378)=45.5, p<0.001]. The overall three-way interaction between group×preexposure×blocks was significant [F(18,378)=2.75, p<0.001]. This interaction can be attributed to the increase in avoidance response in the NPE condition relative to the PE condition, in saline- [F(9,126)=16.75, p<0.001] and PCP-treated groups [F(9,126)=3.73, p<0.001], but not in Amp-treated groups [F(9,126)=1.69, p=0.98]. Put simply, the saline and PCP groups showed latent inhibition of the acquisition of avoidance responding, but this latent inhibition was not observed in Amp-treated groups. Figure 4b shows the same data collapsed over the factor of blocks and clearly demonstrate the two-way interaction between drug treatment and preexposure condition. Post hoc analyses using Tukey’s test confirmed a significant difference between responding in the PE and NPE groups for the Sal- and PCP-pretreated rats (p<0.001) but not for the Amp-pretreated rats (p=0.238). The disruption of LI in the Amp-pretreated rats was due to the increase in avoidance responses made by the PE group.
Effects of sensitizing regimens of phencyclidine (PCP), amphetamine (Amp) or saline (Sal) on avoidance responses made during 100 test trials in the conditioned avoidance paradigm. Animals had previously experienced either the apparatus alone (non-preexposed group, NPE) or the apparatus and an 80-dB white noise (preexposed group, PE). Data are shown as averages of ten blocks of ten trials each (a) and as the average total percent avoidance for the 100 test trials (b). Values are mean±SEM for eight rats per group. *p<0.001, significant differences between PE and NPE groups
During the conditioned avoidance test PE rats made significantly more intertrial crossings than NPE rats [F(1,42)=78.9, p<0.0001]. The three groups of rats did not differ from each other as shown by the lack of a significant main effect of group [F(2,42)=1.34, p>0.2] and the lack of an interaction between group and preexposure condition [F(2,42)=0.18, p>0.8].
Conditioned taste aversion
Table 4 shows the effects of PCP and Amp withdrawal on liquid consumption over 4 days. The first 3 days of fluid intake was analysed by a 3×3×2 (group×day×preexposure) ANOVA. There was an effect of day [F(2,63)=13.3, p<0.001] and of preexposure [F(1,63)=21.7, p<0.001] but no effect of group on the overall liquid consumption. Fluid intake increased over days for all six groups with the PE groups drinking more than the NPE groups. A 3×2 (treatment×preexposure) ANOVA on sucrose consumption on the fourth day (conditioning session) revealed a main effect of preexposure [F(1,21)=17.1, p<0.001]. Rats previously exposed to the sucrose solution consumed slightly more than those rats that had their first exposure on the conditioning day. Again, PCP and Amp had no effect on the overall liquid consumption.
Figure 5 shows the effects of PCP and Amp treatment withdrawal on sucrose preference on the test day. A two-way ANOVA showed main effects of group [F(2,42)=7.89, p<0.001] and preexposure [F(1,42)=202.39, p<0.001] as well as a group×preexposure interaction [F(2,42)=58.52, p<0.001]. Post hoc Tukey’s test revealed the Sal and PCP PE groups showed a significantly higher preference for sucrose solution than their NPE counterparts (p<0.001). In contrast, the Amp-sensitized rats showed no significant difference in the amount of sucrose solution consumed whether they were previously exposed to sucrose or not (p>0.05).
Effects of sensitizing regimens of phencyclidine (PCP) , amphetamine (Amp) or saline (Sal) on sucrose preference made during the test period, subsequent to conditioning of a taste aversion. Some animals were previously preexposed (PE) to sucrose; the remaining animals were not preexposed to sucrose (NPE). Values are mean±SEM for eight rats per group. *p<0.001, significant difference between PE and NPE groups
Discussion
Repeated, intermittent injections of Amp and PCP resulted in the development of drug-induced locomotor sensitization, implying that the treatment with Amp and PCP induced long-lasting neuroadaptive and functional changes. However, while Amp produced schizophrenia-like deficits in PPI as well as LI in active avoidance and taste aversion tests, repeated PCP did not.
The results of experiment 1 replicated our previous findings that rats sensitized to Amp show reduced PPI, in the absence of any effect on basal startle reactivity (Tenn et al. 2003). Although the PPI disruption was smaller than when Amp was injected just before testing, the effect was still observed at 3, 21 and 60 days of withdrawal, suggesting that it is a robust and relatively enduring response. The Amp-sensitized state also abolished the latent inhibition (or slowed learning) of a conditioned avoidance response in rats preexposed to the conditioned stimulus (CS) that was subsequently used to signal shock onset. When first introduced to the test cages, the Amp-sensitized rats made fewer spontaneous shuttles between the two compartments as compared with controls. However, on the day of the test Amp sensitization did not alter the number of intertrial shuttles during the CAR testing phase. Thus, changes in general activity level do not account for the abolition of LI in the Amp-sensitized rats. These same rats also showed disrupted LI of a CTA. In control rats, preexposure to a sucrose solution attenuated the acquisition of a subsequent CTA after pairing of sucrose ingestion with LiCl. The Amp-sensitized rats showed a strong CTA regardless of the preexposure condition; thus preexposure to sucrose did not diminish the strength of an acquired taste aversion in these rats. Amp-sensitized rats were no different from controls on measures of fluid intake during either preexposure or conditioning sessions, indicating that the effect of Amp sensitization to disrupt LI cannot be attributed to basal changes in unconditioned fluid intake.
The two LI (CAR and CTA) test procedures have quite different features, including the use of two dissimilar behaviours (locomotion and drinking), different unconditioned stimuli (UCS) and of multiple (CAR) vs single (CTA) conditioning trials. The effects of Amp sensitization on LI are independent of the type of task used to assess LI, indicating that Amp sensitization induces a deficiency in a fundamental cognitive process. At present there is a lack of agreement over the nature of the cognitive process that underlies LI and that is presumed to be dysfunctional when LI is altered. Various theories have been proposed to account for LI suggesting altered attentional mechanisms, altered CS–UCS associability, or altered switching between behavioural states (Escobar et al. 2002; Lubow 1997; Weiner 2003). The present data do not shed any light on these competing theories. However, because disrupted LI may be a useful indicator of cognitive deficits in schizophrenia, the generalization of the effects of Amp sensitization to disrupt LI in different tasks indicates that Amp sensitization may be useful for modelling this aspect of schizophrenia.
Previous studies have failed to show disruption of PPI in Amp-sensitized animals (Druhan et al. 1998; Murphy et al. 2001a,b; Russig et al. 2002). A striking feature of these studies is the variety in methods used to induce sensitization particularly regarding the dose of Amp and the frequency of injections. Two of these studies used 1.5 mg/kg on five consecutive days (Murphy et al. 2001a) and 2 mg/kg every 3 days for six injections (Druhan et al. 1998). The strength of sensitization, as indexed by shifts in the magnitude of locomotor stimulant effects of a challenge dose of Amp, seem to differ across these various schedules. For example, although Druhan et al. (1998) found a leftward shift in the Amp dose–response curve, there appeared to be little evidence of sensitization to a challenge dose of 0.5 mg/kg. Similarly, although the rats used by Murphy et al. (2001a) showed enhanced responses to an Amp challenge of 1.5 mg/kg these effects were reported as being not statistically significant. These small effects are in contrast with the robust (250%) increase in Amp-stimulated activity observed with our rats. Although it is difficult to make accurate comparisons across studies that used different methods for measuring locomotion, it seems the degree to which Amp sensitization disrupts PPI may be related to the magnitude of sensitization induced by the drug.
Other studies of the impact of Amp sensitization on PPI used an escalating dose regimen that is superficially similar to the one used in the present experiment. However, in these previous studies Amp was injected three times a day for 6 days for a total of 80 mg/kg of Amp (Murphy et al. 2001b; Russig et al. 2002). This contrast with the total dose of 18 mg/kg used in the present studies and that was administered once every few days over a period of 15 days. This higher dose regimen also failed to disrupt PPI measured after withdrawal periods of 4 to 60 days. Again, it is possible that the two regimens of Amp exposure resulted in differing degrees of sensitization. These earlier studies did not provide a direct measure of the strength of sensitization induced by Amp treatment, such as Amp-induced locomotion. Murphy et al. (2001b) reported that their escalating dose regimen of Amp disrupted LI after 4 and 13 days of withdrawal, but that the effect had begun to wane by the 28th day. In contrast, we found strong disruption of LI at 28 days of withdrawal. These different results suggest that the escalating dose schedule with intermittent injections that we used may induce a more robust, or at least, more enduring level of sensitization than the regimen used by others (Murphy et al. 2001b).
The PCP-treated rats showed disrupted PPI when tested immediately after a PCP injection, and also demonstrated a sensitized locomotor response to a challenge with PCP. However, these rats did not show any evidence of altered PPI or LI. An earlier study reported disrupted PPI in rats tested after nine daily injections with another NMDA receptor antagonist, dizocilpine, but that effect was context dependent and was seen in rats that received injections in the startle apparatus and not in the home cage (Schulz et al. 2001). Our results, however, are consistent with those of Martinez et al. (1999) who found normal PPI responses in rats receiving a variety of regimens of chronic or subchronic exposure to PCP. Regarding LI, some (Schroeder et al. 1998), but not all (Weiner and Feldon 1992), previous studies have reported disruption of LI after treatment with PCP during conditioning and/or preexposure phases. The data presented here show that LI is normal in PCP-sensitized rats when tested after a long withdrawal period. Taken together, all of these studies illustrate that while PPI and LI are disrupted by PCP when testing is conducted under the influence of the drug, the neuroadaptive changes induced by repeated exposure to PCP are insufficient to alter the expression of these behaviours when tested in a drug-free state. This stands in marked contrast to the effects of Amp as reported here and elsewhere.
Both PPI and LI are disrupted by increases in DA neuronal activity (Solomon et al. 1981; Solomon and Staton 1982; Warburton et al. 1994; Weiner et al. 1988). The Amp-sensitized state reflects a hyperactivity of mesocorticolimbic DA systems (Robinson and Becker 1986), and this likely contributes to the disruptions of PPI and LI in Amp-sensitized rats. The regimen of PCP administration used here blunted the locomotor response to Amp. Two previous studies using four daily injections of 2.5 or 15 mg/kg PCP report the same blunting of the locomotor stimulant effect of Amp (Greenberg and Segal 1985; Turgeon and Case 2001). The results of these two studies, taken together with the present results, are consistent in demonstrating that PCP exposure does not necessarily lead to the development of sensitization of the mesolimbic DA system, at least as inferred from changes in response to the stimulant effect of Amp. The different effects of Amp vs PCP sensitization on PPI and LI may thus reflect the development of DA-dependent sensitization vs DA-independent sensitization, respectively. However, it should be noted that unlike the results reported here and elsewhere, Jentsch et al. (1998a) found that PCP-treated rats showed an enhanced response to an Amp challenge. In that case, 5 mg/kg PCP was administered twice a day for 7 days, with testing conducted after 1 week of withdrawal. The reasons why this regimen of PCP, but not others, leads to apparent behavioural sensitization of the mesolimbic DA pathway are not clear. However, as with Amp these disparate outcomes between different experiments illustrate the need to carefully consider the parameters of drug exposure in models of sensitization.
In summary, our results indicate that rats sensitized to Amp showed disruption of PPI and of LI in two quite different learning tasks. In contrast, PCP-sensitized rats showed normal PPI and LI. Given that disrupted PPI and LI are features of schizophrenia our results suggest that the Amp-sensitized state may provide a useful model for understanding the neural mechanisms that may be dysfunctional in the illness.
References
Abi-Dargham A, Moore H (2003) Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist 9:404–416
Akiyama K, Kanzaki A, Tsuchida K, Ujike H (1994) Methamphetamine-induced behavioral sensitization and its implications for relapse of schizophrenia. Schizophr Res 12:251–257
Angrist B, Peselow E, Rubinstein M, Wolkin A, Rotrosen J (1985) Amphetamine response and relapse risk after depot neuroleptic discontinuation. Psychopharmacology 85:277–283
Baruch I, Hemsley DR, Gray JA (1988) Differential performance of acute and chronic schizophrenics in a latent inhibition task. J Nerv Ment Dis 176:598–606
Braff DL, Grillon C, Geyer MA (1992) Gating and habituation of the startle reflex in schizophrenic patients. Arch Gen Psychiatry 49:206–215
Braff DL, Geyer MA, Swerdlow NR (2001) Human studies of prepulse inhibition of startle: normal subjects, patient groups, and pharmacological studies. Psychopharmacology (Berl) 156:234–258
Carlsson M, Carlsson A (1990) Interaction between glutamatergic and monoaminergic systems within the basal ganglia-implications for schizophrenia and Parkinson’s disease. Trends Neurosci 13:272–276
Castner SA, Goldman-Rakic PS (2003) Amphetamine sensitization of hallucinatory–like behaviours is dependent on prefrontal cortex in nonhuman primates. Biol Psychiatry 54:105–110
Coyle JT (1996) The glutamatergic dysfunction hypothesis for schizophrenia. Harv Rev Psychiatry 3:241–253
Druhan JP, Geyer MA, Valentino RJ (1998) Lack of sensitization to the effects of d-amphetamine and apormorphine on sensorimotor gating in rats. Psychopharmacology 135:296–304
Ellenbroek BA, Knobbout DA, Cools AR (1997) The role of mesolimbic and nigrostriatal dopamine in latent inhibition as measured with the conditioned taste aversion paradigm. Psychopharmacology (Berl) 129:112–120
Escobar M, Oberling P, Miller RR (2002) Associative deficit accounts of disrupted latent inhibition and blocking in schizophrenia. Neurosci Biobehav Rev 26:203–216
Greenberg BD, Segal DS (1985) Acute and chronic behavioural interactions between phencyclidine (PCP) and amphetamine: evidence for a dopaminergic role in some PCP-induced behaviors. Pharmacol Biochem Behav 23:99–105
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of model of schizophrenia. Am J Psychiatry 148:1301–1308
Jentsch JD, Roth RH (1999) The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20:201–225
Jentsch JD, Elsworth JD, Redmond DE Jr, Roth RH (1997) Phencyclidine increases forebrain monoamine metabolism in rats and monkeys: modulation by the isomers of HA966. J Neurosci 17:1769–1775
Jentsch JD, Taylor JR, Roth RH (1998a) Subchronic phencyclidine administration increases mesolimbic dopaminergic system responsivity and augments stress- and psychostimulant-induced hyperlocomotion. Neuropsychopharmacology 19:105–113
Jentsch JD, Tran A, Taylor JR, Roth RH (1998b) Prefrontal cortical involvement in phencyclidine-induced activation of the mesolimbic dopamine system: behavioural and neurochemical evidence. Psychopharmacology (Berl) 138:89–95
Johnson KM, Phillips M, Wang C, Kevetter GA (1998) Chronic phencyclidine induces behavioral sensitization and apoptotic cell death in the olfactory and piriform cortex. J Neurosci Res 52:709–722
Kolta MG, Shreve P, De Souza V, Uretsky NJ (1985) Time course of the development of the enhanced behavioral and biochemical responses to amphetamine after pretreatment with amphetamine. Neuropharmacology 24:823–829
Lahti AC, Holcomb HH, Medoff DR, Tamminga CA (1995) Ketamine activates psychosis and alters limbic blood flow in schizophrenia. NeuroReport 6:869–872
Laruelle M (2000) The role of endogenous sensitization in the pathophysiology of schizophrenia: implications from recent brain imaging studies. Brain Res Rev 31:371–384
Laruelle M, Kegeles LS, Abi-Dargham A (2003) Glutamate, dopamine and schizophrenia. Ann N Y Acad Sci 1003:138–158
Lieberman JA, Sheitman BB, Kinon BJ (1997) Neurochemical sensitization in the pathophysiology of schizophrenia: deficits and dysfunction in neuronal regulation and plasticity. Neuropsychopharmacology 17:205–229
Lubow RE (1997) Latent inhibition as a measure of learned inattention: some problems and solutions. Behav Brain Res 88:75–83
Martinez ZA, Ellison GD, Geyer MA, Swerdlow NR (1999) Effects of sustained phencyclidine exposure on sensorimotor gating of startle in rats. Neuropsychopharmacology 21:28–39
Murphy CA, Di Iorio L, Feldon J (2001a) Effects of psychostimulant withdrawal on latent inhibition of conditioned active avoidance and prepulse inhibition of the acoustic startle response. Psychopharmacology (Berl) 156:155–164
Murphy CA, Fend M, Russig H, Feldon J (2001b) Latent inhibition, but not prepulse inhibition, is reduced during withdrawal from an escalating dosage schedule of amphetamine. Behav Neurosci 115:1247–1256
Nelson LR, Ellison G (1978) Enhanced stereotypies after repeated injections but not continuous amphetamines. Neuropharmacology 17:1081–1084
Olney JW, Farber NB (1995) Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry 49:975–982
Phillips M, Wang C, Johnson KM (2001) Pharmacological characterization of locomotor sensitization induced by chronic phencyclidine administration. J Pharmacol Exp Ther 296:905–913
Post RM (1980) Intermittent versus continuous stimulation: effect of time interval on the development of sensitization or tolerance. Life Sci 26:1275–1282
Robinson TE (1984) Behavioural sensitization: characterization of enduring changes in rotational behaviour produced by intermittent injections of amphetamine in male and female rats. Psychopharmacology (Berl) 84:466–475
Robinson TE, Becker JB (1986) Enduring changes in brain and behaviour produced by chronic amphetamine administration: a review and evaluation of animal models of amphetamine psychosis. Brain Res 396:157–198
Russig H, Murphy CA, Feldon J (2002) Clozapine and haloperidol reinstate latent inhibition following its disruption during amphetamine withdrawal. Neuropsychopharmacology 26:765–777
Sato M, Numachi Y, Hamamura T (1992) Relapse of paranoid psychotic state in methamphetamine model in schizophrenia. Schizophr Bull 18:115–122
Scalzo FM, Holson RR (1992) The ontogeny of behavioural sensitization to phencyclidine. Neurotoxicol Teratol 14:7–14
Schroeder U, Schroeder H, Darius J, Grecksch G, Sabel BA (1998) Simulation of psychosis by continuous delivery of phencyclidine from controlled-release polymer implants. Behav Brain Res 97:59–68
Schulz B, Fendt M, Pedersen V, Koch M (2001) Sensitization of prepulse inhibition deficits by repeated administration of dizocilpine. Psychopharmacology (Berl) 156:177–181
Solomon PR, Staton DM (1982) Differential effects of microinjections of d-amphetamine into the nucleus accumbens or the caudate putamen on the rat’s ability to ignore an irrelevant stimulus. Biol Psychiatry 17:743–756
Solomon PR, Crider A, Winkelman JW, Turi A, Kamer RM, Kaplan LJ (1981) Disrupted latent inhibition in the rat with chronic amphetamine or haloperidol-induced supersensitivity: relationship to schizophrenic attention disorder. Biol Psychiatry 16:519–537
Srisurapanont M, Ali R, Marsden J, Sunga A, Wada K, Monteiro M (2003) Psychotic symptoms in methamphetamine psychotic in-patients. Int J Neuropsychopharmacol 6:347–352
Tenn CC, Fletcher PJ, Kapur S (2003) Amphetamine-sensitized animals show a sensorimotor gating and neurochemical abnormality similar to that of schizophrenia. Schizophr Res 64:103–114
Tsai G, Coyle JT (2002) Glutamatergic mechanisms in schizophrenia. Annu Rev Pharmacol Toxicol 42:165–179
Turgeon SM, Case LC (2001) The effects of phencyclidine pre-treatment on amphetamine-induced behaviour and c-Fos expression in the rat. Brain Res 888:302–305
Ujike H (2002) Stimulant-induced psychosis and schizophrenia: the role of sensitization. Curr Psychiatry Rep 4:177–184
Warburton EC, Joseph MH, Feldon J, Weiner I, Gray JA (1994) Antagonism of amphetamine-induced disruption of latent inhibition in rats by haloperidol and ondansetron: implications for a possible antipsychotic action of ondansetron. Psychopharmacology (Berl) 114:657–664
Weiner I (2003) The “two-headed” latent inhibition model of schizophrenia: modeling positive and negative symptoms and their treatment. Psychopharmacology (Berl) 169:257–297
Weiner I, Feldon J (1992) Phencyclidine does not disrupt latent inhibition in rats: implications for animal models of schizophrenia. Pharmacol Biochem Behav 42:625–631
Weiner I, Lubow RE, Feldon J (1988) Disruption of latent inhibition by acute administration of low doses of amphetamine. Pharmacol Biochem Behav 30:871–878
Xu X, Domino EF (1994) Phencyclidine-induced behavioural sensitization. Pharmacol Biochem Behav 47:603–608
Acknowledgements
This work was supported by a special initiative grant from the Ontario Mental Health Foundation (OMHF). C.T. was supported by a Research Fellowship from the OMHF. S.K. is supported by a Canadian Research Chair in Schizophrenia and Therapeutic Neuroscience.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tenn, C.C., Kapur, S. & Fletcher, P.J. Sensitization to amphetamine, but not phencyclidine, disrupts prepulse inhibition and latent inhibition. Psychopharmacology 180, 366–376 (2005). https://doi.org/10.1007/s00213-005-2253-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-2253-z